OCI-R
Explore the OCI-R, a trusted tool for diagnosing OCD and hoarding disorders, aiding in precise symptom assessment and treatment planning.


What is the Obsessional Compulsive Inventory-Revised (OCI-R)?
The Obsessional Compulsive Inventory-Revised (OCI-R) is a widely used self-reporting psychological assessment tool designed to evaluate the severity and presence of symptoms associated with Obsessive-Compulsive Disorder (OCD). This inventory, which is an updated version of the original Obsessional Compulsive Inventory, comprises 18 items that participants respond to based on their experiences over the past month. The responses are rated on a 5-point Likert scale ranging from 0 ("not at all") to 4 ("extremely").
The OCI-R, which assesses OCD and hoarding disorder, is structured around six subscales, each reflecting a specific dimension of OCD symptoms:
- Washing
- Checking
- Ordering
- Obsessing
- Hoarding
- Neutralizing
Each subscale consists of three items, making the inventory concise yet comprehensive as it measures OCD symptoms, along with more severe hoarding symptoms. This structure allows clinicians and researchers to assess not only the overall severity of OCD but also specific symptom dimensions, which can guide targeted therapeutic interventions.
The revised version, developed by Edna Foa and her colleagues, is favored for its brevity, reliability, and validity, making it an efficient tool for clinical settings and research studies. It helps in the diagnosis, assessment, and monitoring of treatment progress in individuals with OCD. The OCI-R has been validated in various populations and has been translated into several languages, supporting its applicability in diverse cultural contexts.
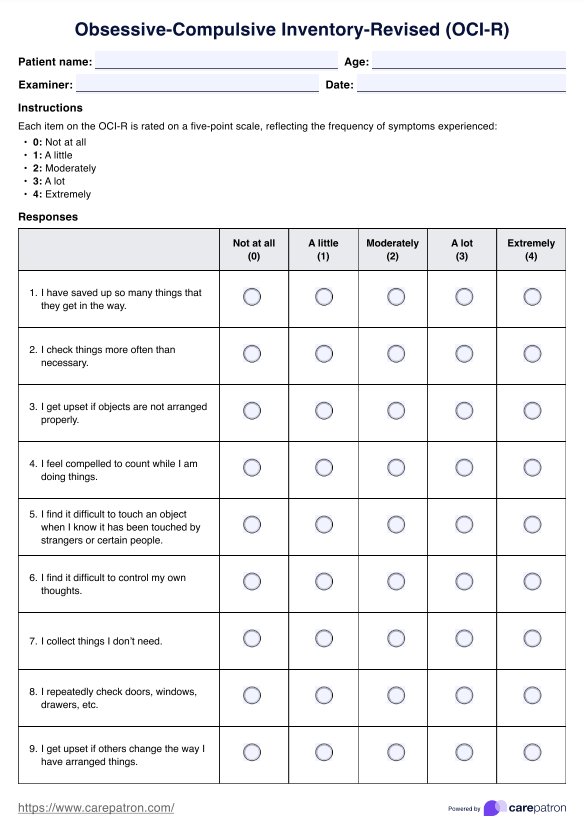
OCI-R Template
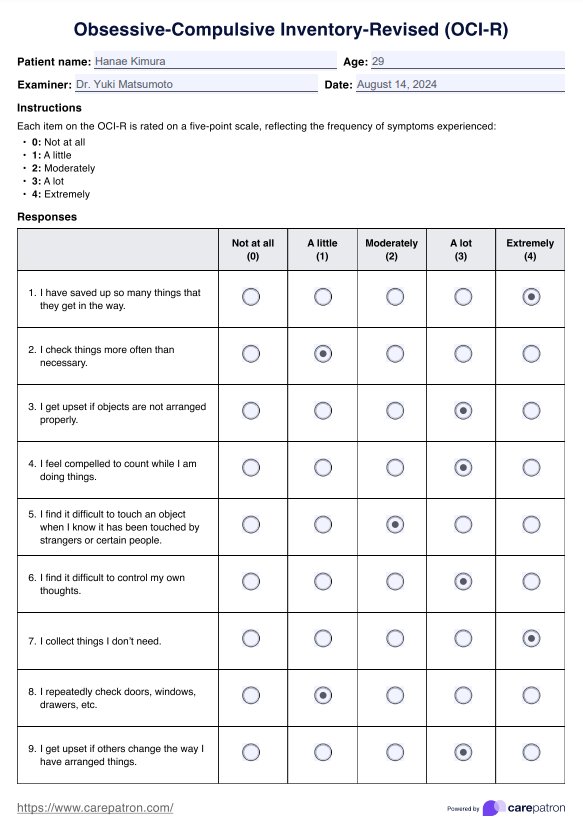
OCI-R Example
How to use our OCI-R template
This template is designed for the structured assessment of Obsessive-Compulsive Disorder (OCD) symptoms using the Obsessive-Compulsive Inventory-Revised (OCI-R). It aids clinicians and researchers in capturing essential information and systematically evaluating symptom severity.
Step 1: Collect patient information
Enter the patient's name, age, date of assessment, and examiner's details to start. This template is optimized for use in clinical samples, ensuring accurate data collection and analysis in diverse settings.
Step 2: Instruct on the rating scale
Clearly explain the five-point rating scale to the patient:
- 0: Not at all - No occurrence of the symptom.
- 1: A little - Infrequent occurrence.
- 2: Moderately - Occasional occurrence with moderate severity.
- 3: A lot - Frequent and distressing occurrence.
- 4: Extremely - Very frequent and highly distressing occurrence. Ensure the patient understands each level to guarantee accurate responses.
Step 3: Administer the OCI-R
Guide the patient to complete the 18-item questionnaire, selecting the option that best describes the frequency of their symptoms based on the past month's experiences. Emphasize the importance of honesty to ensure the accuracy of the assessment.
Step 4: Calculate and interpret scores
Once the questionnaire is completed, tally the scores for each item to derive the total score. Higher scores indicate more severe OCD symptoms. Review the scoring section in the template to identify areas requiring immediate attention and therapeutic intervention.
Step 5: Document and plan further action
Utilize the additional notes section for any relevant observations, patient comments, or specific circumstances that might influence the assessment or clinical sample. Discuss the results with the patient, outlining potential treatment options or further diagnostic evaluations.
Scoring and interpretation
The Obsessive-Compulsive Inventory-Revised is a valuable tool for assessing the severity of OCD symptoms. The total score ranges from 0 to 72, with the OCD-specific portion consisting of 15 items (numbers 2-6, 8-12, and 14-18) and scores ranging from 0 to 60. Higher scores on this scale indicate more intense OCD symptoms, providing a comprehensive overview of the individual's condition.
Within the OCD component, the OCI-R includes five subscales: Washing, Obsessing, Ordering, Checking, and Neutralizing. Each subscale is scored from 0 to 12 and offers clinical percentiles that compare the respondent's scores to those of a clinically diagnosed OCD group. These subscales provide a nuanced understanding of specific OCD manifestations, such as contamination fears, intrusive thoughts, arranging compulsions, excessive checking behaviors, and number-related preoccupations.
In addition to the OCD-specific items, the OCI-R includes a separate subscale for hoarding disorder and severe hoarding symptoms, comprising three items (1, 7, and 13) with scores ranging from 0 to 12. A score of 6 or above on this subscale is considered the threshold for a probable hoarding disorder diagnosis, offering a quick screening tool for this distinct but related condition.
Next steps after using the OCI-R
After administering the Obsessional Compulsive Inventory-Revised and obtaining results, clinicians and researchers can follow a structured approach to interpret and act on the findings. This process involves several steps designed to address the symptoms and impacts of OCD in individuals effectively.
Analyze the results
The first step involves a detailed analysis of the OCI-R scores. Analyze results meticulously to facilitate an accurate OCD diagnosis, considering the total and subscale scores. High scores in specific areas may indicate more severe symptoms or areas of concern requiring targeted interventions.
Discuss the findings with the individual
It's crucial to have an open discussion with the individual about their OCI-R results. This conversation should cover how their symptoms manifest daily and any specific challenges they face. Understanding the individual's perspective helps validate and align their experiences with therapeutic goals.
Develop a treatment plan
Develop personalized treatment plans, including behavioural and cognitive psychotherapy. This plan may include cognitive-behavioral therapy (CBT), particularly Exposure and Response Prevention (ERP), which is considered the gold standard for treating OCD. Medication may also be considered if necessary.
Implement interventions
Begin implementing the agreed-upon therapeutic interventions. Regular sessions focusing on CBT techniques and possibly incorporating medication management should be initiated. Ensure that interventions are adapted as needed based on the individual's progress and any changes in their symptoms.
Monitor progress and adjust the treatment
Continuously monitor the individual's progress through regular check-ins and possibly re-administration of the OCI-R at intervals. Use the results to adjust the treatment plan dynamically. This might involve intensifying therapy, exploring additional therapy modalities, or adjusting medications.
Long-term management
Finally, establish a long-term management plan that includes strategies for relapse prevention and coping mechanisms for managing OCD symptoms. Conduct periodic evaluations to adapt the treatment plan as the individual's needs change over time, ensuring sustained support and intervention effectiveness.
Commonly asked questions
Yes, OCD can be effectively treated without medication, especially through cognitive-behavioral therapy (CBT) and specifically through techniques like exposure and response prevention (ERP).
OCD can significantly disrupt daily life by causing distressing and intrusive thoughts or other anxiety disorders, leading to repetitive behaviors or rituals that interfere with daily activities and social interactions.
Group therapy can be beneficial for individuals with OCD, as it provides support from peers, reduces feelings of isolation and anxiety disorders, and allows individuals to share coping strategies in a supportive environment.



















-template.jpg)


















































































