Psych Nurse Report Sheet
Streamline patient care with our comprehensive Psych Nurse Report Sheet, designed for efficient communication and organization. Download now!


What is a Psych Nurse Report Sheet?
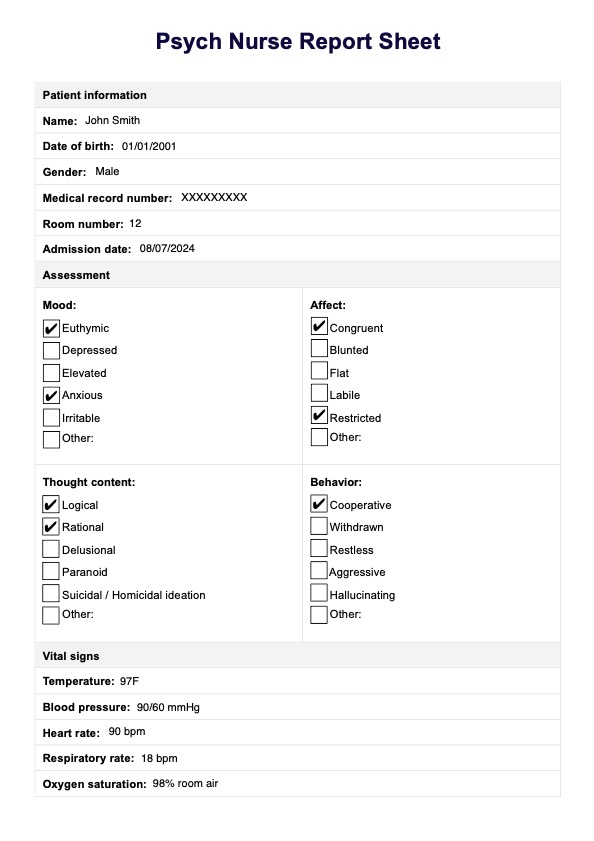
A Psych Nurse Report Sheet, also known as a nursing report sheet or nursing brain sheet, is a document used by nurses, particularly those specializing in mental health, to stay organized and track important patient information during day and night shifts.
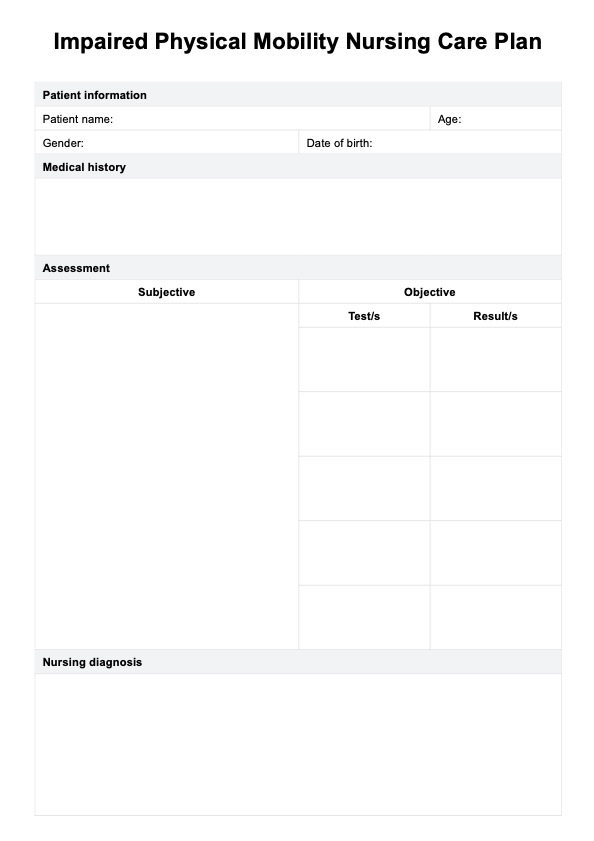
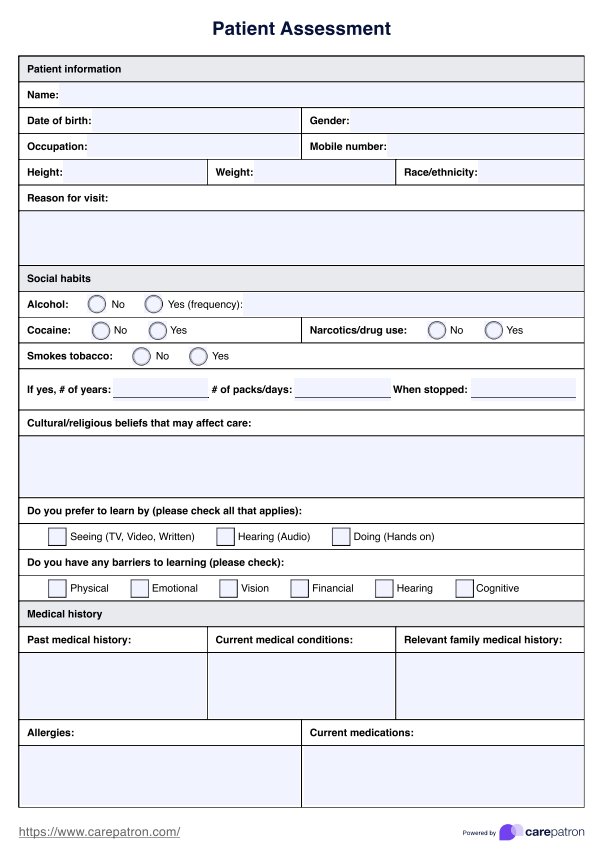
Completing assessments are crucial to mental health nurses and lay the groundwork for specialty care (Coombs et al., 2011). These sheets are crucial for nursing students and experienced nurses in hospitals or other healthcare settings. They typically come in PDF format and contain sections for medical history, patient progress, care plans, medications, precautions, and other relevant details.
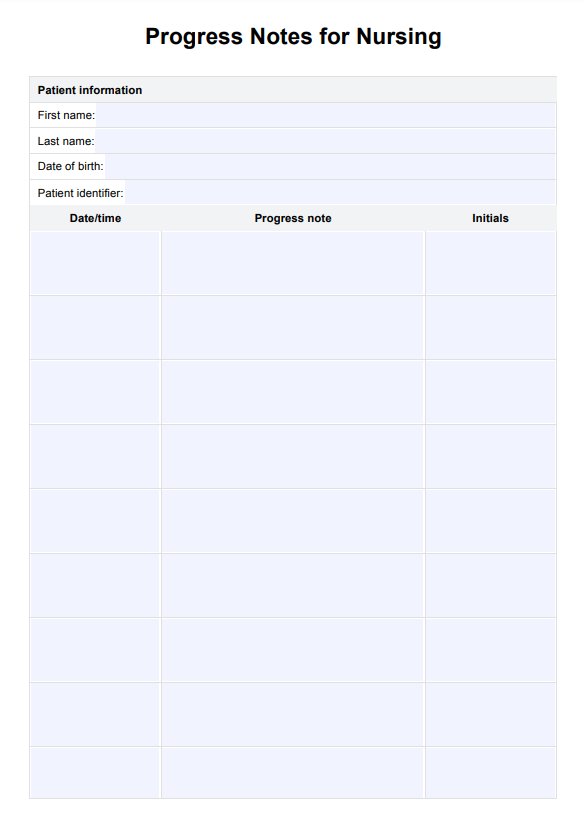
Using a nursing report sheet, nurses can track patient progress, document any changes in condition, and ensure that all critical information is recorded and passed on to the next shift. This helps ensure patient safety and quality of care. This report sheet includes important patient information such as; affect, plans for coping skills, and physical assessment that can support quality care within the mental health workforce (Carniaux Moran, 2008).
Additionally, having a report sheet helps nursing students learn how to organize and prioritize tasks effectively during their clinical rotations. Finally, having a well-organized report sheet saves time and reduces the risk of missing important details.
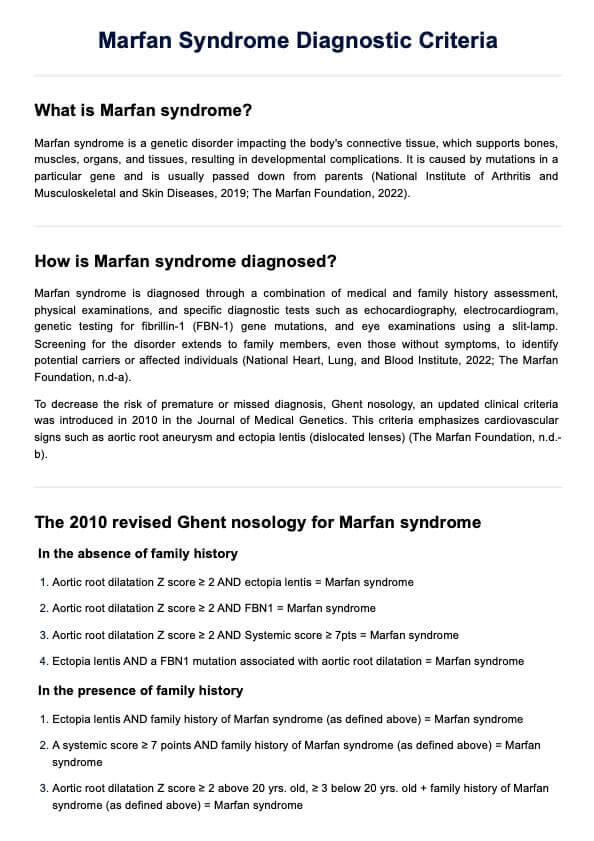
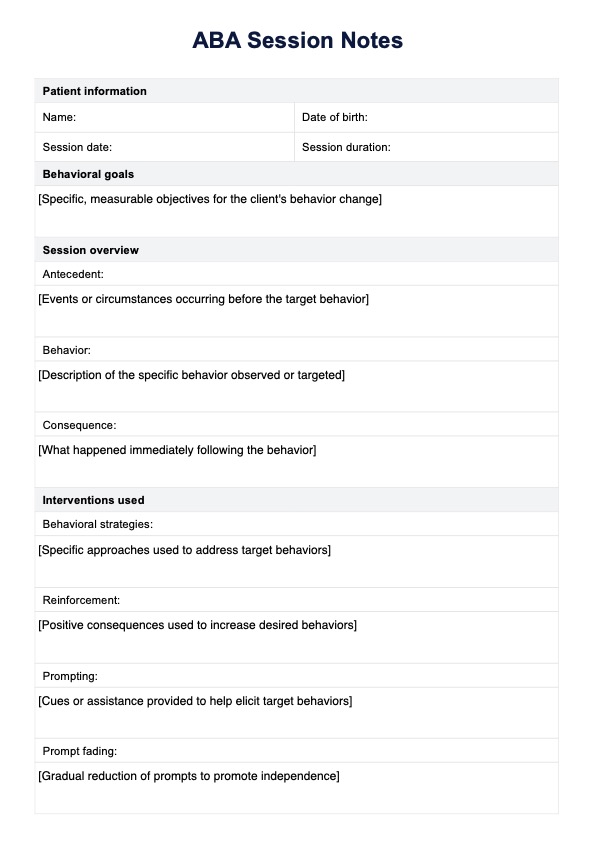
Psych Nurse Report Sheet Template
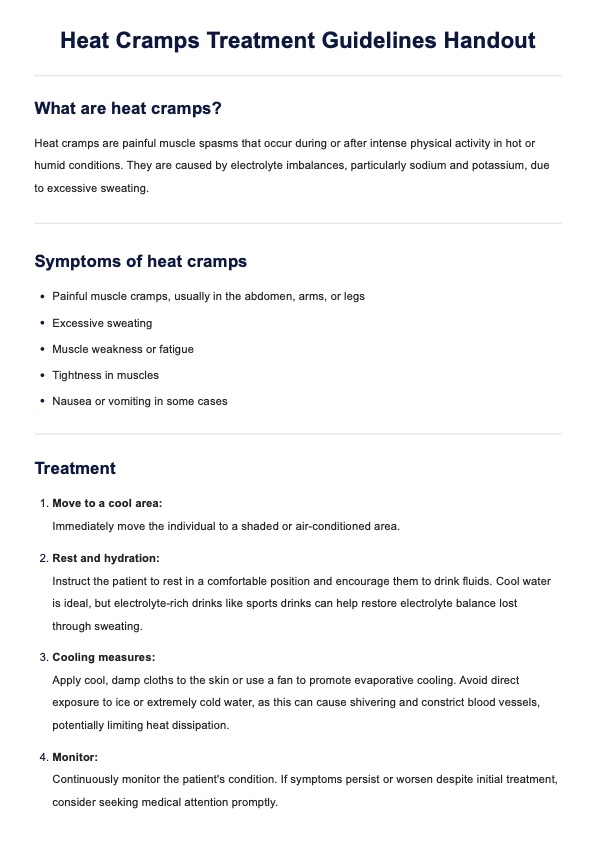
Psych Nurse Report Sheet Example
How does the Psych Nurse Report Sheet work?
Our Psych Report Sheet template is free and easy to use:
Step 1: Access the Psych Nurse Report Sheet
You can access the Psych Nurse Report Sheet through the Carepatron app. Simply download it to your preferred device for online use. Or you can also print this document out for physical use.
Step 2: Complete the report document
Once you have acquired this report sheet, you can complete the document when completing routine assessments. Go through each segment of the report sheet and fill out the sections that you are considering applicable. Every day is different as a practitioner, so you can utilize this document how you see fit.
Step 3: Communicate with other practitioners
You may also use this sheet with other practitioners who may be also caring for your patients. It allows for information to be widely accessed and communicated. Utilize this sheet to support intervention plans and progress reporting later on.
Step 4: Safely store this document
Once you have a completed the Psych Nurse Report Sheet you can store it safely in the Carepatron app. Storing this document can allow all practitioners working within the workplace on assessments to access full documentation notes. This allows your workplace to function more reliably and to it's full capacity.
How does a Psych Nurse Report Sheet differ from a general nursing report sheet?
A Psych Nurse Report Sheet differs from a general or nursing student report sheet in several key ways:
- Focus on mental health: A Psych Nurse Report Sheet is specifically tailored to address the unique needs and considerations of psychiatric or mental health care patients. It emphasizes aspects such as mood assessment, psychiatric symptoms, and safety precautions related to mental health conditions.
- Specialized assessments: While a general nursing report sheet may primarily focus on physical assessments and vital signs, a Psych Nurse Report Sheet includes specialized evaluations related to mental health, such as mood, affect, thought content, and risk of harm to self or others.
- Psychotropic medications: The medication section of a Psych Nurse Report Sheet typically includes a greater emphasis on psychotropic medications used to manage psychiatric symptoms, such as antidepressants, antipsychotics, mood stabilizers, and anxiolytics.
- Safety precautions: Due to the unique risks associated with psychiatric conditions, a Psych Nurse Report Sheet often includes specific safety precautions, such as suicide risk assessments, precautions for patients with aggressive behaviors, or protocols for managing patients at risk of elopement.
- Therapeutic interventions: In addition to traditional nursing interventions, a Psych Nurse Report Sheet may document therapeutic interventions specific to psychiatric care, such as cognitive-behavioral techniques, psychoeducation, or group therapy sessions.
- Communication and collaboration: Given the interdisciplinary nature of psychiatric care, a Psych Nurse Report Sheet may facilitate enhanced communication and collaboration with other members of the mental health team, such as psychiatrists, psychologists, social workers, and occupational therapists.
Benefits of utilizing a Psych Nurse Report Sheet
Improving patient care and communication with a Psych Nurse Report Sheet involves several vital strategies:
Enhanced documentation
The structured format of the report sheet facilitates comprehensive documentation of patient assessments, interventions, and outcomes. This ensures that important information is captured accurately, promoting continuity of care and informed decision-making by healthcare providers.
Promoting collaboration
A report sheet is a communication tool among healthcare team members, facilitating cooperation and care coordination. Providing a centralized platform for sharing information fosters interdisciplinary communication and teamwork, ultimately enhancing patient care outcomes.
Facilitating handovers
The report sheet enables nurses to convey critical patient information to the incoming nursing staff during shift changes. This ensures that important details about the patient's condition, care plan, and any pending tasks are communicated effectively, minimizing the risk of errors and providing seamless transitions in care.
Identifying trends and patterns
By systematically documenting patient data over time, the report sheet allows nurses to identify trends and patterns in the patient's condition. This enables proactive interventions and adjustments to the care plan, promoting timely and targeted interventions to address evolving patient needs.
Empowering patient engagement
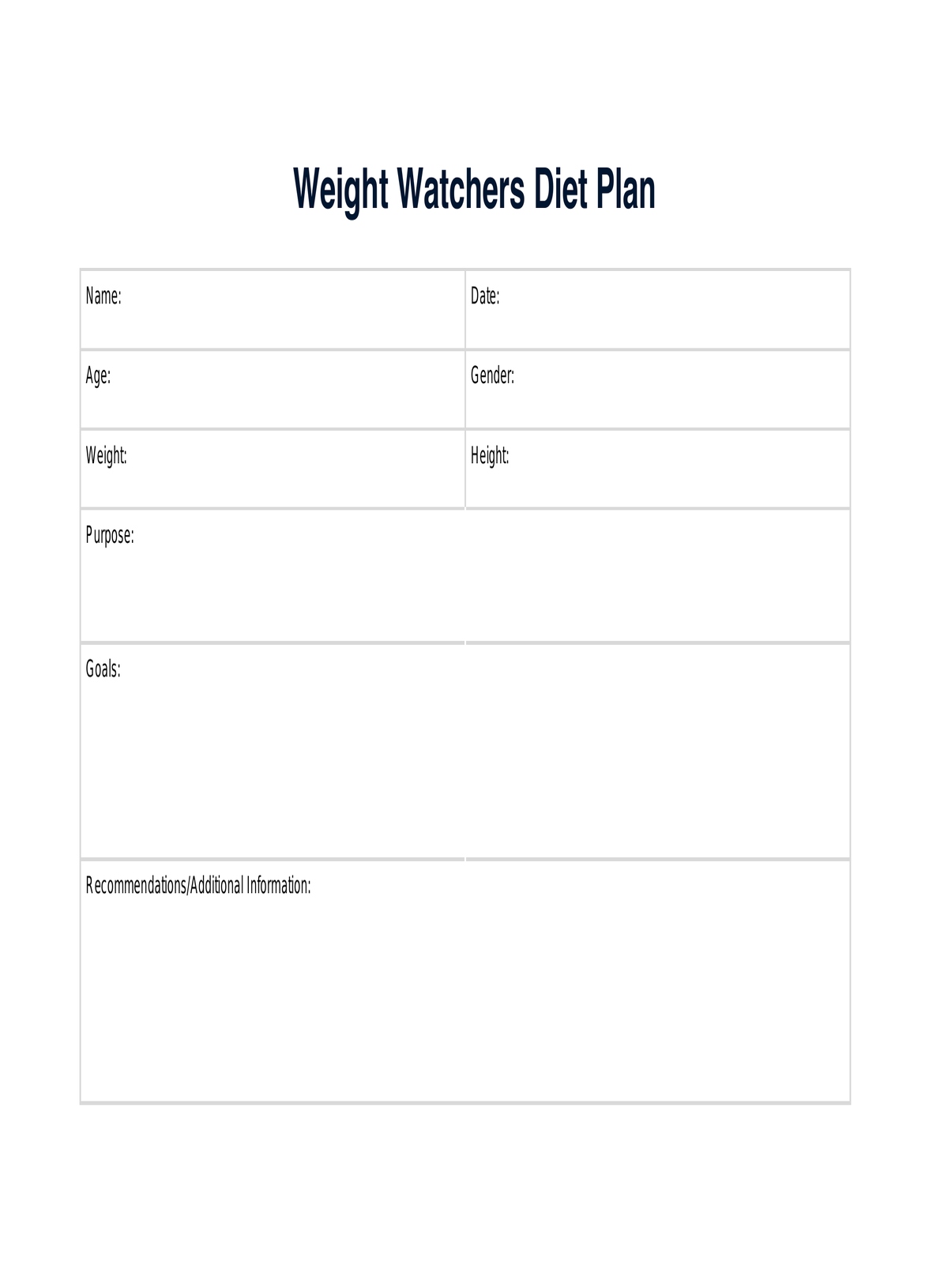
The report sheet can also be valuable for engaging patients in their care. Nurses can use the information documented on the report sheet to educate patients about their treatment plan, goals, and progress, empowering them to participate actively in decision-making and self-management of their mental health.
Quality improvement initiatives
Data collected through the report sheet can be used for quality improvement initiatives within the healthcare facility. By analyzing trends in patient outcomes, resource utilization, and adherence to best practices, healthcare providers can identify areas for improvement and implement strategies to enhance the quality and efficiency of care delivery.
References
Carniaux Moran, C. (2008). The psychiatric nursing assessment. In Psychiatric mental health nursing: An introduction to theory and practice (pp. 41–43).
Coombs, T., Curtis, J., & Crookes, P. (2011). What is a comprehensive mental health nursing assessment? A review of the literature. International Journal of Mental Health Nursing, 20(5), 364–370. https://doi.org/10.1111/j.1447-0349.2011.00742.x
Commonly asked questions
Document psychiatric nursing notes by recording observations, assessments, interventions, and patient responses in a structured format. Include relevant details such as mood, affect, behavior, vital signs, and any safety concerns or changes in mental status.
Write a nursing report by providing a concise summary of the patient's condition, including assessments, interventions, and responses to treatment. Use a systematic approach, focusing on critical information such as vital signs, medications, care plans, and any significant events or changes in the patient's status.
The Mental Status Examination (MSE) is the most critical assessment tool for the psychiatric nurse. It evaluates vital aspects of the patient's mental health, including mood, affect, thought content, perception, cognition, and insight, providing valuable insights into the patient's overall mental status and functioning.