Premenstrual Dysphoric Disorder DSM-5
Explore the criteria of Premenstrual Dysphoric Disorder (PMDD) as outlined in DSM-5, shedding light on panic disorder and its impact on mental health.


What is PMDD according to the DSM-5?
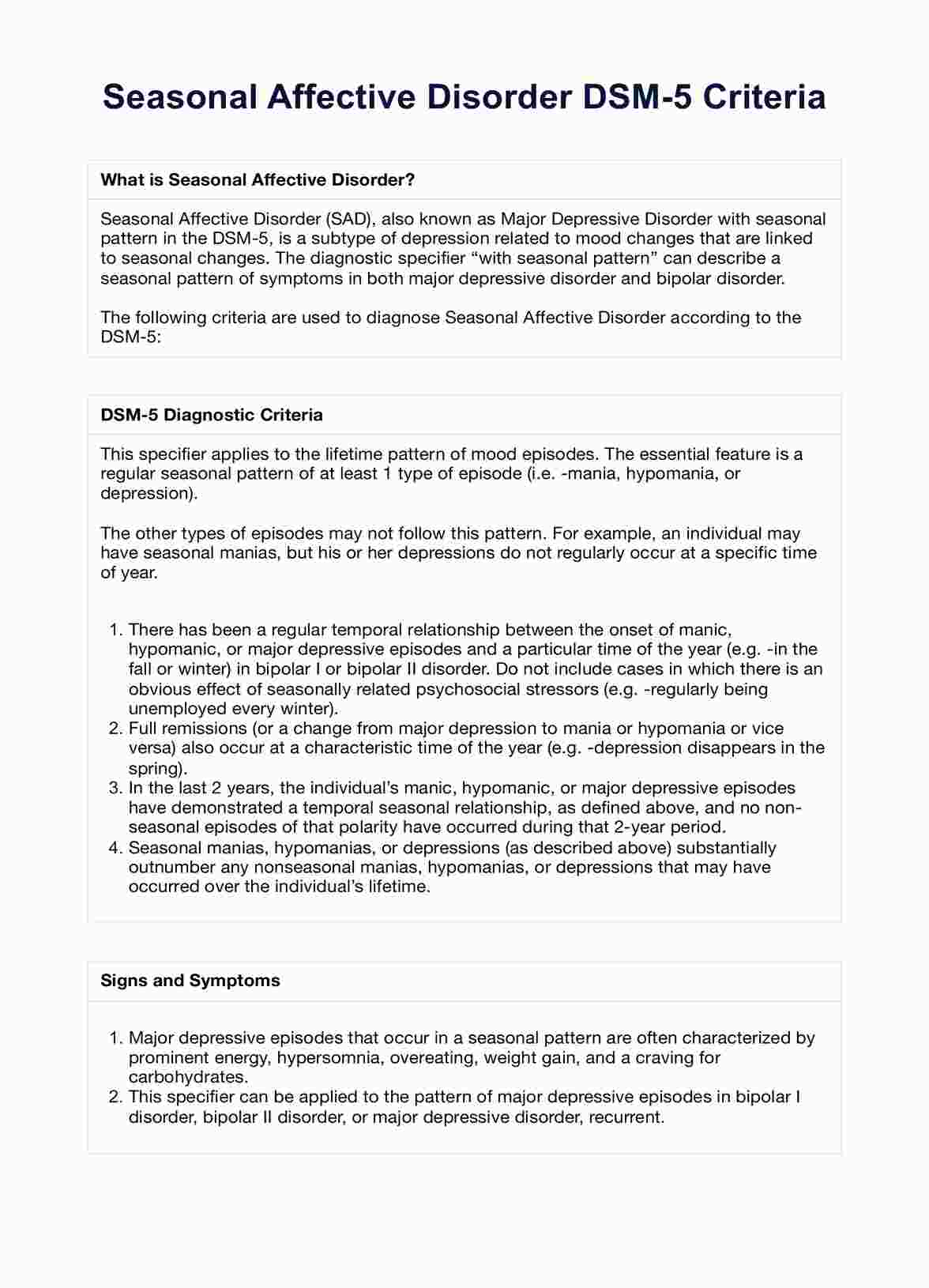
Premenstrual Dysphoric Disorder (PMDD) is a condition classified in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) under depressive disorders. It is characterized by severe mood symptoms, emotional disturbances, and physical symptoms occurring during the late luteal phase of most menstrual cycles. PMDD symptoms markedly interfere with daily functioning and result in clinically significant distress. These symptoms may include marked irritability, mood swings, depressed mood, feelings of sadness, anger, anxiety, marked affective lability, and decreased interest in usual activities.
Physical symptoms commonly associated with PMDD include joint or muscle pain, breast tenderness, weight gain, food cravings, major depression, and other somatic symptoms. These symptoms typically appear following ovulation and improve with the onset of menses.
PMDD diagnosis requires the presence of specific depressive symptoms during most menstrual cycles and their resolution shortly after menstruation begins. Risk factors for PMDD include hormonal fluctuations, reproductive hormones, and underlying mood disorders such as major depressive disorder or persistent depressive disorder.
Treatment for PMDD may involve psychotherapy, lifestyle changes, and medication, including selective serotonin reuptake inhibitors (SSRIs) to alleviate symptoms. It's crucial to differentiate PMDD from other mood disorders, premenstrual syndrome (PMS), and medical conditions to provide appropriate management and support to individuals affected by this condition.
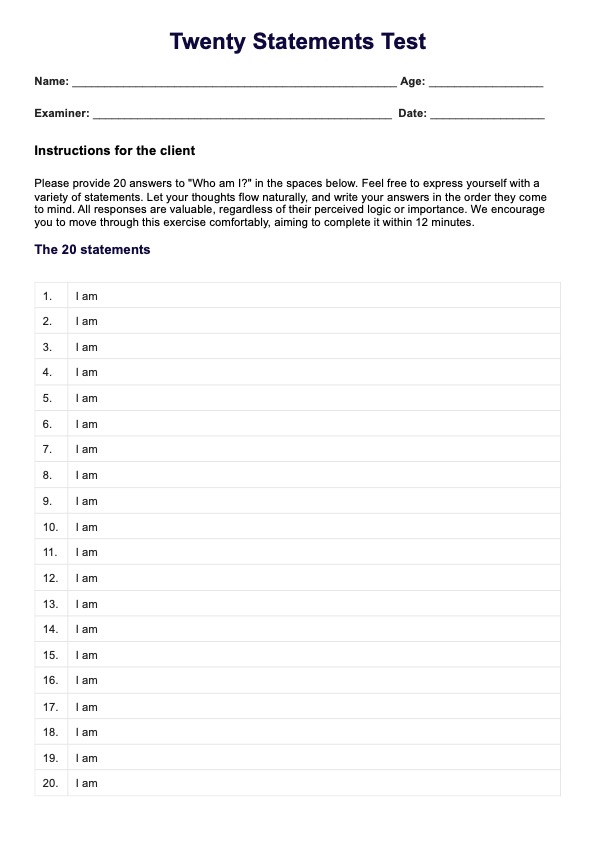
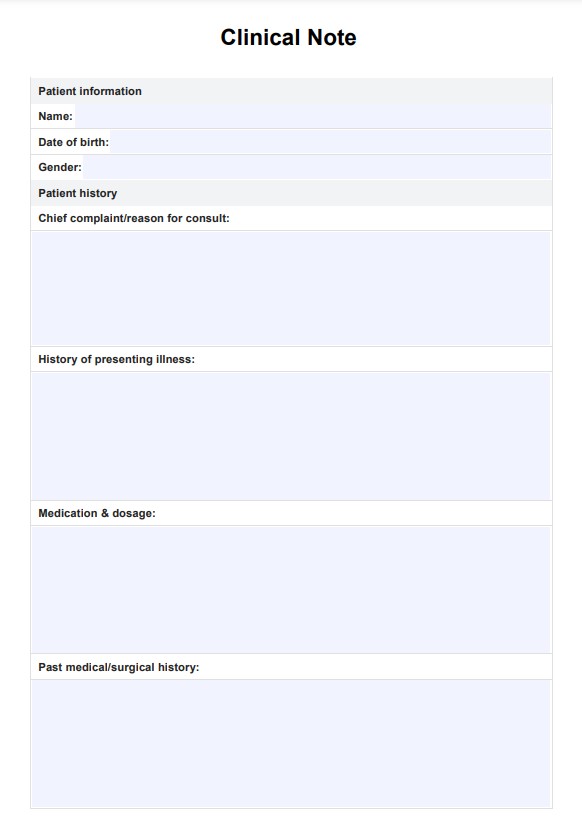
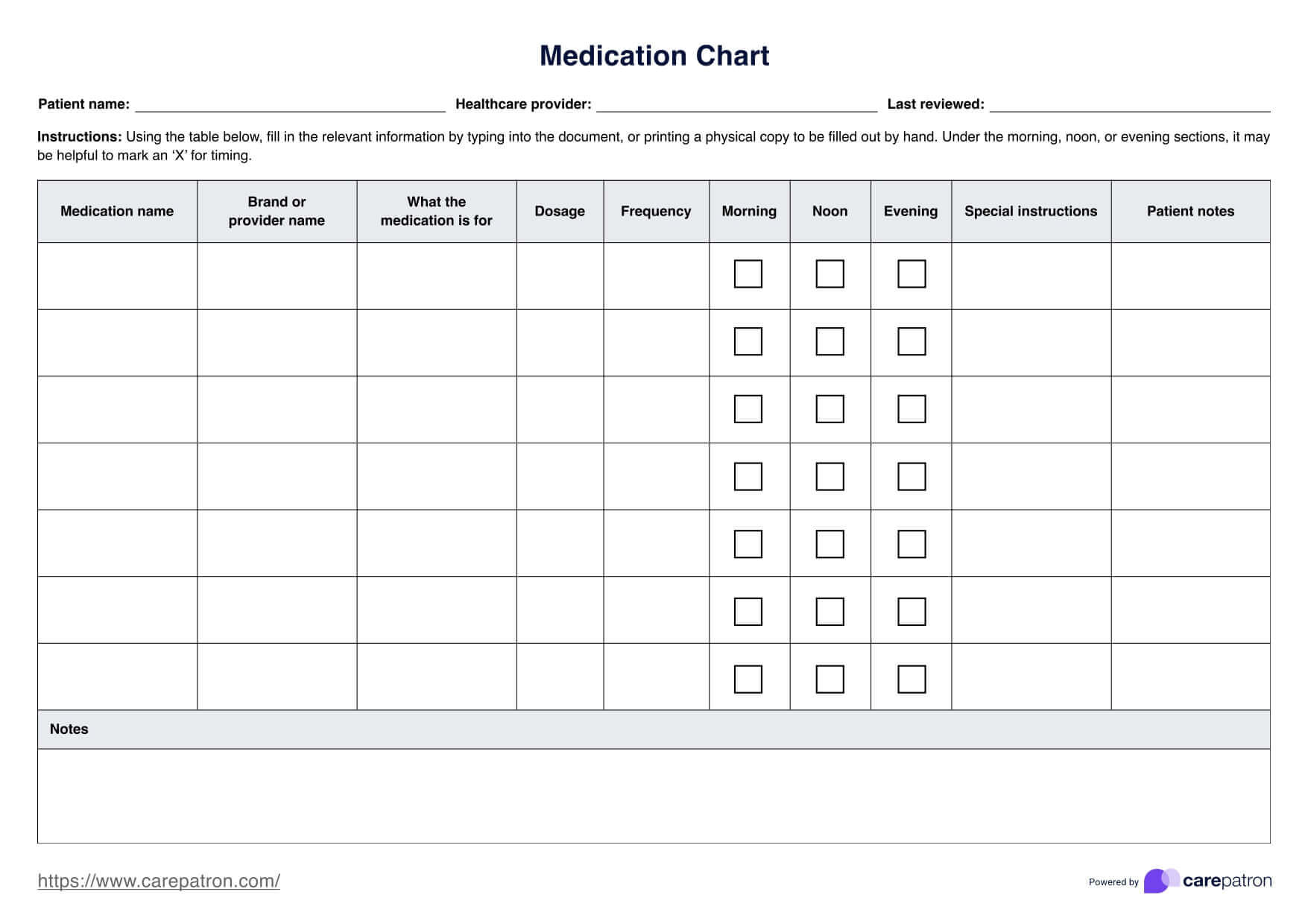
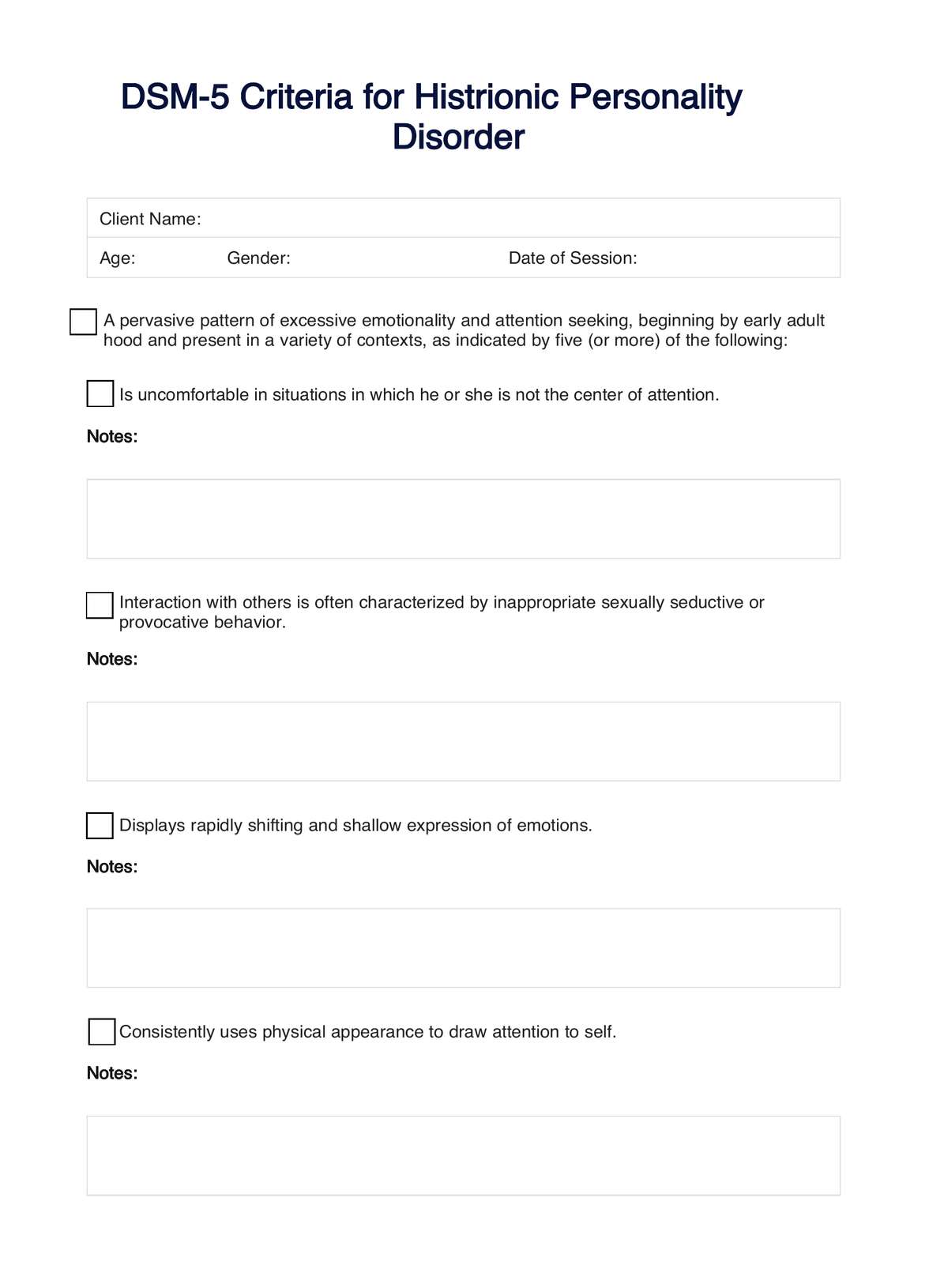
Premenstrual Dysphoric Disorder DSM-5 Template
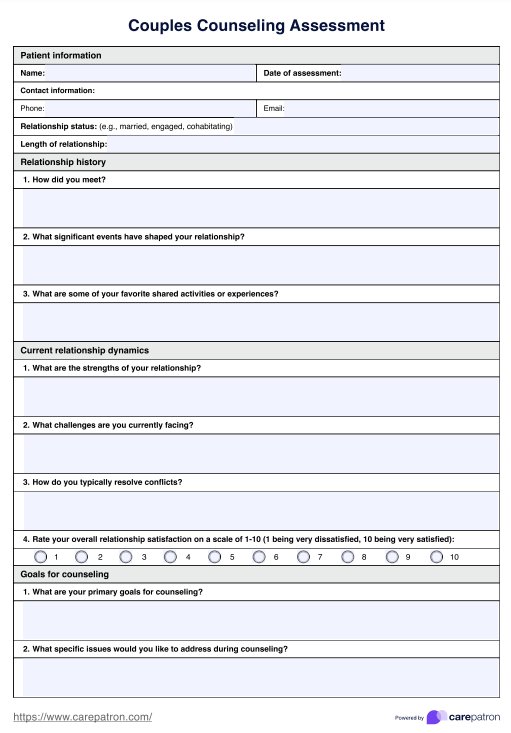
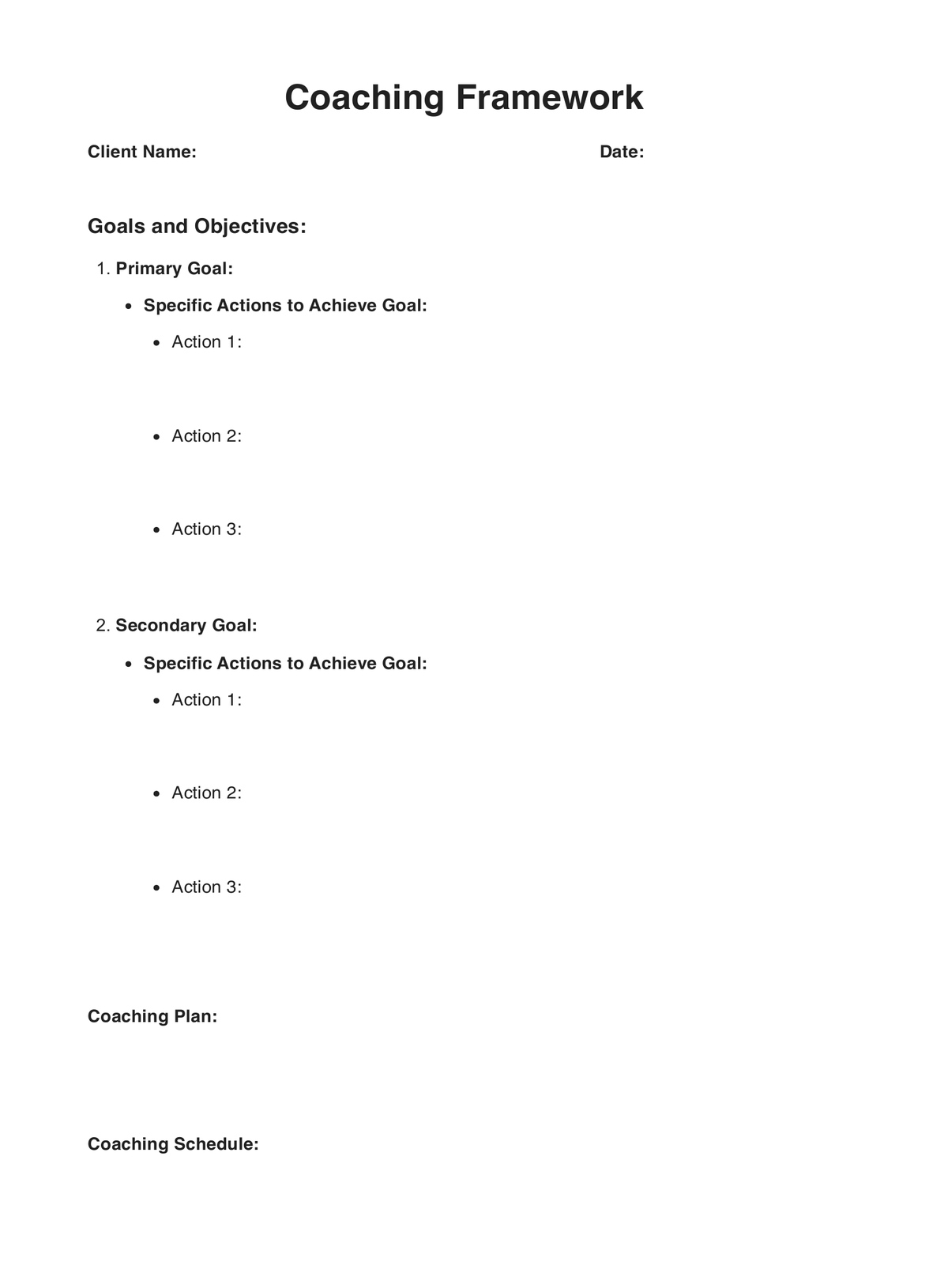
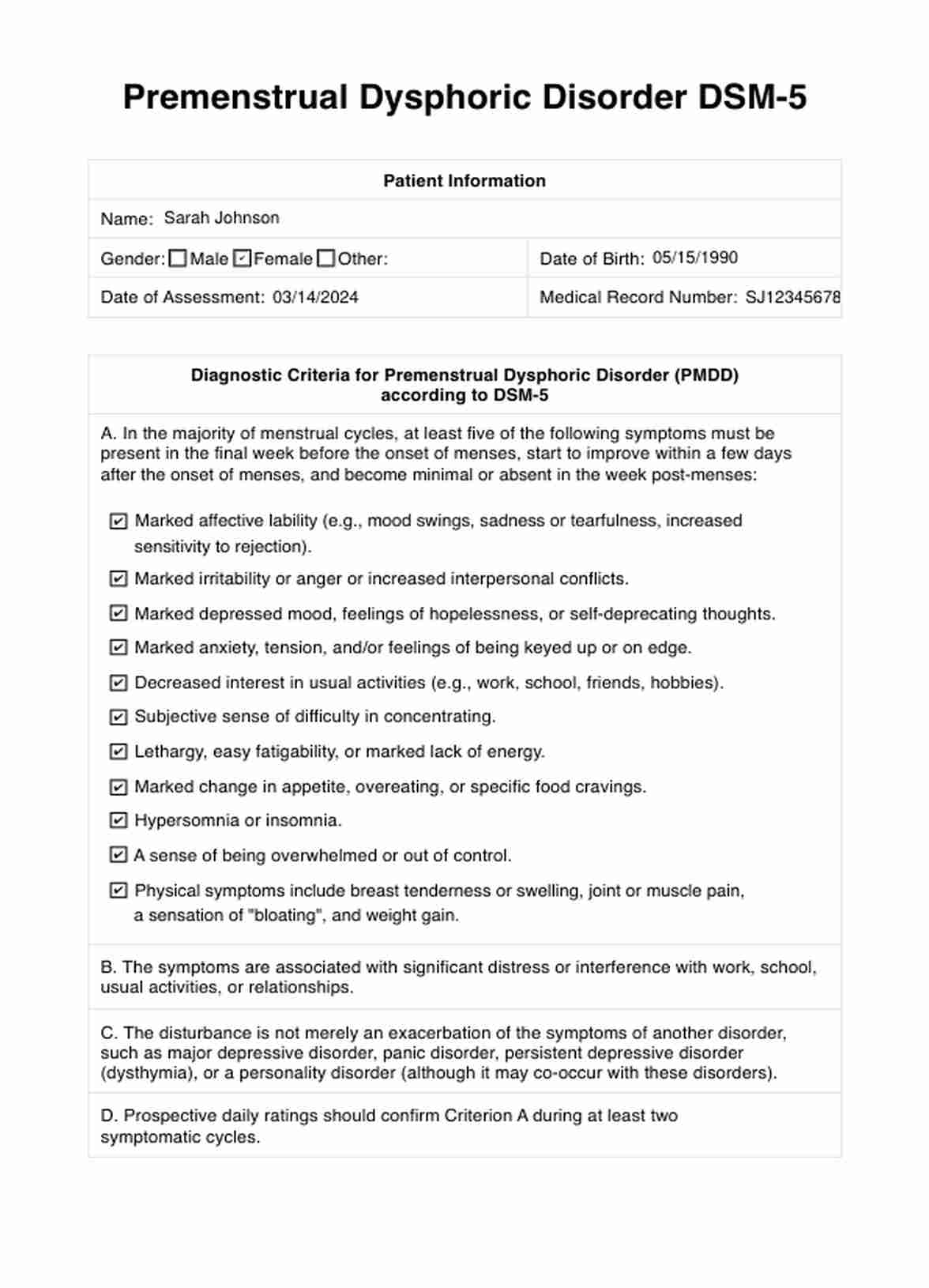
Premenstrual Dysphoric Disorder DSM-5 Example
How is PMDD distinguished from regular PMS?
Premenstrual Dysphoric Disorder (PMDD) is distinguished from regular Premenstrual Syndrome (PMS) by the severity, duration, and impact of symptoms on daily functioning. While both PMDD and PMS involve physical and emotional symptoms that occur in the late luteal phase of the menstrual cycle, PMDD is characterized by more severe and debilitating symptoms that significantly interfere with daily life.
Here's how PMDD is distinguished from regular PMS:
- Severity: PMDD symptoms are more severe and debilitating compared to PMS. Individuals with PMDD experience intense mood disturbances, such as severe irritability, depression, mood swings, and anxiety, which may significantly impair their ability to function normally.
- Duration: PMDD symptoms are typically more persistent and last longer than those of PMS. While PMS symptoms usually resolve after menstruation begins, PMDD symptoms may persist throughout the menstrual cycle and improve only after the onset of menstruation.
- Impact on daily functioning: PMDD symptoms cause significant distress and impairment in daily functioning, affecting various areas of life, including work, school, relationships, and social activities. In contrast, PMS symptoms may cause mild discomfort but generally do not disrupt daily activities to the same extent.
- Specificity: PMDD is characterized by specific symptoms, such as marked irritability, mood swings, and affective lability, which are not typically present in regular PMS. These symptoms are listed in the diagnostic criteria for PMDD but may not be as pronounced in individuals with milder forms of premenstrual symptoms.
- Response to treatment: PMDD often requires more intensive treatment approaches, such as medication (e.g., SSRIs) and psychotherapy, due to the severity of symptoms. PMS symptoms, on the other hand, may be managed with lifestyle changes, over-the-counter pain relievers, and self-care strategies.
What causes PMDD?
The exact cause of Premenstrual Dysphoric Disorder (PMDD) is not fully understood, but it is believed to involve a combination of biological, genetic, and environmental factors. Some potential contributors to the development of PMDD include:
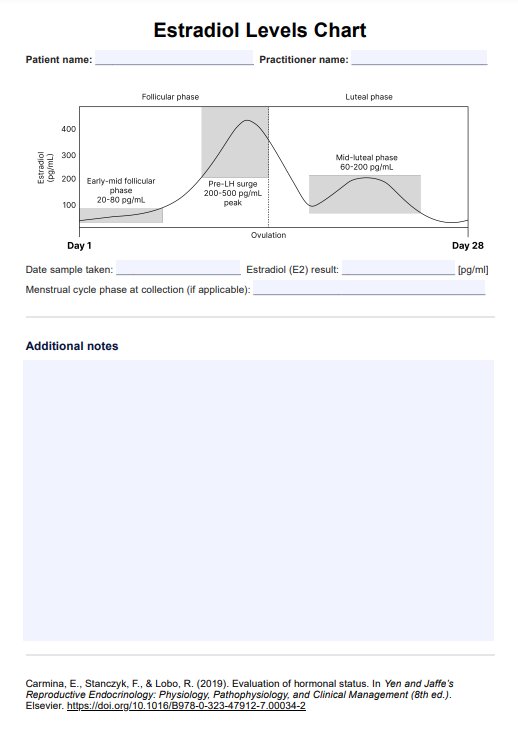
- Hormonal changes: Fluctuations in reproductive hormones, such as estrogen and progesterone, during the menstrual cycle may play a role in triggering PMDD symptoms. The transition from the follicular phase to the luteal phase, marked by changes in hormone levels, is particularly relevant to the onset of PMDD symptoms.
- Neurotransmitter imbalance: PMDD may be associated with alterations in neurotransmitter activity, particularly serotonin, which regulates mood, emotions, and behavior. It is hypothesized that changes in serotonin levels during the menstrual cycle contribute to the mood disturbances and emotional symptoms characteristic of PMDD.
- Genetic factors: There may be a genetic predisposition to PMDD, as it tends to run in families. Studies have suggested that certain genetic variations may increase susceptibility to PMDD or influence individual responses to hormonal fluctuations and stress.
- Sensitivity to hormonal changes: Some individuals may be more sensitive to hormonal changes during the menstrual cycle, leading to exaggerated responses in mood and behavior. This heightened sensitivity may contribute to the development of PMDD symptoms.
- Environmental and psychosocial factors: Stress, lifestyle factors, and psychosocial stressors can exacerbate PMDD symptoms or contribute to their severity. Poor coping mechanisms, inadequate social support, and environmental stressors may interact with hormonal changes to worsen symptoms.
- Neuroendocrine dysregulation: Dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis regulates stress responses, and hormone levels have been implicated in PMDD. Dysfunction in the HPA axis may contribute to mood disturbances and exacerbate PMDD symptoms.
How common is PMDD?
Estimating the prevalence of Premenstrual Dysphoric Disorder (PMDD) can be challenging due to variations in diagnostic criteria, study methodologies, and cultural factors. However, research suggests that PMDD affects a significant proportion of individuals with menstrual cycles.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), PMDD is estimated to affect approximately 2-5% of menstruating individuals. However, some studies have reported higher prevalence rates, ranging from 3% to 8%, depending on the population studied and the diagnostic criteria used.
PMDD tends to occur most commonly during the reproductive years, typically starting in the late teens or early twenties, and may persist until menopause. It is more prevalent among individuals with a personal or family history of mood disorders, such psychiatric disorders such as major depressive disorder or bipolar disorder.
It's important to note that while PMDD is less common than Premenstrual Syndrome (PMS), which affects a more significant proportion of individuals, PMDD is characterized by more severe symptoms and more significant impairment in daily functioning. Additionally, many cases of PMDD may go undiagnosed or misdiagnosed due to a lack of awareness among healthcare providers and individuals themselves.
How is PMDD diagnosed?
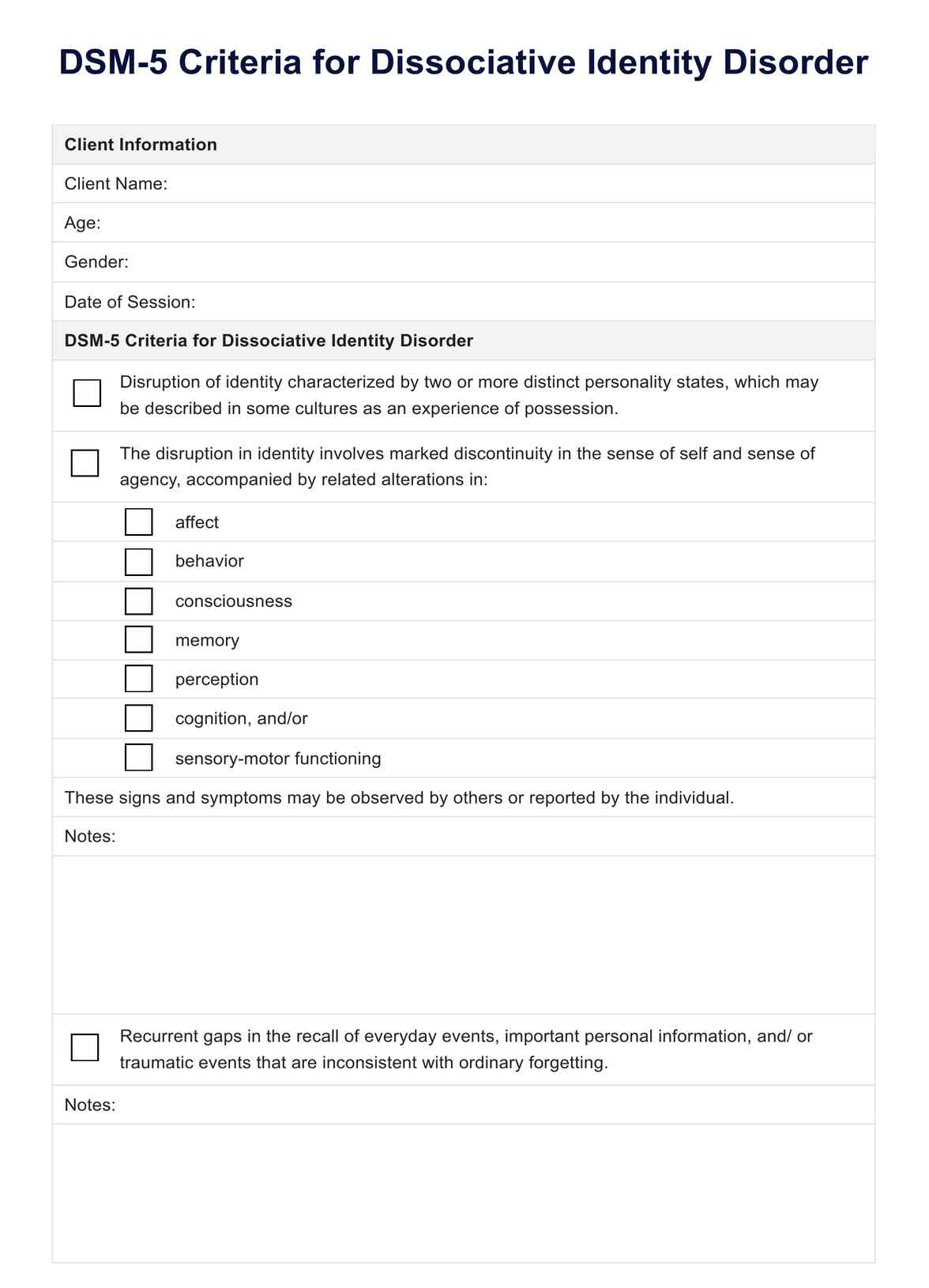
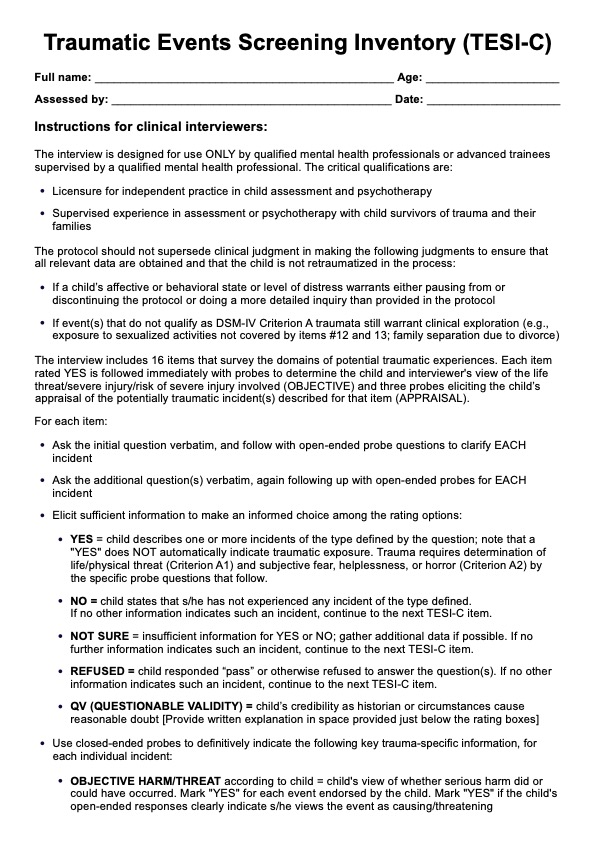
Diagnosing Premenstrual Dysphoric Disorder (PMDD) involves a thorough evaluation of symptoms, medical history, and menstrual cycle patterns. The process typically includes the following steps:
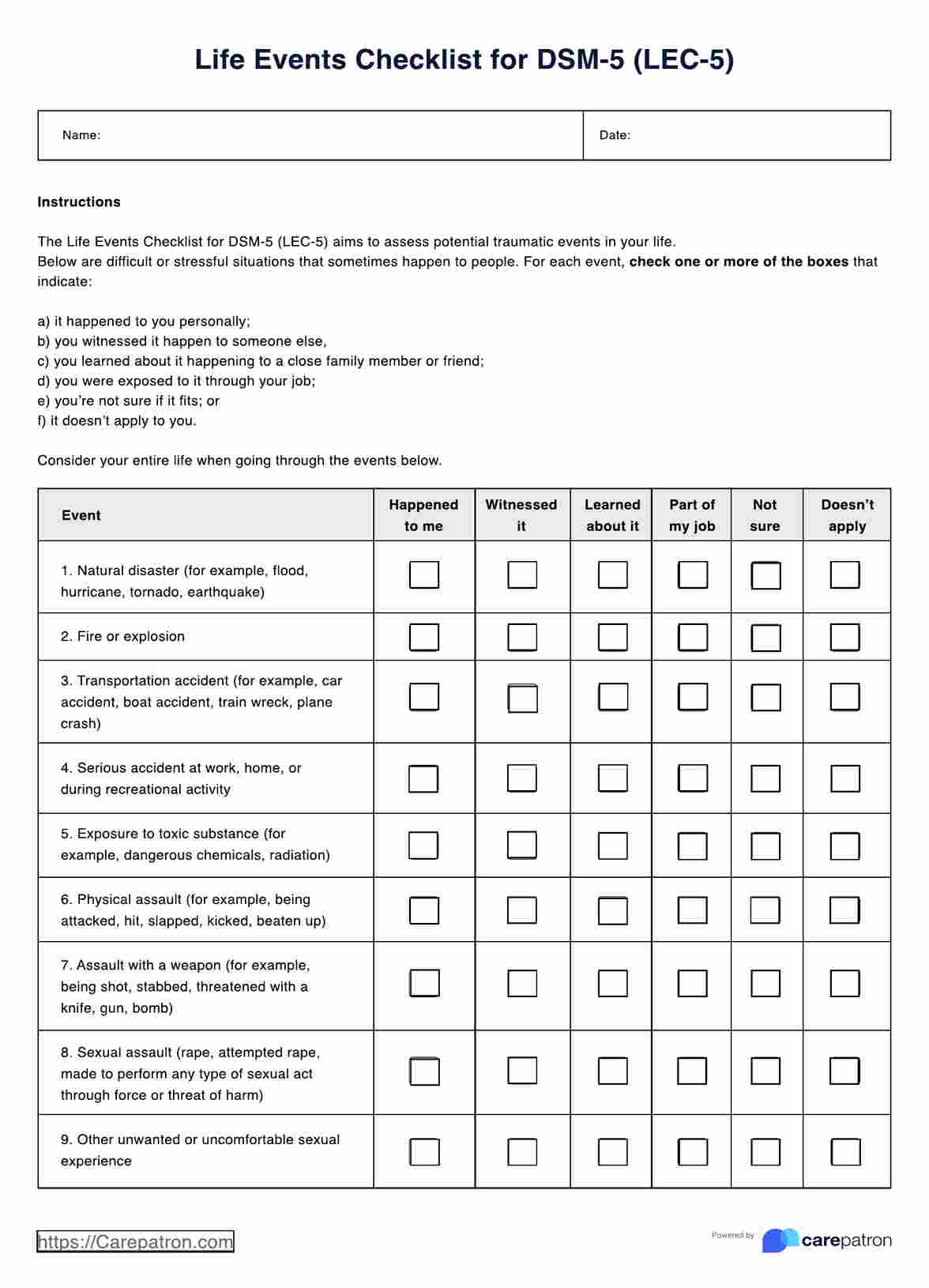
- Clinical assessment: A healthcare provider will conduct a comprehensive clinical examination, including a detailed history of symptoms and their impact on daily functioning. They may ask questions about the timing, duration, and severity of mood and physical symptoms experienced during the menstrual cycle.
- Symptom tracking: Keeping a symptom diary or calendar to track mood changes, physical symptoms, and their relationship to the menstrual cycle can provide valuable information for diagnosis. Tracking symptoms over several menstrual cycles helps identify patterns and confirm the presence of PMDD.
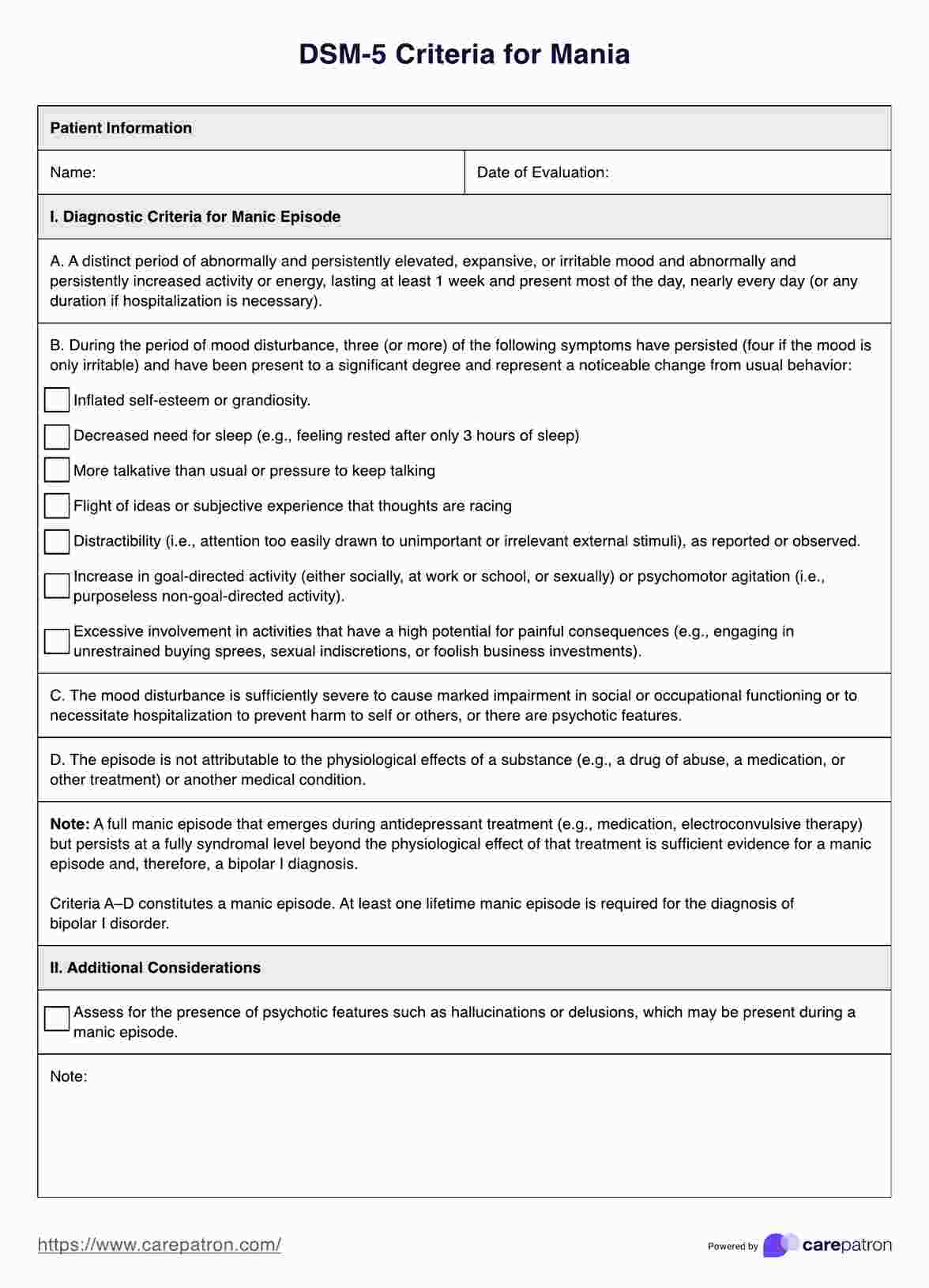
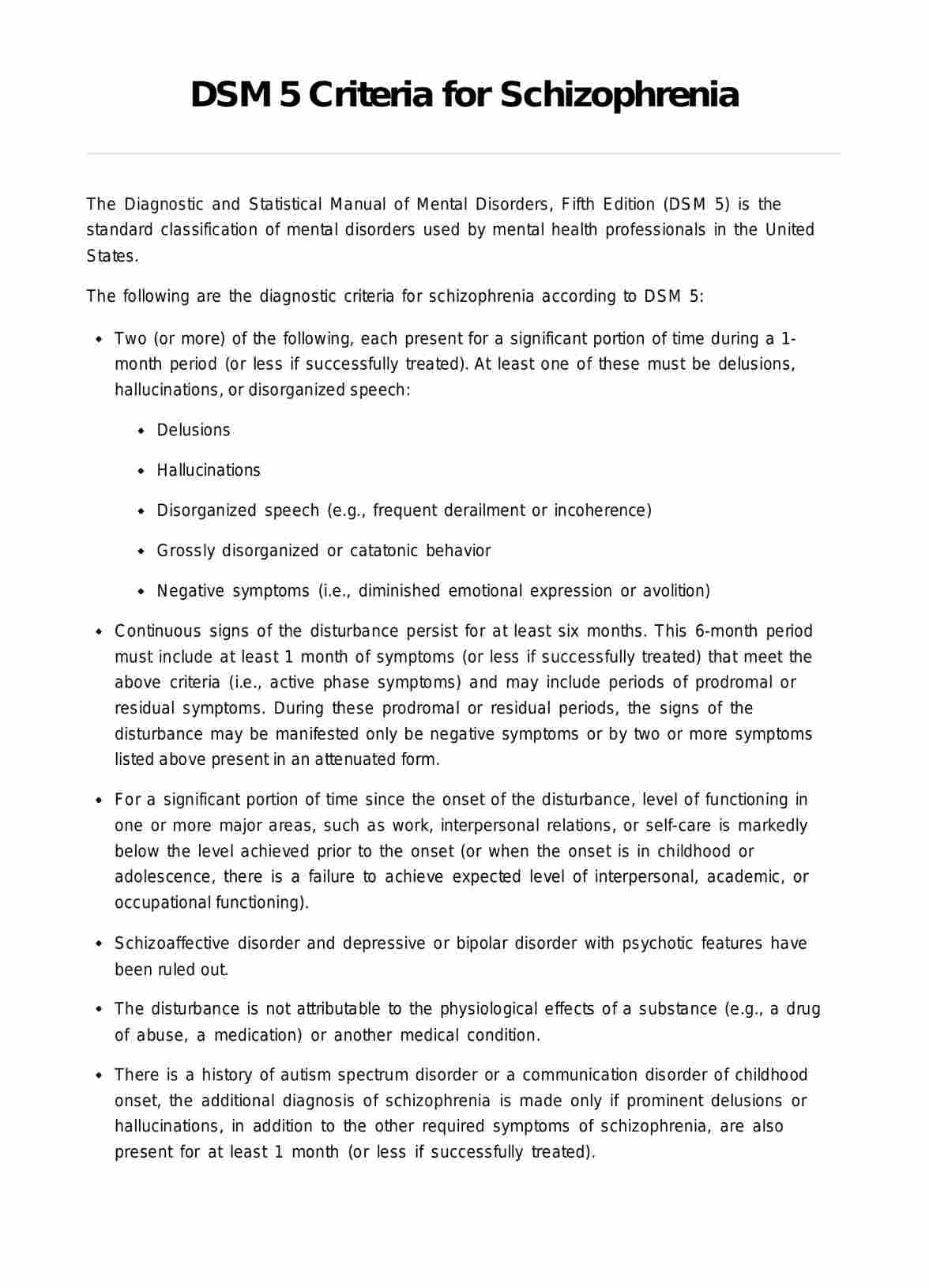
- Differential diagnosis: It's essential to differentiate PMDD from other mood disorders, such as major depressive disorder, bipolar disorder, or generalized anxiety disorder, as well as medical conditions that may mimic PMDD symptoms. A thorough medical and psychiatric evaluation may be necessary to rule out other possible causes of symptoms.
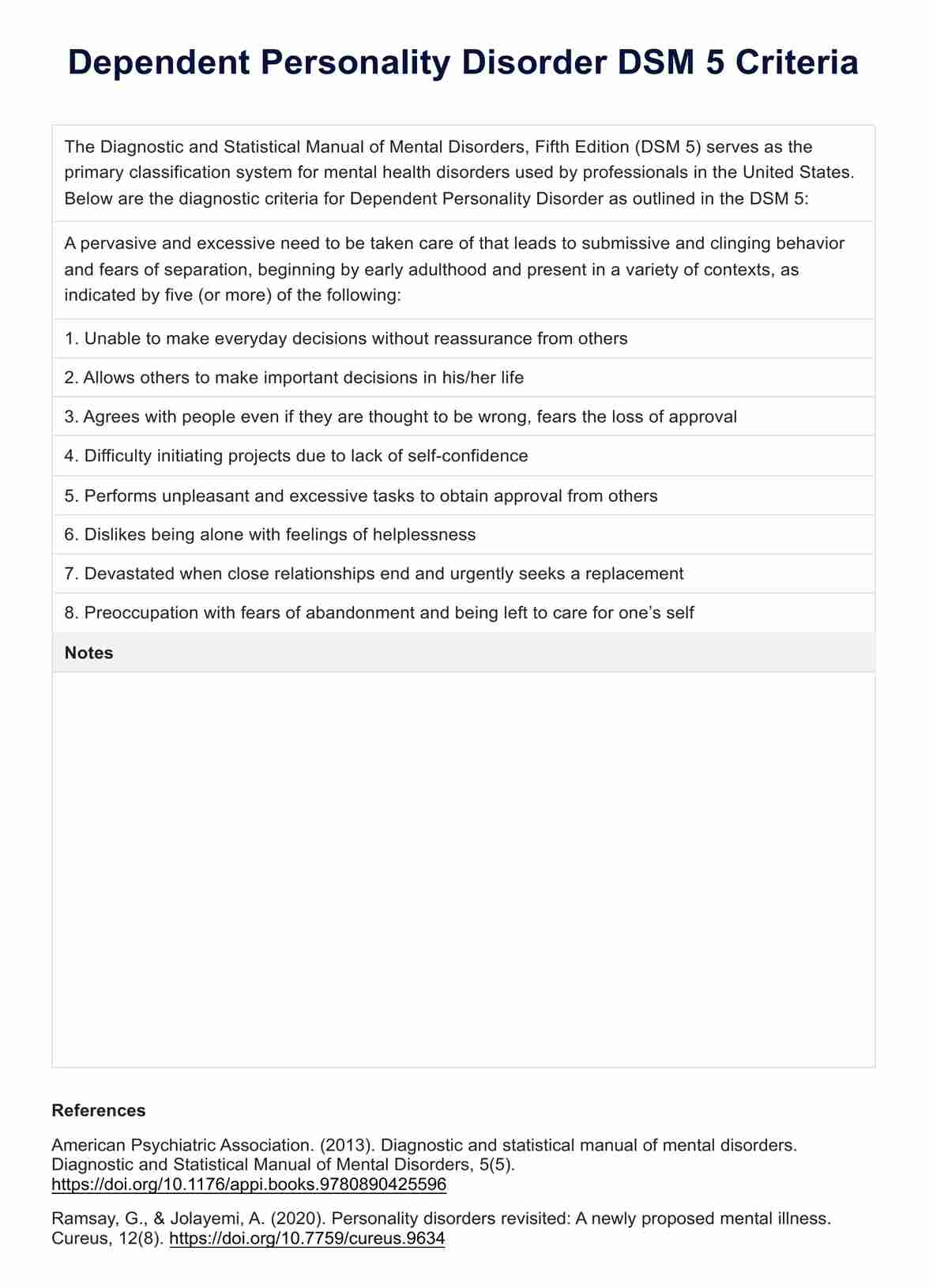
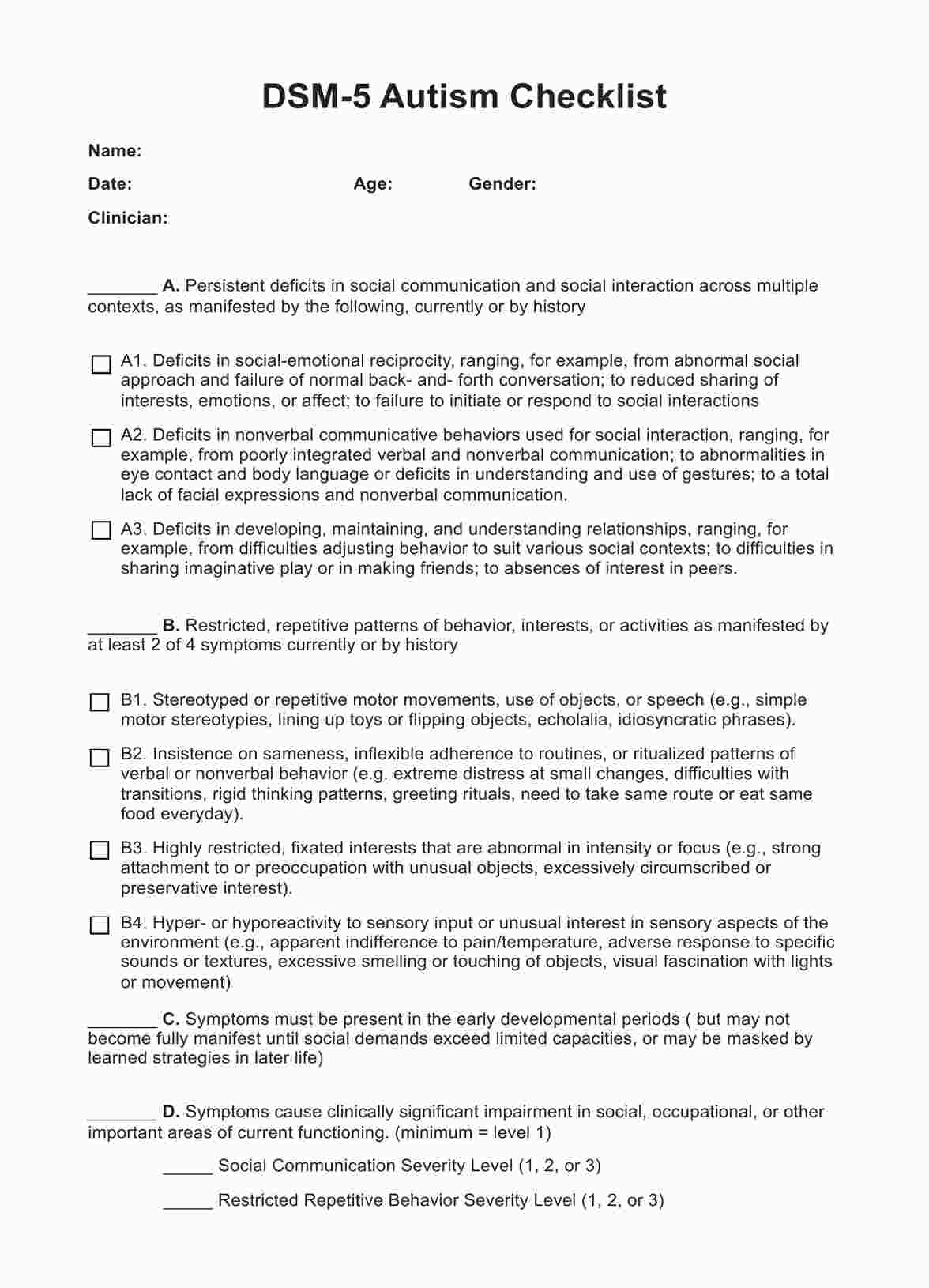
- Diagnostic criteria: PMDD is diagnosed based on specific criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).
- Collaboration: Collaboration between the individual and healthcare provider is essential in diagnosing PMDD. Open communication about symptoms, concerns, and treatment preferences helps ensure accurate diagnosis and appropriate management.
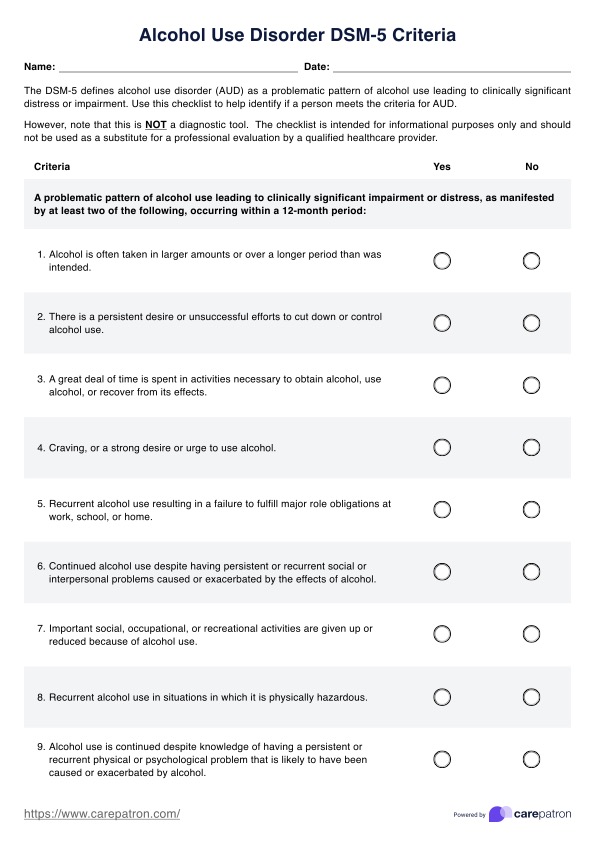
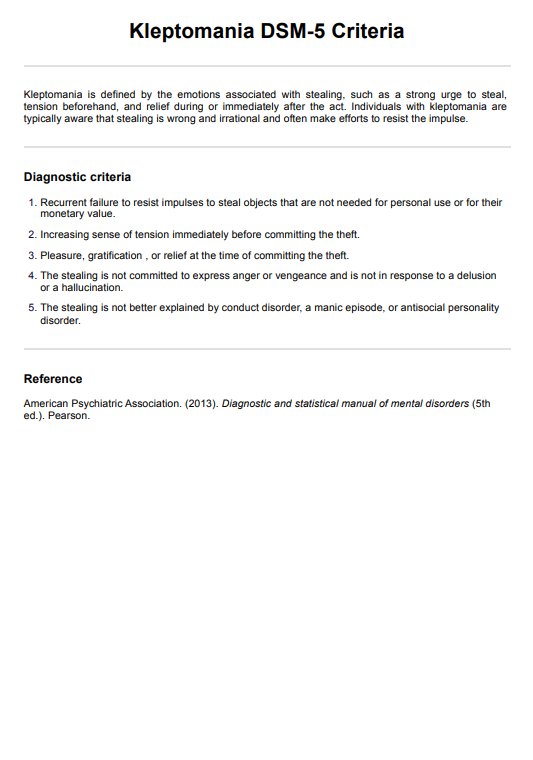
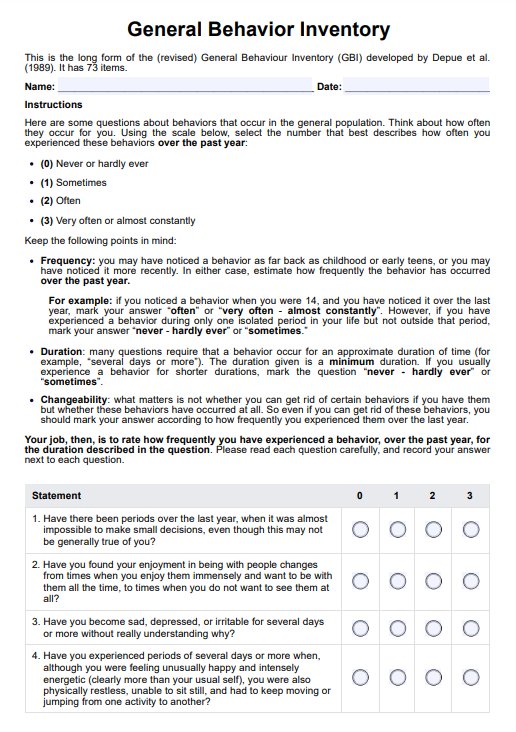
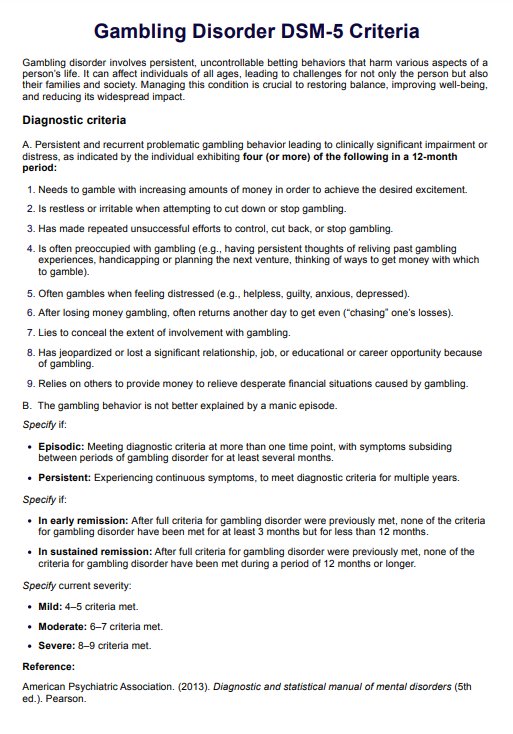
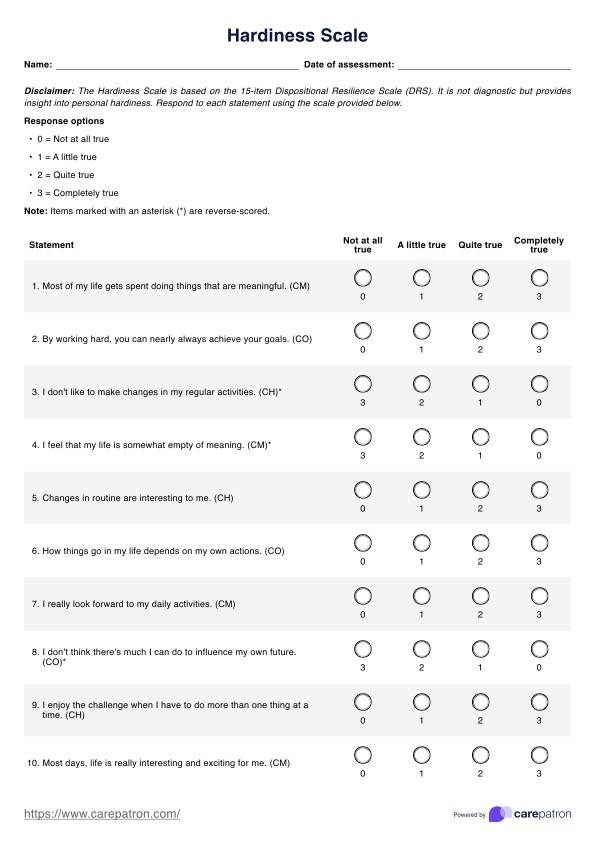
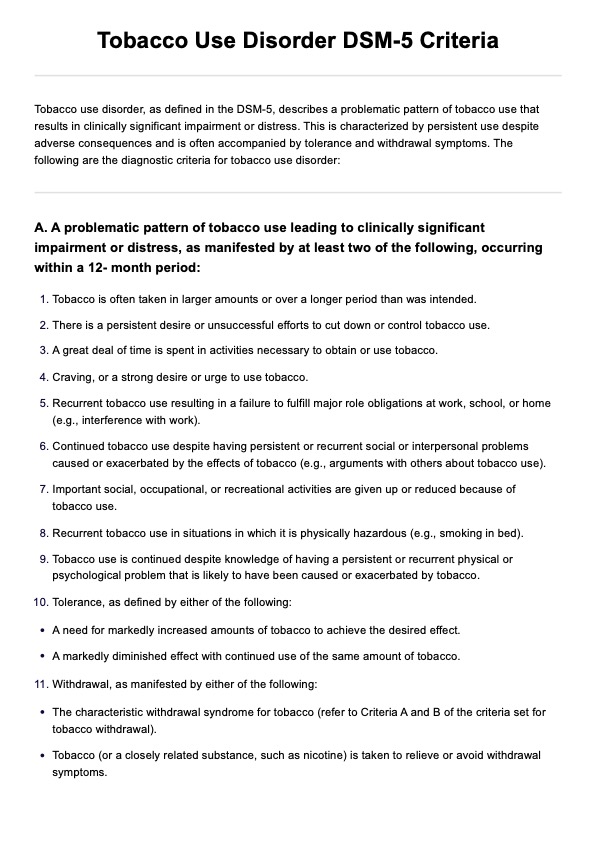
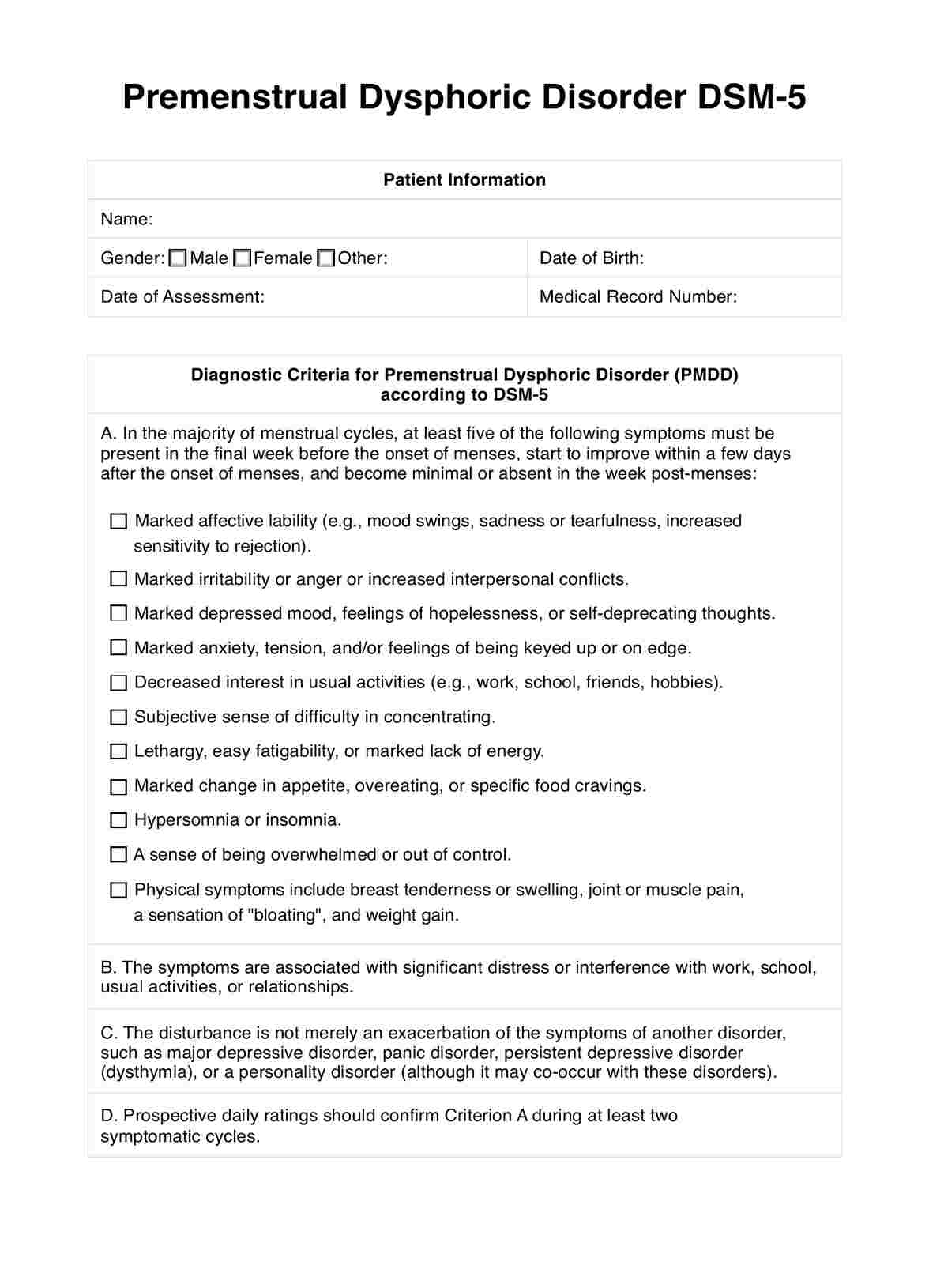
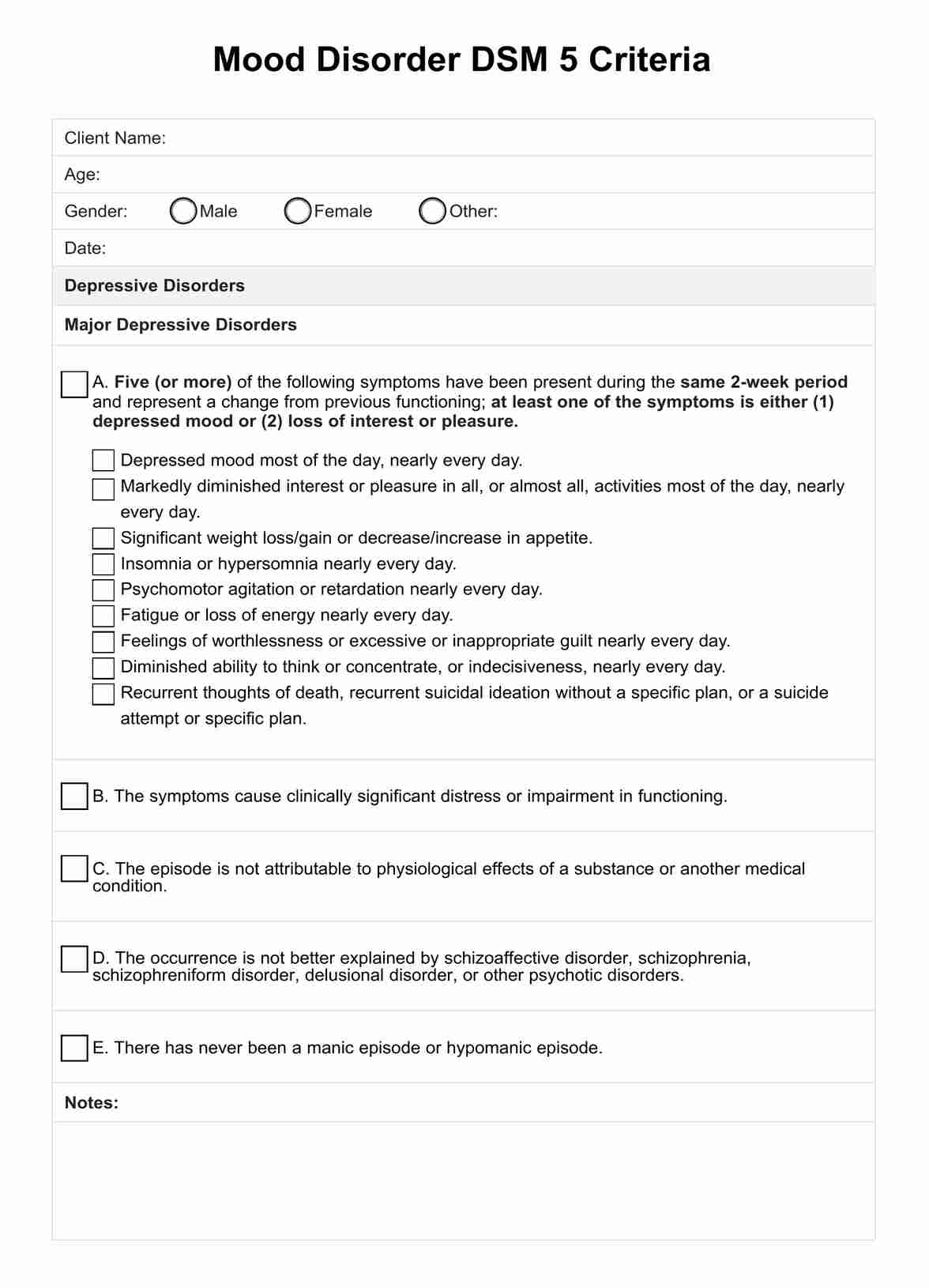
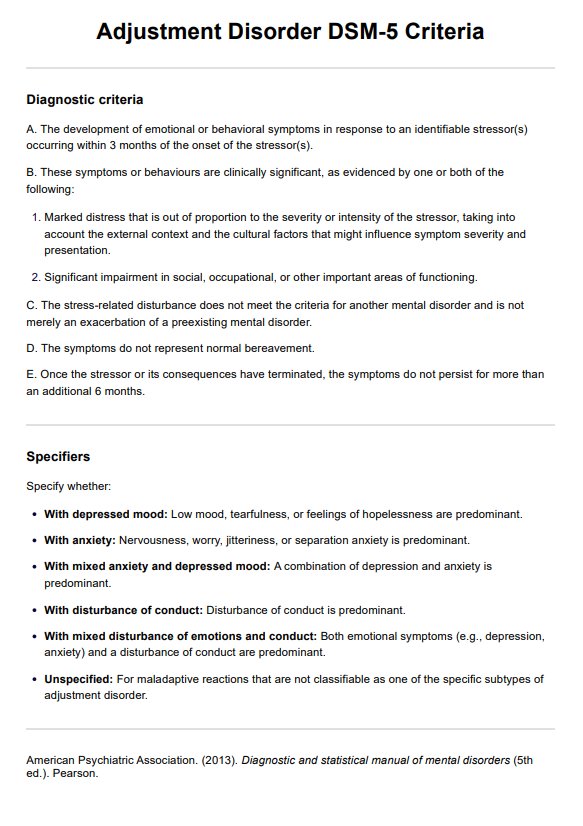
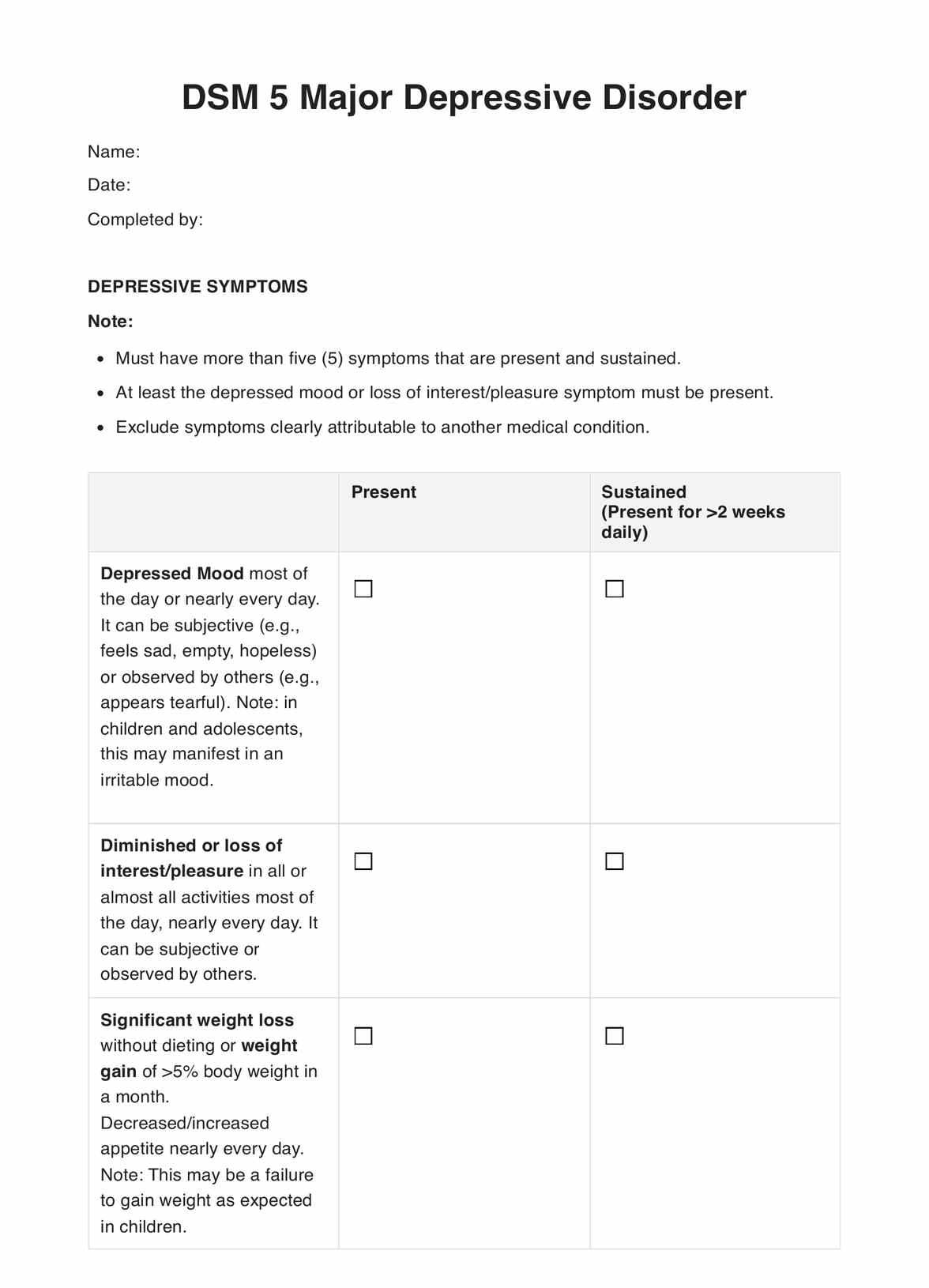
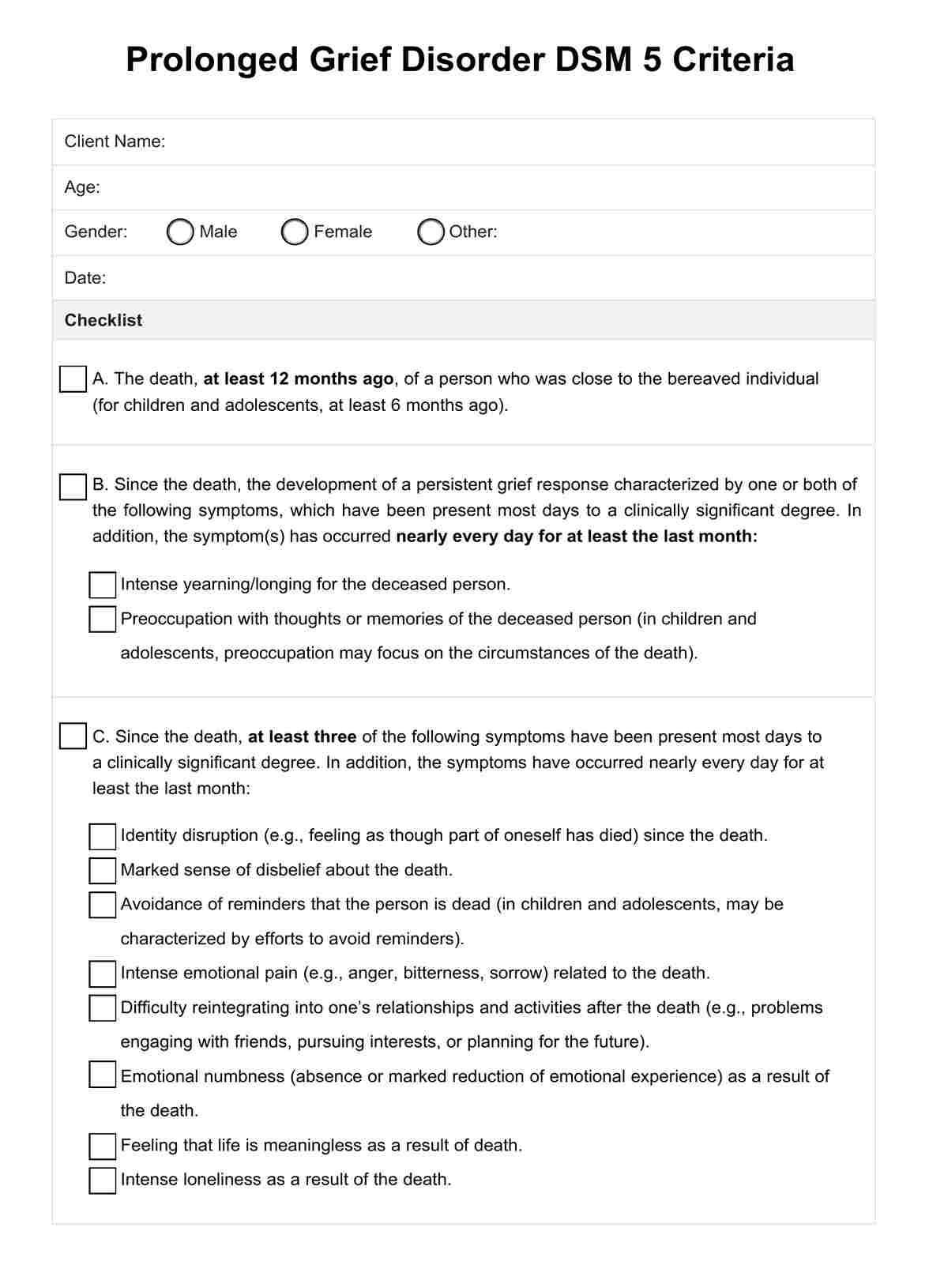
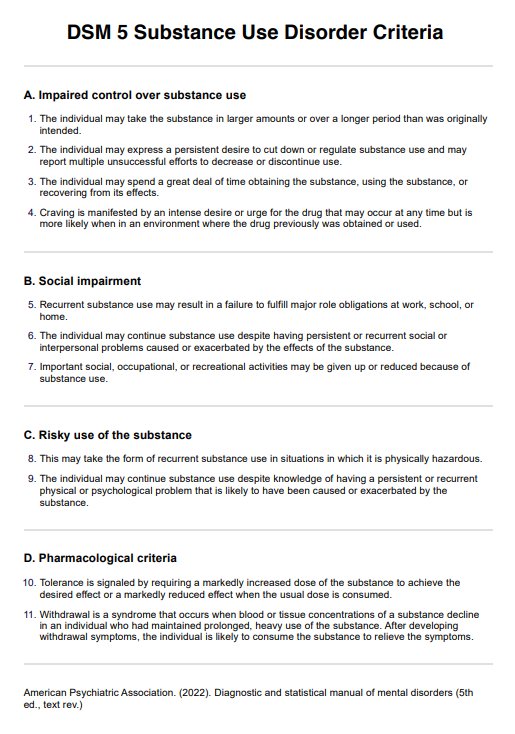
DSM-5 diagnostic criteria
To aid in diagnosis and treatment, the DSM-5 outlines specific criteria for identifying PMDD. These criteria encompass a range of emotional, behavioral, and physical symptoms that must be present during particular phases of the menstrual cycle. Below are the detailed diagnostic criteria according to the DSM-5:
- Criterion A: In the majority of menstrual cycles, at least 5 symptoms must be present in the final week before the onset of menses, start to improve within a few days after the onset of menses, and become minimal or absent in the week post menses.
- Criterion B: At least 1 of the following symptoms must be present:some text
- Marked affective lability (e.g., mood swings, feeling suddenly sad or tearful, or increased sensitivity to rejection)
- Marked irritability or anger or increased interpersonal conflicts
- Marked depressed mood, feelings of hopelessness, or self-deprecating thoughts
- Marked anxiety, tension, and feelings of being keyed up or on edge
- Criterion C: At least 1 of the following symptoms must additionally be present to reach a total of 5 symptoms when combined with symptoms from Criterion B above:some text
- Decreased interest in usual activities (e.g., work, school, friends, hobbies).
- Subjective difficulty in concentration
- Lethargy, easy fatiguability, or marked lack of energy
- Marked change in appetite, overeating, or specific food cravings
- Hypersomnia or insomnia
- A sense of being overwhelmed or out of control
- Physical symptoms such as breast tenderness or swelling, joint or muscle pain, a sensation of “bloating,” or weight gain
The symptoms in Criteria A-C must have been met for most menstrual cycles that occurred in the preceding year.
- Criterion D: The symptoms are associated with clinically significant distress or interference with work, school, usual social activities, or relationships with others. This may manifest as:some text
- Avoidance of social activities
- Decreased productivity and efficiency at work, school, or home
- Difficulty maintaining relationships due to mood swings or irritability
- Criterion E: The disturbance is not merely a worsening of the symptoms of another disorder, such as major depressive disorder, panic disorder, persistent depressive disorder (dysthymia), or a personality disorder (although it may co-occur with any of these disorders).
- Criterion F: Preview daily ratings should confirm '' Criterion A '' during at least 2 symptomatic cycles. The diagnosis may be made provisionally before this confirmation.
- Criterion G: The symptoms are not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication, or other treatment) or another medical condition (e.g., hyperthyroidism). This ensures that external factors do not cause the symptoms and are indeed related to premenstrual dysphoric disorder.
What are the treatment options for PMDD?
Treatment options for Premenstrual Dysphoric Disorder (PMDD) aim to alleviate symptoms, improve quality of life, and reduce the impact of PMDD on daily functioning. Treatment choice depends on the severity of symptoms, individual preferences, and medical history.
Here are some standard treatment options for PMDD:
Medications
- Selective serotonin reuptake inhibitors (SSRIs): Antidepressant medications such as fluoxetine (Prozac), sertraline (Zoloft), and paroxetine (Paxil) are often used as first-line treatment for PMDD. SSRIs can help reduce mood, irritability, and physical symptoms when taken continuously or during the luteal phase of the menstrual cycle.
- Oral contraceptives: Combined oral contraceptives containing estrogen and progestin may help regulate hormonal fluctuations and improve PMDD symptoms. Continuous or extended-cycle regimens may be particularly beneficial in reducing symptoms.
- Gonadotropin-releasing hormone (GnRH) Agonists: These medications suppress ovarian function and may be used in severe cases of PMDD that do not respond to other treatments. GnRH agonists are typically used short-term due to potential side effects and long-term implications for bone health.
Psychotherapy
- Cognitive-behavioral therapy (CBT): CBT can help individuals with PMDD learn coping skills, identify negative thought patterns, and develop strategies to manage mood symptoms and stressors. CBT techniques may include cognitive restructuring, relaxation training, and problem-solving skills.
- Interpersonal therapy (IPT): IPT focuses on improving interpersonal relationships and communication skills, which may be particularly helpful for addressing interpersonal conflicts and relationship stressors associated with PMDD.
Lifestyle modifications
- Regular exercise: Regular physical activity, such as aerobic exercise or yoga, can help improve mood, reduce stress, and alleviate PMDD symptoms.
- Dietary changes: Adopting a balanced diet rich in fruits, vegetables, whole grains, and lean proteins while minimizing caffeine, alcohol, and sugar intake may help regulate mood and energy levels.
- Stress management: Practicing relaxation techniques, such as deep breathing, meditation, or mindfulness, can help reduce stress and improve coping skills.
- Sleep hygiene: Establishing a regular sleep schedule, optimizing the sleep environment, and practicing good sleep hygiene habits can promote better sleep quality and overall well-being.
Alternative therapies
- Herbal supplements: Some individuals may relieve PMDD symptoms with herbal supplements such as chasteberry (Vitex agnus-castus), evening primrose oil, or St. John's wort. However, the evidence supporting the efficacy of these supplements is limited, and they may interact with other medications.
- Acupuncture: Acupuncture may help alleviate PMDD symptoms by promoting relaxation, reducing stress, and restoring balance to the body's energy flow. Research on the effectiveness of acupuncture for PMDD is ongoing.
Commonly asked questions
PMS involves mild to severe mood disorder with moderate symptoms like bloating and mood swings, while PMDD is a severe form with intense mood disturbances like irritability and depression.
PMDD is differentiated by its specific symptoms occurring in the late luteal phase and resolving shortly after menstruation, distinct from other mood disorders or menstrual conditions.
Yes, PMDD is classified as a mental illness in the DSM-5 due to its significant impact on mood and functioning during the menstrual cycle.












-template.jpg)