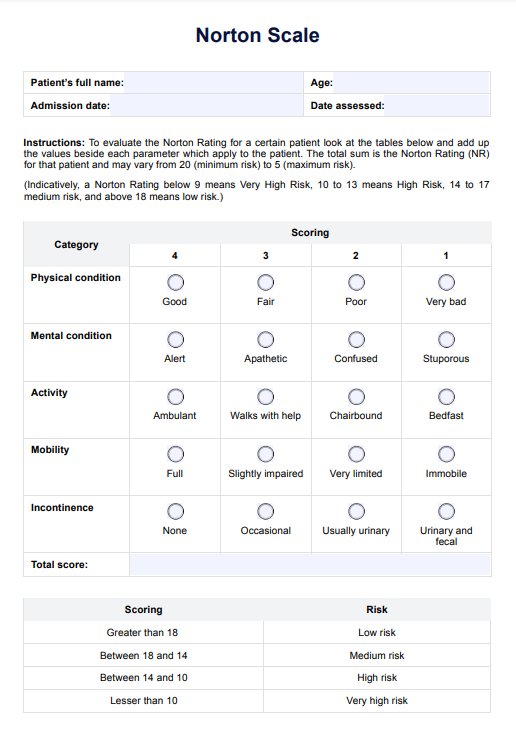
The Norton Scale assesses an adult's risk of developing a pressure ulcer by evaluating five categories: physical condition, mental condition, activity, mobility, and incontinence.
Norton Scale
Learn about the Norton Scale, a tool used in healthcare to assess the risk of pressure ulcers. Understand its significance and application through this guide!
Use Template
Norton Scale Template
Commonly asked questions
The Norton Scale assigns a score of 1-4 for each category based on the individual's condition. Lower scores indicate a higher risk of developing bedsores. Generally, individuals scoring 14 or less are considered at risk.
Norton Scale scores categorize individuals into risk levels: a score above 18 indicates low risk, 18-14 indicates medium risk, 13-10 indicates high risk, and a risk score below 10 indicates very high risk.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











