Rheumatoid Arthritis Diagnosis Criteria
Learn about the essential Rheumatoid Arthritis Diagnosis Criteria for accurate identification and timely treatment in healthcare.


What is rheumatoid arthritis (RA)?
Rheumatoid arthritis (RA) is an inflammatory arthritis, a chronic disease affecting joints. It causes joint inflammation, pain, and stiffness. Early rheumatoid arthritis may manifest as joint symptoms like swelling and tenderness. Diagnosing rheumatoid arthritis involves assessing joint involvement and considering factors like rheumatoid factor and inflammatory markers. Treating rheumatoid arthritis typically involves a combination of medication and lifestyle changes to manage symptoms and prevent joint damage.
It is crucial to distinguish RA from other conditions like systemic lupus erythematosus or inflammatory bowel disease, as the treatment approach may differ. Additionally, individuals with psoriatic arthritis or reactive arthritis may exhibit similar joint symptoms. Rheumatoid nodules, another characteristic feature, may develop in some cases.
Early detection and intervention are crucial for effectively managing rheumatoid arthritis and improving quality of life.
Symptoms
Rheumatoid arthritis (RA) is a multifaceted disease with symptoms that impact patients differently. Accurate identification of these symptoms is crucial for diagnosis and determining the best course of action:
- Joint swelling: Characterized by enlargement that makes joints appear bigger and feel warm and tender to the touch.
- Swollen joints: Increased size or puffiness in larger joints, such as knees and elbows, leading to restricted movement and discomfort.
- Active rheumatoid arthritis: Ongoing joint pain and inflammation marked by stiffness, fatigue, and increased discomfort during flare-ups.
- Large joint symptoms: Inflammation and potential mobility impairment in weight-bearing joints like the hips and shoulders.
- Distal interphalangeal joint involvement: Stiffness and swelling in the joints at the tips of fingers and toes may lead to deformities.
- Inflammatory joint disease: Pain, stiffness, and a decreased range of motion in the affected joints, often accompanied by redness and warmth.
- Joint destruction: Long-term RA can cause joint damage, visible as erosion and deformity, which indicates advanced disease progression.
Healthcare providers need to recognize these symptoms promptly to slow the disease's progression and help maintain their patients' quality of life. Regular monitoring and adapting treatment approaches based on the progression of these symptoms are vital in the effective management of RA.
Risk factors and causes of rheumatoid arthritis
Rheumatoid arthritis (RA) develops from genetic, lifestyle, and environmental factors. Understanding these can help in prevention and targeted treatment:
- Genetic factors: Individuals with a family history of RA are at a higher risk, indicating a genetic predisposition to the disease.
- Lifestyle choices: Smoking significantly increases the risk of developing RA and can exacerbate its severity.
- Environmental exposures: Exposure to substances like silica and asbestos, especially in specific workplaces, is linked to an elevated risk of RA.
The causes of RA involve complex interactions within the body:
- Autoimmune reaction: An improper immune response leads to inflammation in the synovium, the lining of the joints, which is characteristic of RA.
- Genetic and environmental interaction: The disease often results from genetic susceptibility and environmental triggers.
As noted by Wasserman (2011), these factors collectively contribute to the risk and development of RA, emphasizing the importance of a comprehensive understanding for effective management.
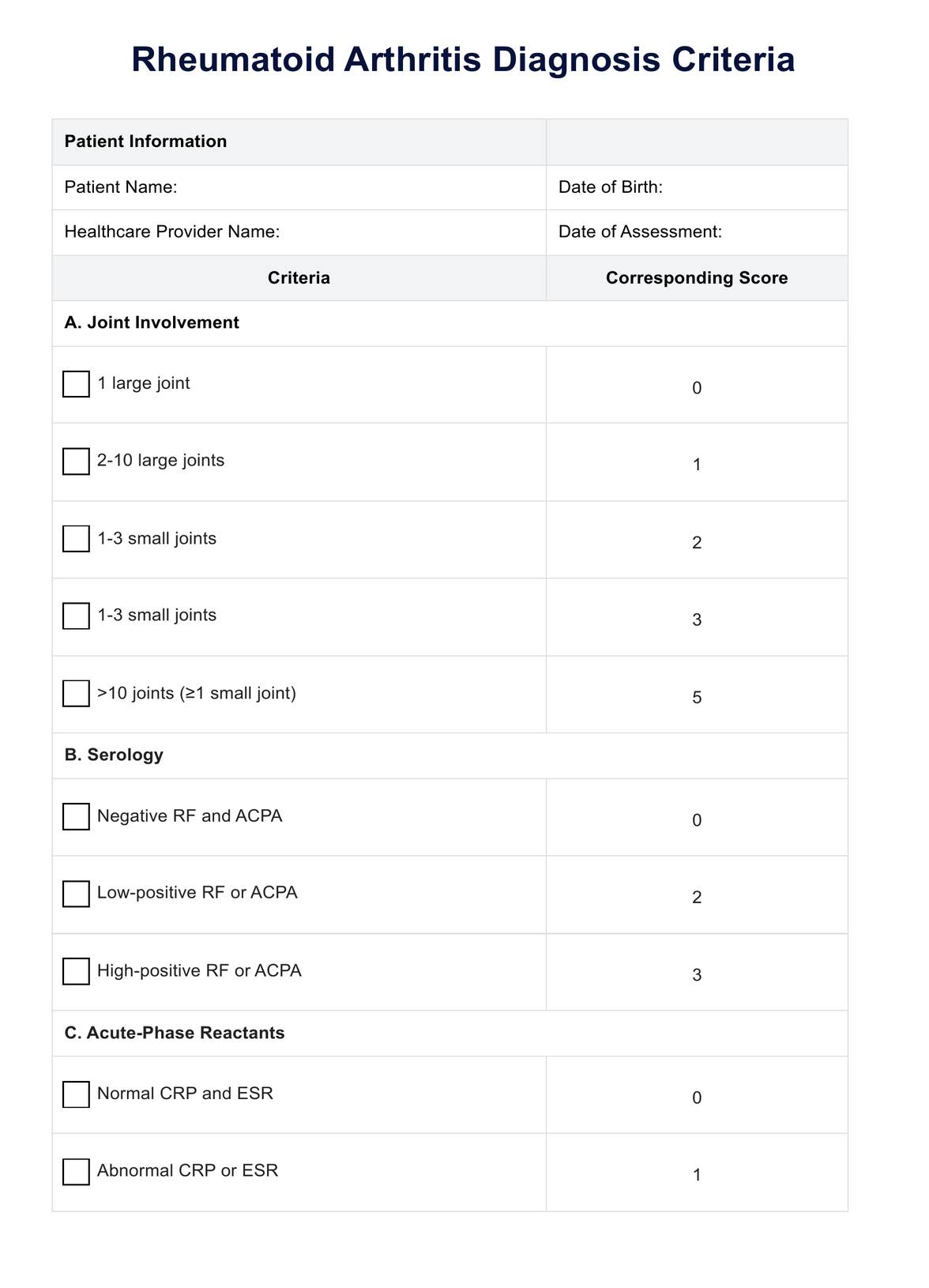
Rheumatoid Arthritis Diagnosis Criteria Template
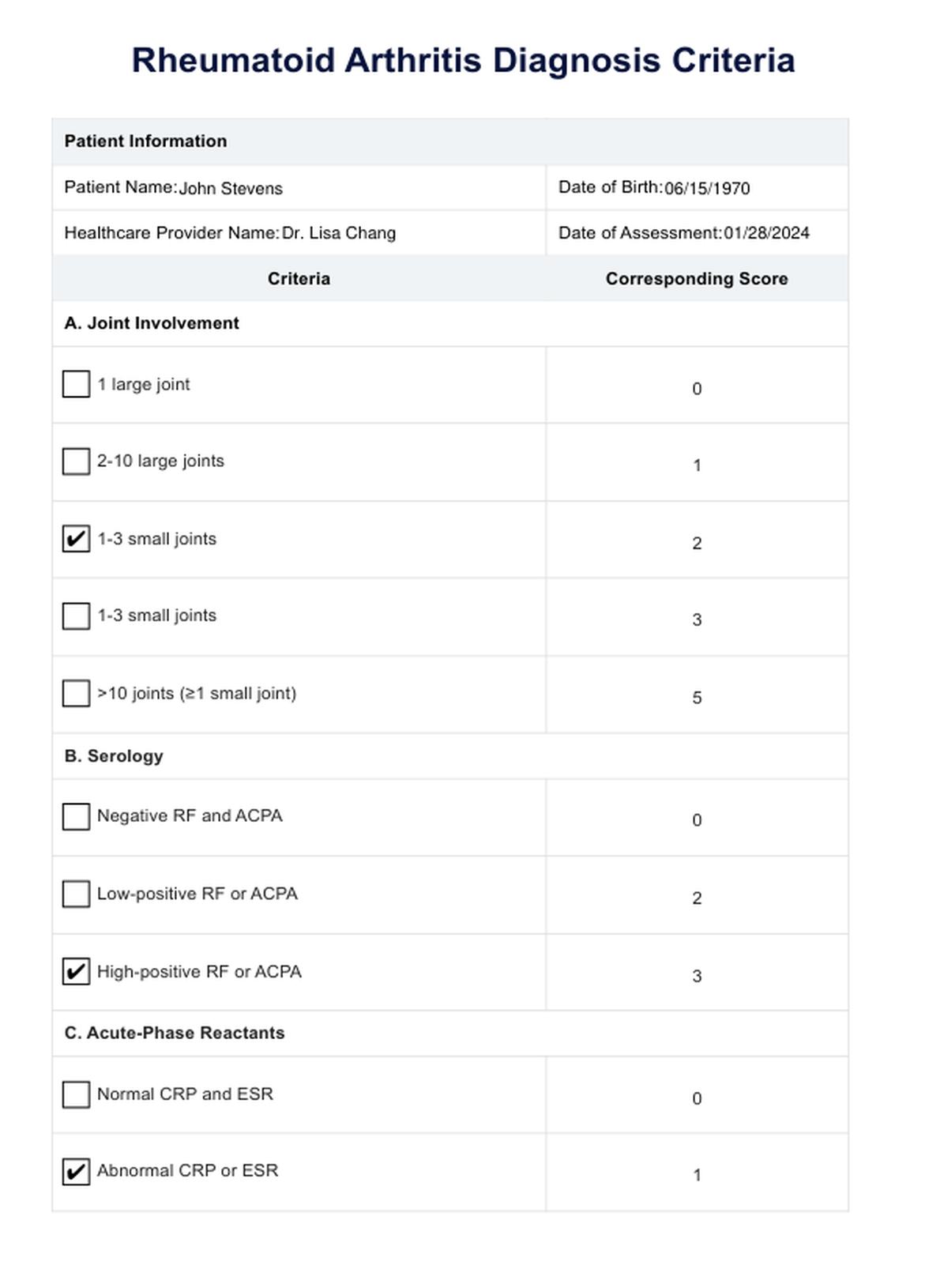
Rheumatoid Arthritis Diagnosis Criteria Example
How is rheumatoid arthritis diagnosed?
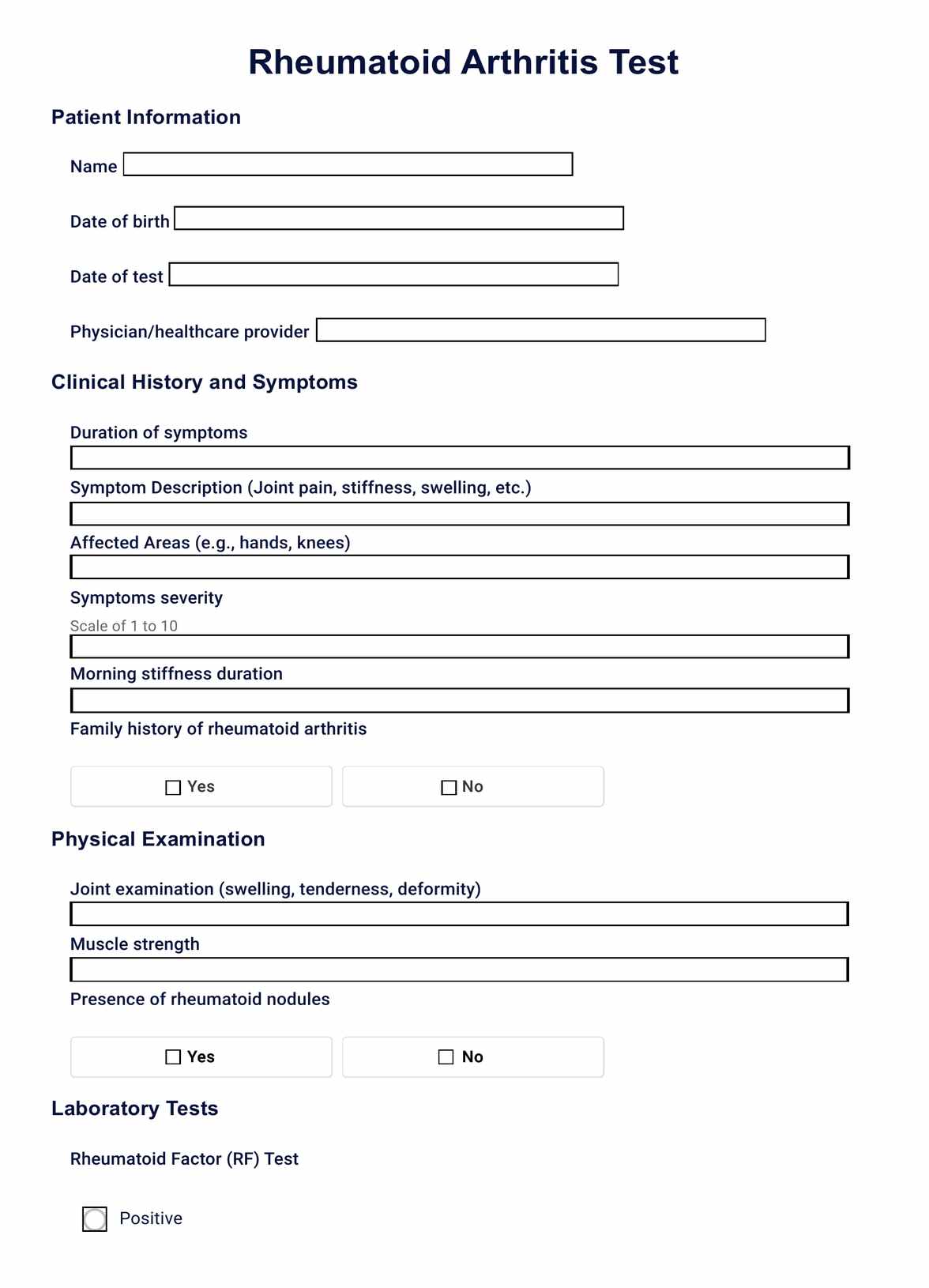
Diagnosing rheumatoid arthritis (RA) involves assessing various clinical presentations, utilizing diagnostic criteria, and conducting specific tests:
Typical presentation
Patients with RA commonly experience pain and stiffness in multiple joints, notably the wrists, proximal interphalangeal joints, and metacarpophalangeal joints. Morning stiffness over an hour indicates inflammatory etiology, often accompanied by visible synovitis or palpable synovial thickening. Indolent arthralgias may precede joint swelling and systemic symptoms like fatigue, weight loss, and low-grade fever.
Diagnostic criteria
Wasserman (2011) of the American College of Rheumatology and the European League Against Rheumatism developed newly updated classification criteria for RA. These standards enable early diagnosis even in patients who did not fit the earlier classification standards. Early asymmetric presentation is possible because symmetric arthritis is not necessary. These criteria, based on the work of Aletaha et al., facilitate the early identification of RA and allow for prompt initiation of treatment interventions to improve patient outcomes.
Diagnostic tests
Autoantibodies such as rheumatoid factor and anti-citrullinated protein antibodies aid in diagnosis. Elevated C-reactive protein and erythrocyte sedimentation rate indicate active RA and are part of the new classification criteria. A baseline complete blood count, renal and hepatic function assessment, and radiography of hands and feet are also conducted to evaluate disease activity and influence treatment options.
Differential diagnosis
Skin findings may suggest other conditions like systemic lupus erythematosus or psoriatic arthritis. Polymyalgia rheumatica should be considered in older patients with shoulder and hip symptoms. Inflammatory back symptoms may indicate spondyloarthropathy, while recurrent acute joint swelling suggests crystal arthropathy. Fibromyalgia can coexist with RA and should be considered during diagnosis.
What are the diagnostic criteria for rheumatoid arthritis?
Rheumatoid arthritis (RA) is a chronic autoimmune disease primarily affecting the joints and can lead to severe inflammation, pain, and potential joint damage if not properly managed. Timely and accurate diagnosis is crucial for effective treatment. According to Wasserman (2011), the diagnosis of RA involves a comprehensive set of criteria that includes clinical, serological, and imaging assessments to help healthcare providers identify and manage this condition.
The simplified diagnostic criteria provided by Carepatron for RA include the following key points:
- Joint involvement: It's essential to check for swelling or tenderness in multiple joints, focusing on smaller joints such as those in the hands and feet.
- Duration of symptoms: Symptoms must persist for at least six weeks to meet the RA diagnostic criteria.
- Morning stiffness: A hallmark of RA, morning stiffness should last at least one hour.
- Serology: Tests for rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP) antibodies are crucial, although negative results do not rule out RA.
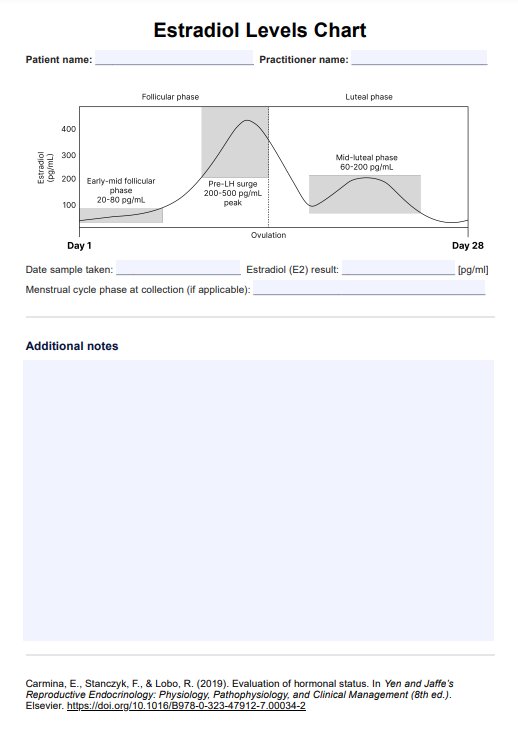
- Acute-phase reactants: Elevated levels of C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) may suggest RA, but these markers are not exclusive to the disease.
- Radiographic changes: X-rays might show changes typical of RA, but such changes may not be apparent early in the disease.
- Exclusion of other diagnoses: Accurate diagnosis requires ruling out other conditions that could mimic RA symptoms.
By following these criteria, healthcare providers can more effectively diagnose rheumatoid arthritis and commence appropriate treatment strategies to manage the disease and improve patient outcomes.
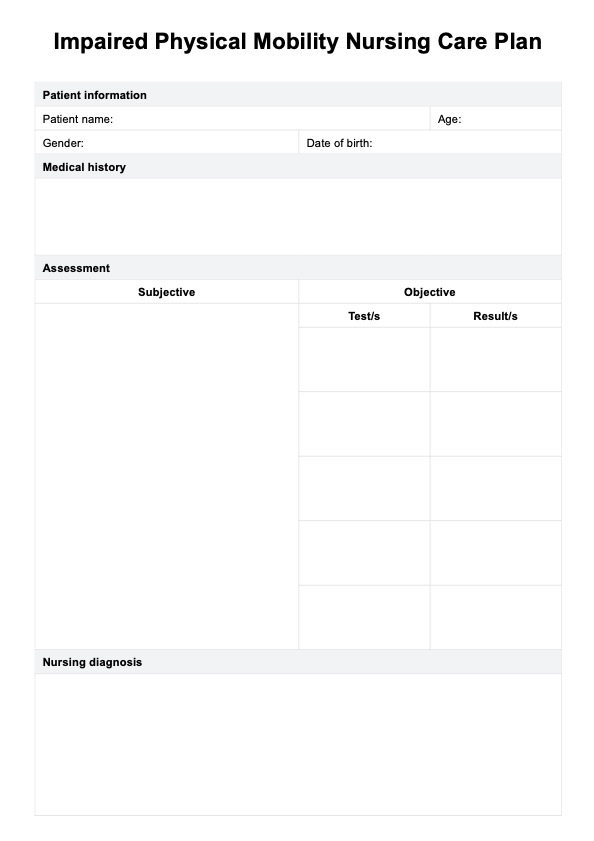
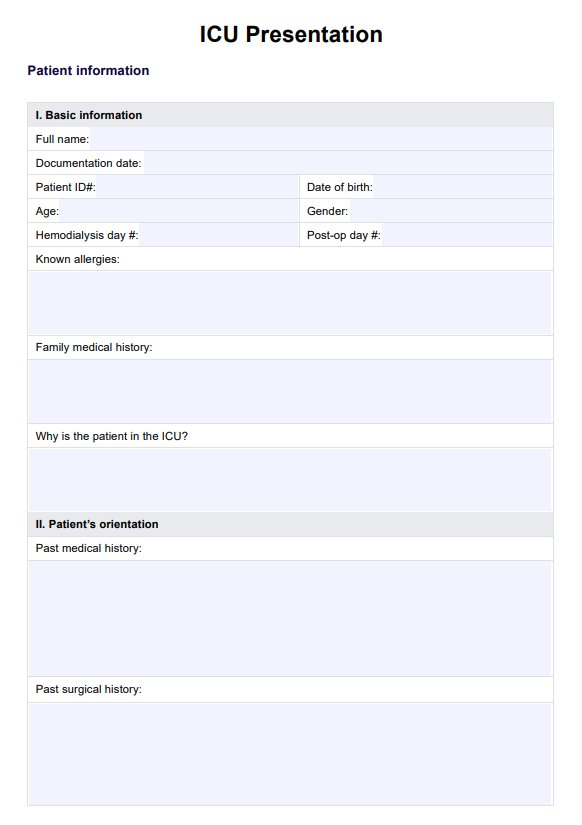
How does our Rheumatoid Arthritis Diagnosis Criteria template work?
RA is a complex autoimmune disease that requires careful evaluation and diagnosis to initiate appropriate treatment. Our Rheumatoid Arthritis Diagnosis Criteria template provides healthcare experts with a structured approach to assessing patients for possible RA and guiding clinical decision-making.
Here is how it works:
Step 1: Assessment
Healthcare professionals begin by assessing the patient's signs and symptoms, focusing on key indicators such as joint pain, swelling, stiffness, and systemic symptoms like fatigue or fever. This comprehensive evaluation forms the basis for determining the likelihood of RA.
Step 2: Completing the template
Using our template, healthcare providers systematically document the presence or absence of specific criteria outlined in the ACR/EULAR 2010 Rheumatoid Arthritis Classification Criteria. These criteria include joint involvement, serology, acute-phase reactants, and duration of symptoms.
Step 3: Joint involvement
Healthcare providers select the appropriate options for joint involvement based on the number and size of affected joints, excluding certain joints like distal interphalangeal (DIP) joints.
Step 4: Serology
The template guides healthcare professionals in evaluating serological markers such as rheumatoid factor and anti-citrullinated protein antibody, categorizing results as negative, low-positive, or high-positive.
Step 5: Acute-phase reactants
Healthcare providers indicate the patient's levels of acute-phase reactants, such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), as normal or abnormal based on laboratory reference ranges.
Step 6: Duration of symptoms
Finally, healthcare professionals assess the duration of symptoms reported by the patient, distinguishing between symptoms lasting less than six weeks and those persisting for six weeks or longer.
Step 7: Interpretation
Once all criteria are completed, healthcare providers interpret the results to determine the likelihood of RA diagnosis based on the cumulative points assigned according to the template.
By systematically following these steps, healthcare providers can effectively identify and diagnose RA, allowing for timely initiation of appropriate treatment and improved patient outcomes.
Treating rheumatoid arthritis
Effective management of rheumatoid arthritis (RA) involves a comprehensive approach to alleviate symptoms, slow disease progression, and enhance the quality of life. This approach integrates pharmacological treatments, nonpharmacological therapies, lifestyle modifications, and potential surgical interventions, following guidelines established by the American College of Rheumatology and the European League Against Rheumatism, as highlighted in various AAFP publications.
Medications
RA medications aim to control symptoms and modify the disease course. Here are the primary types used:
- Disease-modifying antirheumatic drugs (DMARDs) such as methotrexate, hydroxychloroquine, and sulfasalazine are foundational in RA treatment, aiming to suppress inflammation and prevent joint damage.
- Biologic agents, including tumor necrosis factor (TNF) inhibitors like adalimumab and infliximab, as well as other targeted therapies such as rituximab and tocilizumab, are reserved for patients who do not adequately respond to conventional DMARDs.
- Corticosteroids are used for rapid symptom relief during flare-ups but are generally limited in duration due to potential long-term adverse effects.
Nonpharmacologic therapies
These therapies complement medical treatments by improving physical function and reducing stress on affected joints:
- Physical and occupational therapy enhances joint function, range of motion, and mobility.
- Assistive devices, such as splints and braces, support joints and reduce pain.
- Regular exercise, particularly low-impact activities like swimming or cycling, maintains joint flexibility and muscle strength.
- Heat and cold therapy are simple measures to reduce pain and inflammation.
Lifestyle modifications
Lifestyle changes can significantly impact the management of RA, focusing on overall health and symptom control:
- Weight management is critical in reducing stress on joints and improving function.
- An anti-inflammatory diet with fruits, vegetables, and omega-3 fatty acids can help control symptoms.
- Smoking cessation is crucial as smoking exacerbates disease activity and diminishes treatment efficacy.
Surgical interventions
For severe cases where joint damage significantly impairs quality of life, surgery might be considered. In cases of advanced joint damage, surgical procedures like joint replacement (arthroplasty) may be necessary to restore function and relieve pain.
Treatment strategies for RA are tailored to individual patient needs, considering the severity of the disease, response to previous treatments, and personal preferences. Continuous monitoring and close collaboration between patients and healthcare providers are crucial to adapting treatment plans and achieving optimal outcomes.
References
Aletaha, D., Neogi, T., Silman, A. J., Funovits, J., Felson, D. T., Bingham, C. O., Birnbaum, N. S., & Burmester, G. R. (2010). 2010 Rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis & Rheumatism, 62(9), 2569–2581. https://doi.org/10.1002/art.27584
Wasserman, A. M. (2011). Diagnosis and Management of Rheumatoid Arthritis. American Family Physician, 84(11), 1245–1252. https://www.aafp.org/pubs/afp/issues/2011/1201/p1245.html
Commonly asked questions
Currently, there is no cure for RA, but early diagnosis and aggressive treatment can help manage symptoms, slow disease progression, and improve quality of life.
Yes, RA is a systemic disease that can affect organs and systems beyond the joints, leading to complications such as rheumatoid nodules, cardiovascular disease, lung involvement, and osteoporosis.
Lifestyle changes like maintaining a healthy diet, regular exercise, stress management, and smoking cessation can help manage RA symptoms and improve overall well-being.