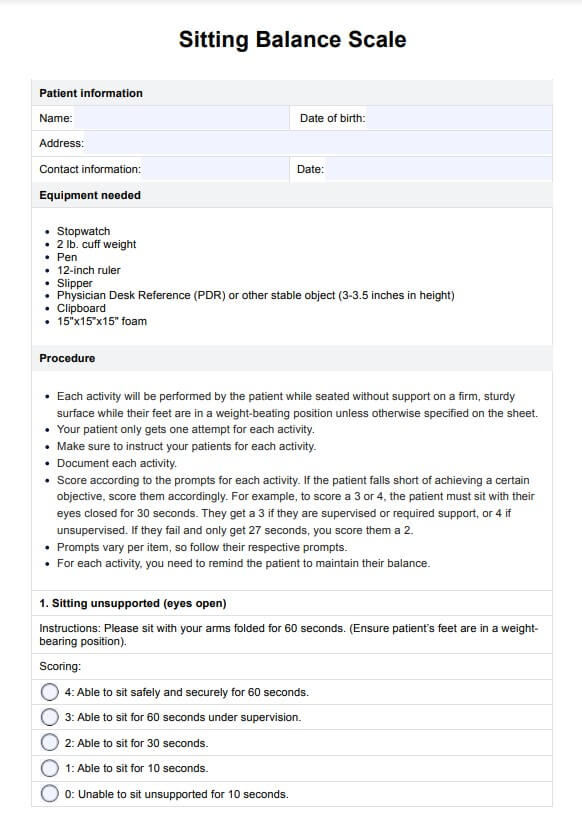
Sitting Balance Scale
Use the Sitting Balance Scale to gauge the capability of mostly non-ambulatory patients to balance themselves while sitting, standing, and moving.


What is the Sitting Balance Scale?
The Sitting Balance Scale (SBS) is a validated tool designed to assess sitting balance in individuals, especially those who are non-ambulatory. This sitting test evaluates balance abilities by scoring a patient's ability to maintain balance while performing tasks such as sitting unsupported, reaching, and transferring. Its primary application is in populations at high fall risk, such as frail or chronically ill patients. The SBS plays a crucial role in measuring sitting balance, providing an objective framework for physical therapists to gauge the need for physical assistance during rehabilitation.
One of the strengths of the SBS lies in its strong correlation with other assessments like the Berg Balance Scale and the Lower Extremity Functional Scale, both widely recognized measures of functional mobility. In physical therapy, the SBS offers a nuanced understanding of balance abilities, contributing significantly to tailored interventions aimed at improving patient outcomes. Its development by Medley and Thompson (2011) has established a benchmark for identifying minimal clinically important differences in balance performance, assisting clinicians in tracking progress or decline. As a result, the SBS has become an essential instrument for identifying impairments in sitting posture, which is critical for reducing fall risk and enhancing patients' overall safety and independence.
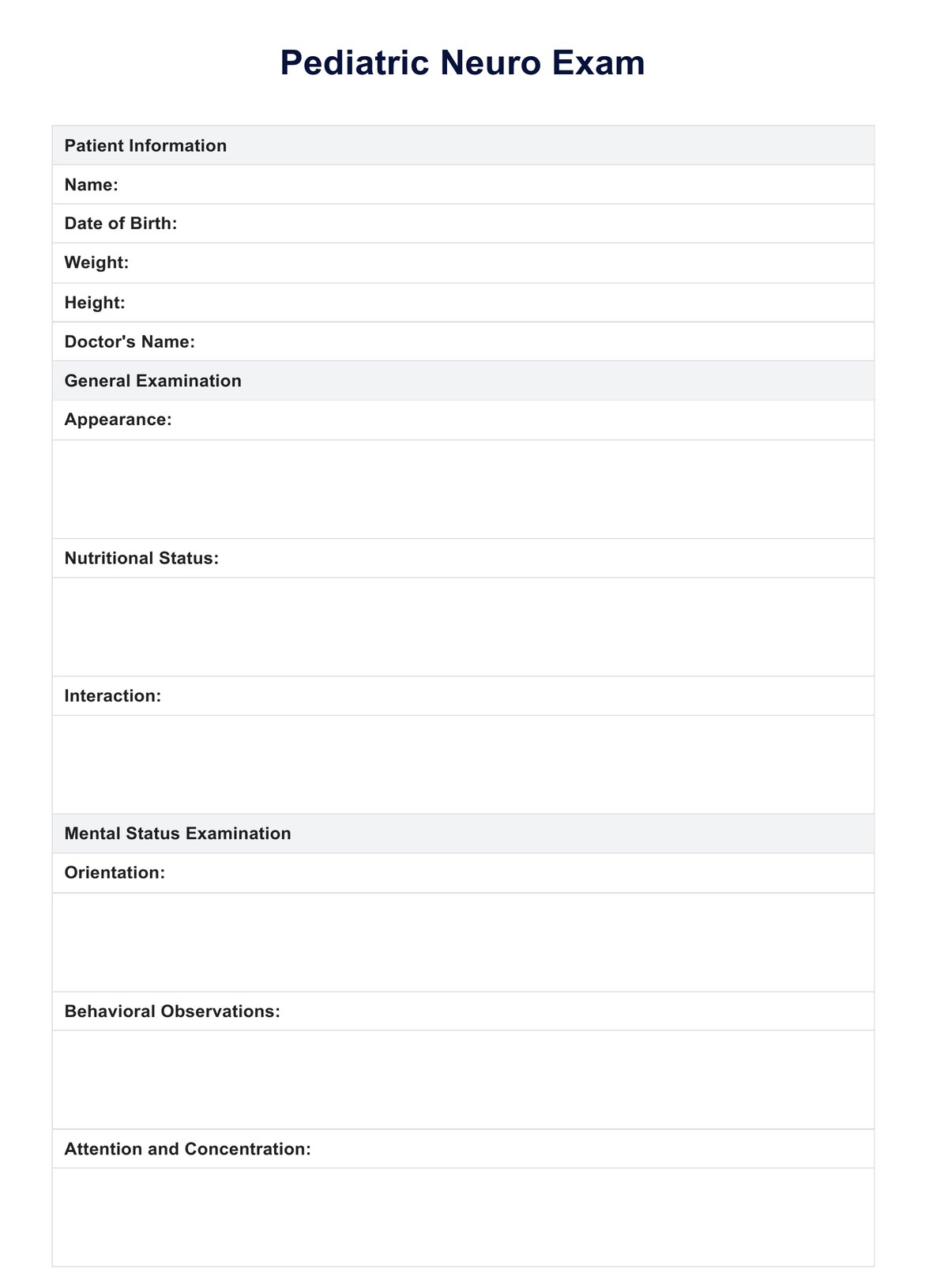
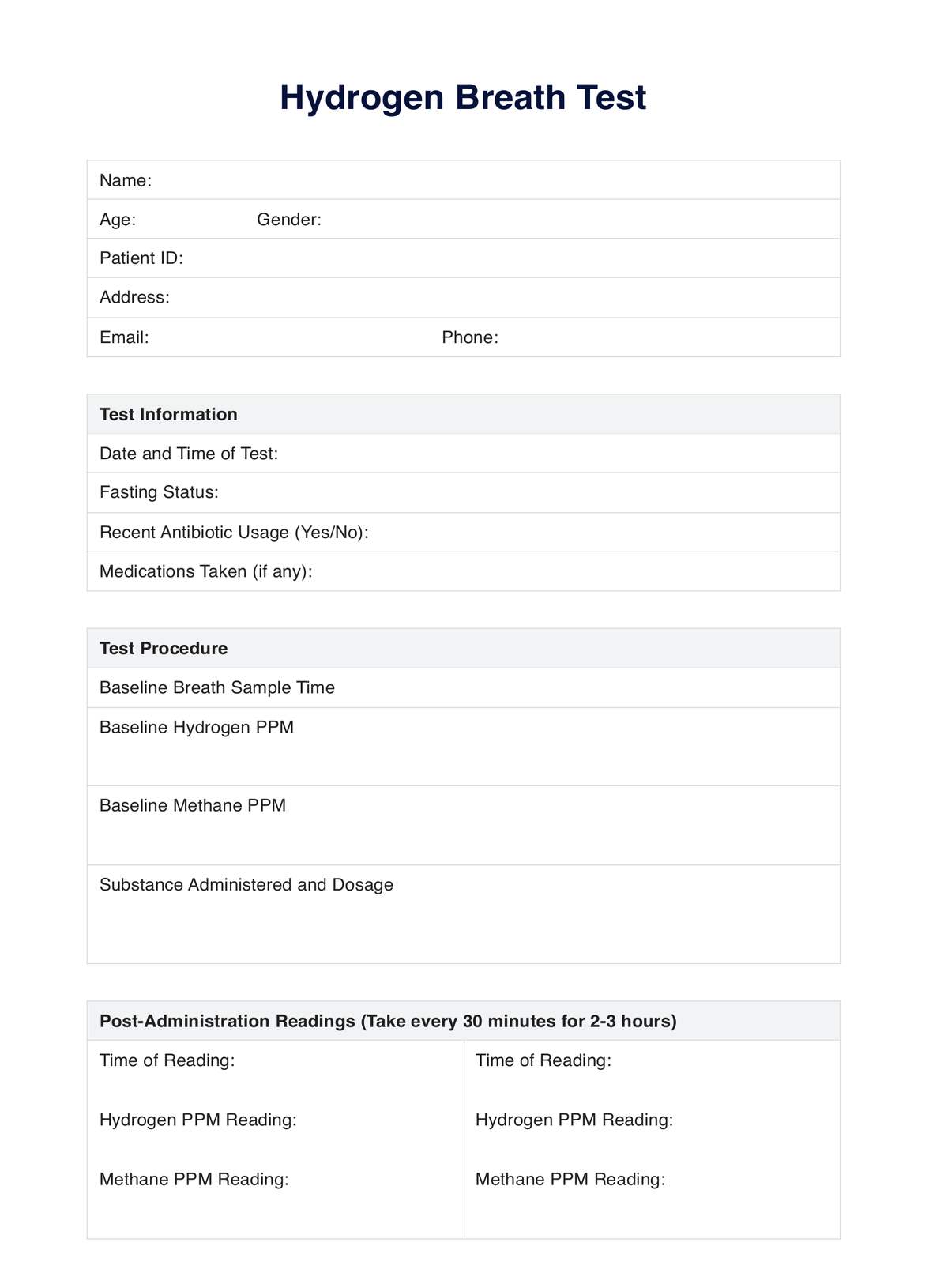
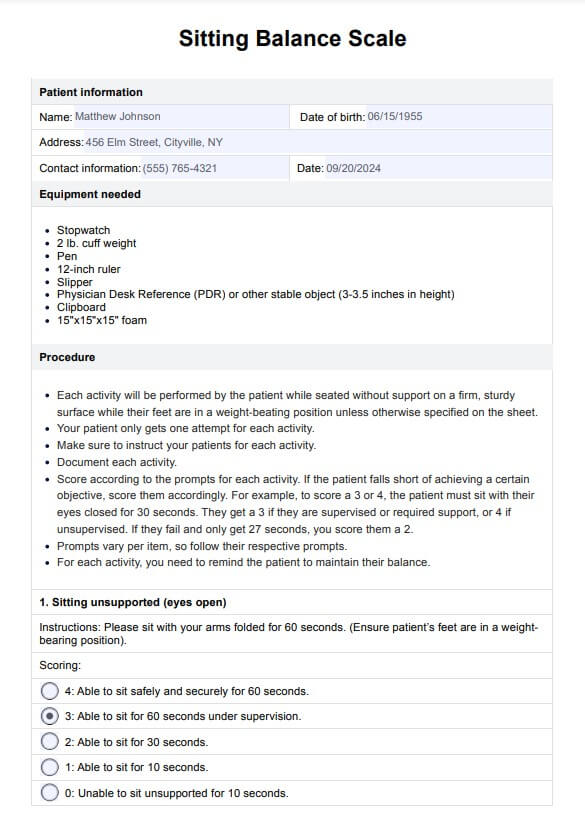
Sitting Balance Scale Template
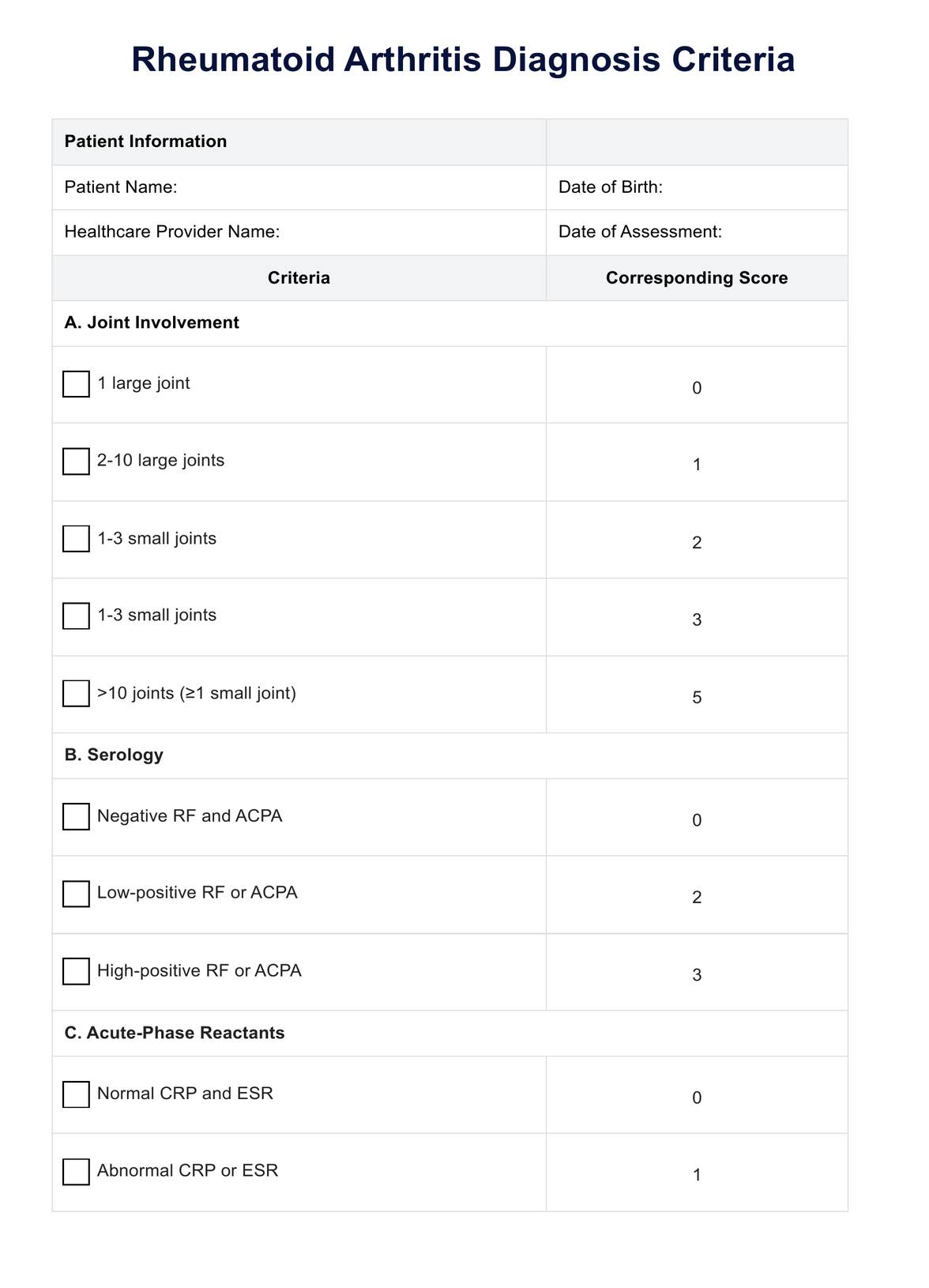
Sitting Balance Scale Example
How to use the Sitting Balance Scale
The Sitting Balance Scale is an effective tool for healthcare providers to assess the ability of a patient to maintain a seated posture during functional tasks. It is commonly used in physical therapy settings, particularly with patients recovering from spinal cord injury or neurological impairments. The SBS can guide practitioners in understanding when physical assistance is needed and help identify the minimal clinically important difference for each patient. Below are the five key steps to effectively use the SBS.
Step 1: Set up the environment
Ensure the patient is seated on a firm surface with their feet flat on the floor. The starting position for each test requires the patient to sit unsupported and maintain posture without losing balance.
Step 2: Provide clear instructions
Instruct the patient on each specific task, ensuring they understand what they need to do. Explain that they should aim to perform task successfully, using their upper extremities only when instructed.
Step 3: Assess and score the tasks
Observe and score the patient's ability to complete task successfully on the 0-4 ordinal scale for each task. Adjust the score if the patient requires minimal assistance or complete assistance.
Step 4: Document physical assistance needed
If complete physical assistance is required during any task, document the level (e.g., moderate assistance) and adjust the score accordingly. Then, assist the patient in completing the task successfully.
Step 5: Analyze outcomes for therapy
Use the SBS scores to tailor physical therapy interventions and determine the minimal clinically important difference that signals improvement or decline in the patient's balance abilities.
When is it best to use the Sitting Balance Scale
The Sitting Balance Scale is primarily used for patients who are mostly non-ambulatory or have difficulty with movement. It is recommended to use this scale when treating such patients. Before using it, it is essential to inform the patient about the scale, as it requires them to perform activities that involve their balance. By assessing balance, the SBS aids in determining the ability of the patient to engage in functional activities and maintain stability during various tasks. Here are the instances or conditions where this scale is necessary:
Acute stroke
Patients recovering from an acute stroke may experience significant balance deficits, making the SBS critical for measuring progress.
Multiple sclerosis
Individuals with multiple sclerosis often face challenges with balance and coordination, necessitating the use of this scale for monitoring functional improvements.
Inpatient rehabilitation
During inpatient rehabilitation, assessing sitting balance is essential for tailoring therapeutic interventions and evaluating outcomes.
Functional assessments
The SBS provides important outcome measures that contribute to the overall clinical relevance of rehabilitation strategies.
Upper extremity rehabilitation
Patients needing upper extremity rehabilitation benefit from assessing their balance while seated, particularly with the outstretched arm test item.
Benefits of using the Sitting Balance Scale
This scale is widely used in physical therapy settings. It helps to identify areas where patients may struggle to complete tasks successfully, ultimately guiding interventions to improve sitting balance and reduce the risk of falls. Here are its benefits:
1. Accurate assessment of sitting balance
The Sitting Balance Scale allows healthcare providers to assess sitting balance systematically. By observing patients in various positions, such as unsupported sitting or reaching forward, the scale identifies specific challenges and limitations that must be addressed. This accuracy is critical for creating individualized treatment plans in physical therapy.
2. Functional task-based evaluation
The scale’s task-oriented nature makes it ideal for evaluating whether a patient can complete tasks successfully in a sitting position. Each task simulates a real-life activity, providing valuable insights into the patient’s ability to perform daily functions safely.
3. Guides physical therapy interventions
As the Sitting Balance Scale highlights areas where patients struggle, it helps healthcare providers design targeted physical therapy interventions. By addressing these specific weaknesses, therapists can improve the patient’s overall stability in a sitting position.
4. Monitors progress over time
By consistently using the Sitting Balance Scale, healthcare providers can track improvements in sitting balance over time. This objective measurement ensures that the interventions are effective and allows adjustments to the therapy plan when necessary.
Reference
Medley, A., & Thompson, M. (2011). Development, reliability, and validity of the Sitting Balance Scale. Physiotherapy Theory and Practice, 27(7), 471–481. https://doi.org/10.3109/09593985.2010.531077
Commonly asked questions
The patient performs tasks like sitting unsupported, reaching forward, and picking up objects. Each task is scored on a 5-point scale, with 0 representing the lowest ability and 4 indicating that the patient can successfully complete tasks confidently in a sitting position.
The Sitting Balance Scale is considered a reliable and valid tool for assessing an individual's seated balance. It effectively measures balance abilities and can predict fall risk. It is correlated with other assessments, such as the Berg Balance Scale and the Lower Extremity Functional Scale. This makes it a valuable instrument for clinicians to assess and monitor balance interventions over time.
The test typically takes about 15-20 minutes, depending on the patient’s ability to complete tasks successfully.
It is primarily used for non-ambulatory patients or those who have difficulty maintaining a stable sitting position. It is adaptable for patients with various conditions, such as frailty, neurological impairments, and balance disorders.






















-template.jpg)