Gestational Diabetes Sugar Level
Get access to a free Gestational Diabetes Sugar Level Chart. Use it as a reference to monitor and manage your patient's blood sugar levels during pregnancy.


Understanding gestational diabetes
Gestational diabetes mellitus is a glucose intolerance occurring during pregnancy, typically in the second or third trimester. It is characterized by high blood sugar levels, which can pose risks to both the mother’s and the baby’s health (American Diabetes Association, n.d.). This condition arises due to hormonal changes during pregnancy that can lead to insulin resistance and impaired glucose tolerance.
In fact, gestational diabetes affects around 2 to 10% of pregnancies in the United States, posing long-term risks such as a 35 to 60% increased chance of developing diabetes mellitus in the years following pregnancy (Gregory & Ely, 2022). However, unlike other forms of diabetes, gestational diabetes is usually temporary and resolves after childbirth. Nevertheless, careful monitoring and management are required to ensure the health and safety of both mother and child.
Women with gestational diabetes may not experience any noticeable symptoms, making regular blood sugar testing crucial to prevent gestational diabetes. High blood sugar levels can lead to complications such as preterm birth, high birth weight, and the need for cesarean delivery. Additionally, women who develop gestational diabetes are at a higher risk of developing type 2 diabetes later in life. Therefore, understanding and managing this condition is essential for long-term health.
Gestational Diabetes Sugar Level Template
Gestational Diabetes Sugar Level Example
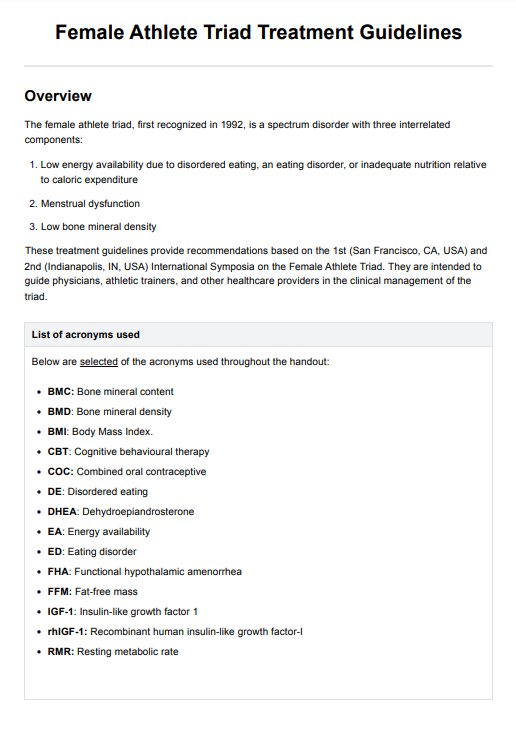
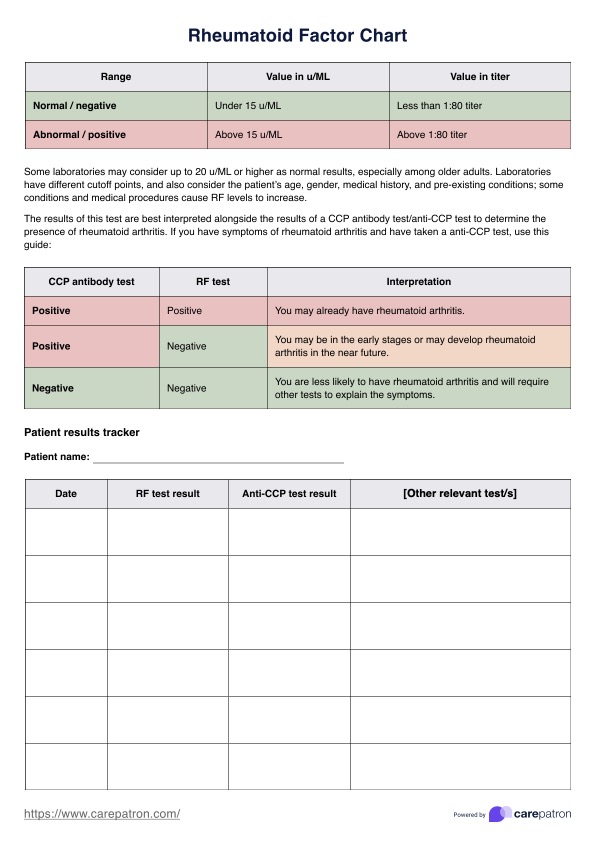
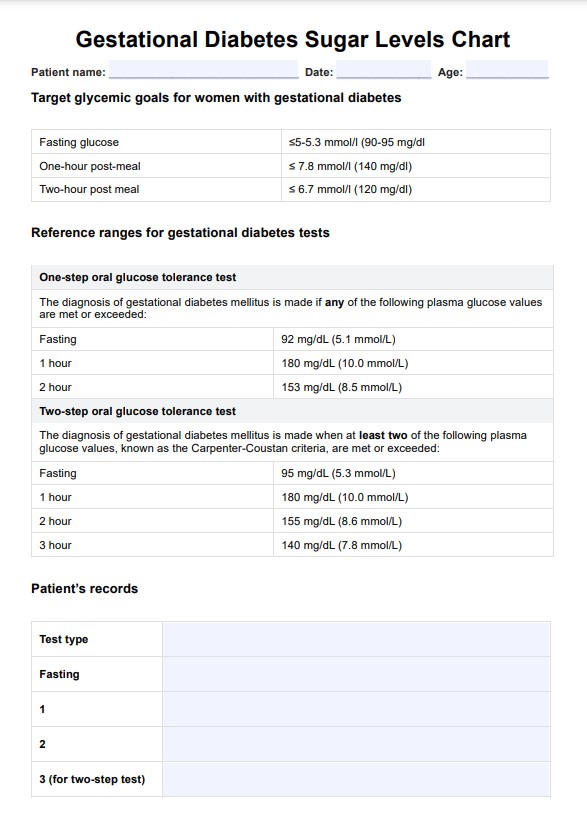
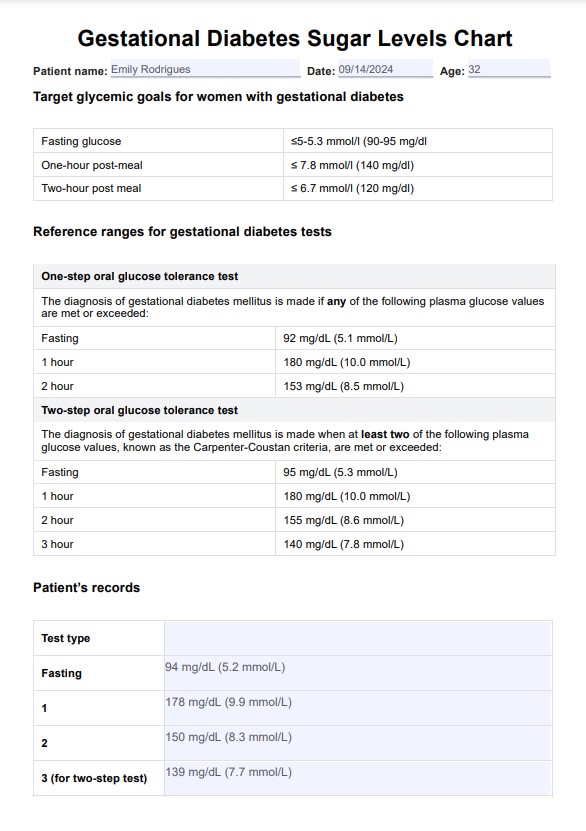
Key blood sugar tests for gestational diabetes
The American Diabetes Association (2020) recommends that all pregnant women should be tested for gestational diabetes between the 24th and 28th weeks of pregnancy. This is because high blood sugar levels during pregnancy can increase the risk of complications for both the mother and baby.
The organization also recommends using the screening tests below for diagnosing gestational diabetes:
One-step oral glucose tolerance test (OGTT)
The one-step strategy involves performing a 75-g OGTT with plasma glucose measurement when the patient is fasting and again at 1 and 2 hours. This test should be conducted between the 24th and 28th weeks of gestation in women not previously diagnosed with diabetes.
To ensure accurate results, the OGTT must be done in the morning following an overnight fast of at least 8 hours. The diagnosis of gestational diabetes mellitus is made if any of the following plasma glucose values are met or exceeded:
- Fasting: 92 mg/dL (5.1 mmol/L)
- 1 hour: 180 mg/dL (10.0 mmol/L)
- 2 hours: 153 mg/dL (8.5 mmol/L)
Two-step OGGT
The initial step involves administering a 50-g glucose load test (GLT) without requiring the patient to fast. This test should be conducted between the 24th and 28th weeks of gestation in women who have not been previously diagnosed with diabetes. Plasma glucose is measured 1 hour after the glucose load. If the plasma glucose level is equal to or greater than 130, 135, or 140 mg/dL (7.2, 7.5, or 7.8 mmol/L), the patient should proceed to the next step.
For patients who meet the criteria in the initial step, a 100-g OGTT is then performed. This test requires the patient to be fasting. Plasma glucose levels are measured at fasting and again at 1, 2, and 3 hours after the glucose load. The diagnosis of gestational diabetes mellitus is made when at least two of the following plasma glucose values, known as the Carpenter-Coustan criteria, are met or exceeded:
- Fasting: 95 mg/dL (5.3 mmol/L)
- 1 hour: 180 mg/dL (10.0 mmol/L)
- 2 hours: 155 mg/dL (8.6 mmol/L)
- 3 hours: 140 mg/dL (7.8 mmol/L)
How to use our Gestational Diabetes Sugar Level Chart
Our Gestational Diabetes Sugar Level Chart is designed to be a practical tool for healthcare professionals and patients managing gestational diabetes. Here’s how you can effectively use this gestational diabetes chart in your practice:
Step 1: Download the chart
Access the Gestational Diabetes Sugar Level Chart from the Carepatron platform. Available in both printable and digital formats, this chart can be easily referenced during patient consultations and follow-up visits.
Step 2: Conduct glucose tests
Once you have performed the necessary blood glucose tests use the chart to compare patient results to the target glycemic goals and test reference ranges for gestational diabetes mellitus.
Step 3: Educate your patients
Use the chart as to explain to patients the importance of maintaining their blood sugar within the recommended range. Help them understand how their current readings compare to normal levels and provide guidance on improving their glucose control if needed.
Step 5: Incorporate into ongoing care management
This chart can be integrated into regular prenatal check-ups to track how well blood sugar is being managed over time. Continuously monitoring normal blood sugar levels for women with gestational diabetes ensures that any necessary adjustments can be made to treatment plans, including lifestyle, healthy diet changes, or medication initiation if required.
Benefits of using our Gestational Diabetes Sugar Level Chart
Our Gestational Diabetes Sugar Level Chart provides healthcare professionals and patients with a clear and practical way to manage gestational diabetes blood sugar levels. Here’s how this tool can help:
Provides clear reference points for blood sugar management
The chart offers precise and easy-to-understand reference test points for gestational diabetes. Healthcare professionals can use it to quickly identify when blood sugar levels are outside of the recommended range, enabling faster and more accurate interventions.
Simplifies patient education
Explaining blood sugar management to patients can be challenging, but this chart makes it easier. The clear breakdown of glycemic goals for women with gestational diabetes and test reference ranges helps patients understand their results, making it simpler to follow their healthcare provider’s recommendations.
Enhances care planning and monitoring
The chart is invaluable for ongoing patient monitoring and a diabetes management plan. Managing gestational diabetes is crucial not only for blood sugar control but also for preventing complications related to digestive and kidney diseases. It allows healthcare providers to track changes in blood sugar over time and adjust treatment plans accordingly. Whether used during routine prenatal visits or in more targeted consultations, this chart ensures that gestational diabetes is well-managed throughout pregnancy.
References
American Diabetes Association. (n.d.). Gestational diabetes | ADA. Diabetes.org. https://diabetes.org/about-diabetes/gestational-diabetes
American Diabetes Association. (2020). Classification and Diagnosis of diabetes: Standards of Medical Care in diabetes—2020. Diabetes Care, 43(Supplement 1), S14–S31. https://doi.org/10.2337/dc20-s002
Gregory, E., & Ely, D. (2022). Trends and Characteristics in Gestational Diabetes: United States, 2016–2020. In Centers for Disease Control and Prevention. National Vital Statistics System. https://www.cdc.gov/nchs/data/nvsr/nvsr71/nvsr71-03.pdf
National Institute of Diabetes and Digestive and Kidney Diseases. (2017, May). Tests & diagnosis for gestational diabetes | NIDDK. https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/gestational/tests-diagnosis#:~:text=Oral%20Glucose%20Tolerance%20Test%20(OGTT
Commonly asked questions
For most women diagnosed with gestational diabetes, blood glucose levels should be checked at least four times a day: fasting in the morning and one to two hours after each meal. The exact frequency will depend on individual circumstances, so following your healthcare provider's recommendations is essential.
For women with gestational diabetes, the target fasting blood sugar level is usually below 95 mg/dl. One hour after meals, blood sugar should be below 140 mg/dl, and two hours after meals, it should be below 120 mg/dl.
The target levels may vary for each individual. However, typical recommended ranges are fasting: 70-95 mg/dL, pre-meal: 95-105 mg/dL, and post-meal: <120 mg/dL.
Yes, gestational diabetes typically resolves after the baby is born. However, women who have had gestational diabetes are at a higher risk of developing type 2 diabetes later in life. Maintaining a balanced diet and healthy lifestyle and following up with your healthcare provider postpartum to monitor your blood sugar levels are essential.



















-template.jpg)