Return To Work Doctors Note
Return To Work Doctors Note Template provides an easy-to-use form when you are ready to return to work after time off due to sickness or injury.


What is a Return To Work Doctors Note Template?
A return to work doctor's note is a formal medical document written by a healthcare provider, typically a physician or nurse practitioner, to allow an employee to resume job duties after a period of illness, injury, or other medical leave.
This note verifies that the employee is medically fit to return to work and can perform their essential job functions without limitations or restrictions. It also provides the employer with information about any necessary accommodations or modifications that may be required to support the employee's successful return to work.
Return To Work Doctors Note Template
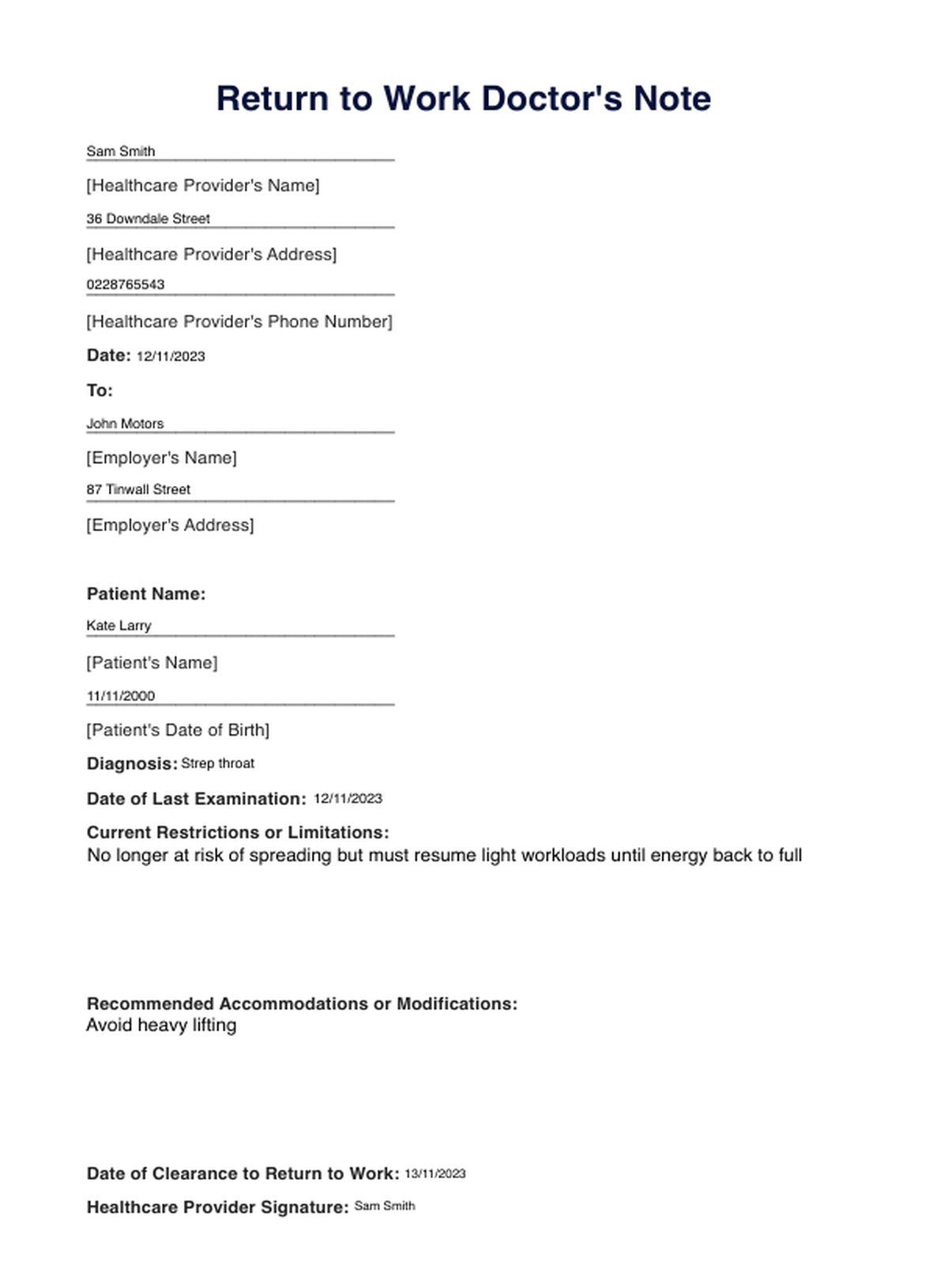
Return To Work Doctors Note Example
How does this template work?
When filling out a printable Return to Work Doctors Note Template, the main steps include the following:
- The healthcare provider schedules an appointment with the employee to discuss their medical condition, recovery progress, and any concerns or limitations they may have regarding returning to work.
- The healthcare provider then conducts a thorough medical examination, reviewing the patient's medical history, current symptoms, and any relevant test results.
- Through a functional assessment, the healthcare provider may evaluate the patient's physical abilities, cognitive function, and overall fitness to perform their job duties safely.
- The healthcare provider discusses the employee's job's specific requirements and physical demands.
- Based on the assessment findings and job demands, the healthcare provider determines whether the employee is medically fit to return to work and provides specific recommendations for accommodations or modifications, if necessary.
- The healthcare provider completes the return to work doctor's note, documenting the assessment findings, recommendations, and clearance date.
- The employee provides the completed note to their employer, who may review it with their human resources department to determine appropriate accommodations or modifications.
When would you use this template?
- When an employee has been absent from work due to an illness or injury, a doctor's note is often required to confirm their medical clearance to return to work and ensure they are physically and mentally fit to perform their job duties without limitations.
- Following surgery or other medical procedures that may require recovery, a doctor's note can provide legal documentation of the employee's readiness to resume work and identify any necessary restrictions or accommodations.
- When an employee has been on disability leave due to a health condition, a doctor's note can update their medical status and confirm their ability to return to work, potentially with specific accommodations or limitations.
- If there is any ambiguity or concern about an employee's fitness to resume their job duties, a doctor's note can provide an objective medical assessment and clarify any limitations or accommodations that may be required.
- Return to work doctor's notes are the official documentation of an employee's medical clearance and any necessary accommodations, which can be helpful for employer records and health insurance purposes.
Benefits of using a return to work doctor's note
Using a return to work doctor's note offers positive outcomes, including the following:
Improved employee health and safety
By requiring a doctor's note before returning to work, employers can help ensure that employees are physically and mentally fit to perform their job duties without limitations. This can help prevent workplace accidents and injuries, promoting employee health and safety.
Reduced absenteeism
By addressing any underlying health concerns and providing appropriate accommodations, return-to-work doctor's notes can help employees return to work more quickly and efficiently, reducing unnecessary absenteeism. Additionally, by ensuring employees are fit to work, these notes can help minimize presenteeism, where employees are physically present at work but not fully productive due to health issues.
Improved communication and collaboration
Return to work doctor's notes facilitate communication between employees, healthcare providers, and employers. These notes can help employers make informed decisions about work assignments, modifications, and return-to-work timelines by clearly explaining an employee's medical condition and any necessary accommodations.
Reduced legal risks and liabilities
Return to work doctor's notes can help employers avoid potential legal issues and liabilities related to workplace safety, discrimination, and accommodations. By documenting an employee's medical clearance and any necessary accommodations, these notes can provide evidence of the employer's efforts to comply with legal requirements and protect the employee's health and safety.
Research & evidence
The return to work following long-term health-related absence poses significant challenges, as highlighted in a study exploring perspectives from key organizations involved in assessment and support.
Research has shown that effective return-to-work processes, including clear medical documentation, can lead to improved outcomes for both employees and employers. A systematic review by Cancelliere and colleagues (2016) found that RTW coordination and work modification were among the most effective interventions for promoting successful return to work across various health conditions.
Clear communication and support are crucial even for healthcare professionals returning to work after extended absences (Cohen et al., 2015). This underscores the importance of standardized RTW doctors' note templates as essential tools to facilitate effective communication, convey personal health information, and create supportive environments for medical professionals to return to work successfully.
References
Cancelliere, C., Donovan, J., Stochkendahl, M. J., Biscardi, M., Ammendolia, C., Myburgh, C., & Cassidy, J. D. (2016). Factors affecting return to work after injury or illness: Best evidence synthesis of systematic reviews. Chiropractic & Manual Therapies, 24(1), 32. https://doi.org/10.1186/s12998-016-0113-z
Cohen, D., Rhydderch, M., Reading, P., & Williams, S. (2015). Doctors' health: obstacles and enablers to returning to work. Occupational Medicine, 65(6), 459–465. https://doi.org/10.1093/occmed/kqv056
Commonly asked questions
To obtain a return-to-work letter from a doctor, employees should schedule an appointment with their healthcare provider, who will assess their health status, determine if they are fit to return to work and validate paid sick leave or other concerns. During the visit, they should discuss any medical conditions or treatments that may affect their ability to perform their job duties. If the doctor deems them ready to return, they will provide a written letter stating their fitness for work, any necessary accommodations, and the date to resume their duties.
Yes, employers often verify doctor's notes to ensure their authenticity and confirm the employee's medical condition. This verification process can involve contacting the healthcare provider listed on the note to validate the details. Employers may have policies in place regarding sick leave and return-to-work procedures, which can include requiring documentation from a medical professional.
Yes, employers often verify doctor's notes to ensure their authenticity and confirm the employee's medical condition. This verification process can involve contacting the healthcare provider listed on the note to validate the details. Employers may have policies in place regarding sick leave and return-to-work procedures, which can include requiring documentation from a medical professional.
To write a doctor's note for returning to work, include the patient's name, the date of the visit, and a statement confirming that the patient has been evaluated and is fit to return to work. Specify any restrictions or accommodations needed, along with the effective date of the return. It is important to sign the note and include the doctor's contact information, practice name, and any relevant credentials to ensure its legitimacy.