Dysthymia DSM-5 Criteria
Access a helpful reference tool with our Dysthymia DSM-5 Criteria when assessing persistent depressive symptoms in patients.


What is persistent depressive disorder (dysthymia)?
Persistent depressive disorder (PDD), also known as dysthymia, is a chronic major depressive disorder characterized by a persistently depressed mood lasting at least two years in adults or one year in children and adolescents (American Psychiatric Association, 2013).
It's marked by milder but longer-lasting symptoms compared to major depressive disorder. Individuals with PDD often experience low self-esteem, fatigue, and difficulties with concentration or decision-making. While less severe than major depression, its chronic nature can significantly impact daily functioning and quality of life.
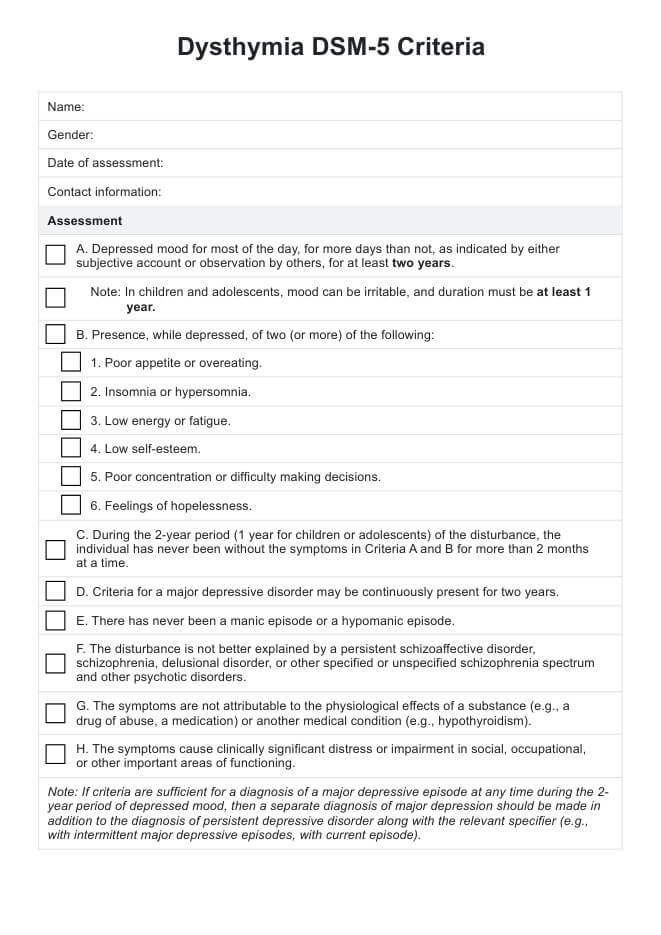
Dysthymia DSM-5 Criteria Template
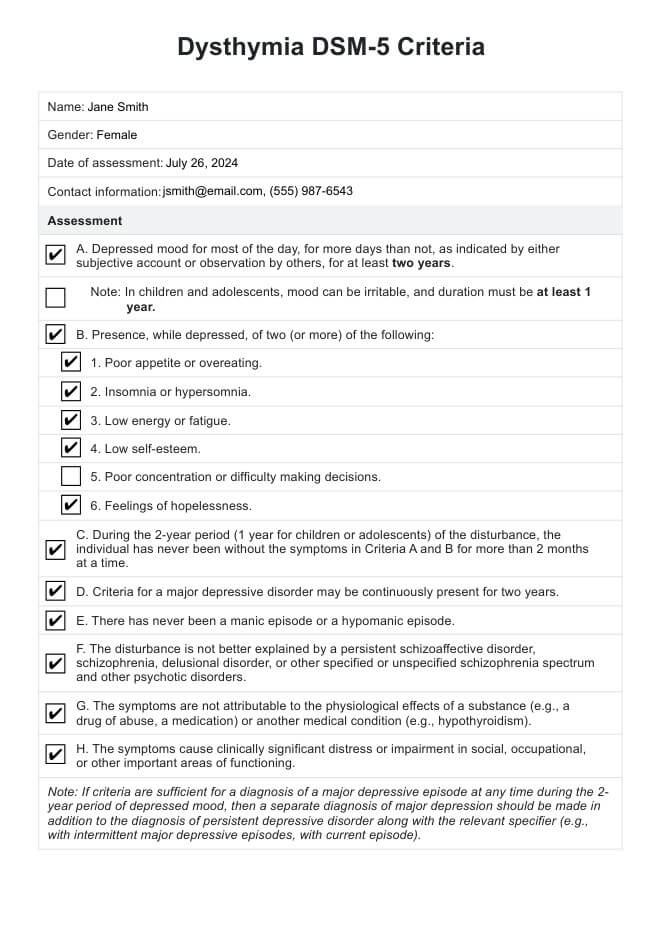
Dysthymia DSM-5 Criteria Sample
How is dysthymia diagnosed?
Diagnosing dysthymia, like other mood disorders and mental conditions, involves a comprehensive evaluation based on the criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). The primary requirement is a depressed mood for most of the day, more often than not, for at least two years in adults or one year in children and adolescents (American Psychiatric Association, 2013). Depressive symptoms should also cause clinically significant distress or impairment.
Diagnosis typically involves a thorough clinical interview, consideration of medical history, and sometimes psychological assessments. It's important to note that individuals with PDD or chronic depression may also experience a major depressive episode, leading to a diagnosis of "double depression."
It's also crucial to rule out other conditions that may better explain the symptoms, such as anxiety disorders, other related depressive disorders, a possible psychotic disorder, physiological effects of substances, or medical conditions. Healthcare providers should be aware that the chronic nature of PDD can sometimes lead patients to consider their symptoms as part of their personality rather than a treatable condition.
Dysthymia DSM-5 diagnosis criteria
The primary criterion is the presence of a depressed mood for most of the day, more days than not, for at least two years in adults or one year in children and adolescents.
During this period, individuals must experience at least two of the following symptoms:
- Poor appetite or overeating
- Insomnia or hypersomnia
- Low energy or fatigue
- Low self-esteem
- Poor concentration or difficulty making decisions
- Feelings of hopelessness
It's important to note that during the specified duration (two years for adults, one year for children/adolescents), the individual should not have been without symptoms for more than two months at a time. This criterion emphasizes the persistent nature of PDD.
The symptoms must also cause clinically significant distress or impairment in social, occupational, or other important areas of functioning. This criterion ensures that the diagnosis is applied only when the symptoms are severe enough to substantially impact the individual's life.
Specifying if the clinical presentation includes anxious distress and atypical features is also important. It should also be indicated if this mood disorder has occurred with a late or an early onset. For the most recent 2 years of the disorder, it is also important to specify if it is a pure dysthymic syndrome or if it occurs with a persistent major depressive episode.
The Dysthymia DSM-5 Criteria within the template is a reference tool formatted as a checklist with a space for additional notes. This ensures that this can be a helpful resource in your clinical practice, whether for taking notes or as a handout when educating clients or patients.
How is dysthymia treated?
Treatment for dysthymia typically involves a combination of psychotherapy and medication. The chronic nature of PDD often requires a long-term, multifaceted approach to achieve the best outcomes.
Psychotherapy
Psychotherapy, particularly cognitive-behavioral therapy (CBT) and interpersonal therapy (IPT), has shown effectiveness in treating PDD. CBT helps individuals identify and change negative thought patterns and behaviors, while IPT focuses on improving interpersonal relationships and social functioning. These therapeutic approaches can be especially beneficial in addressing the long-standing negative self-perceptions and interpersonal difficulties often associated with PDD.
Medication
Medication is frequently used in conjunction with psychotherapy. Selective serotonin reuptake inhibitors (SSRIs) are typically the first-line pharmacological treatment due to their efficacy and generally favorable side effect profile.
For individuals with PDD who experience episodes of major depression ("double depression"), a more intensive treatment approach may be necessary. This might involve higher medication doses, combination pharmacotherapy, or more frequent psychotherapy sessions.
Lifestyle modifications
Lifestyle modifications can also support treatment. Regular exercise, consistent sleep schedules, and engaging in enjoyable activities can help manage symptoms and improve overall well-being.
It's important to note that treatment response in PDD can be slower compared to acute depressive episodes. Patience and persistence are often required, and treatment plans may need adjustment over time. Regular follow-ups are crucial to monitor progress and adjust interventions as needed.
Reference
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Pearson.
Commonly asked questions
Persistent depressive disorder (PDD), also known as dysthymia, is characterized by a depressed mood that lasts for at least 2 years, with the presence of at least two additional symptoms such as poor appetite, insomnia, low energy, low self-esteem, poor concentration, or feelings of hopelessness. In contrast, cyclothymia is a milder form of bipolar disorder, involving mood swings between hypomania and mild depression that last for at least 2 years in adults or 1 year in children and adolescents.
If left untreated, persistent depressive disorder (dysthymia) can lead to significant impairment in daily functioning, social relationships, and overall quality of life. It may also increase the risk of developing a major depressive episode or other mental health conditions.
The DSM-5 code for persistent depressive disorder (PDD) is F34.1.



















-template.jpg)


















































































