With proper treatment and management, an individual with HPD might see a significant improvement in their symptoms. The course of this condition can vary widely among individuals, and long-term management strategies are usually required.
Histrionic Personality Disorder DSM 5 PDF
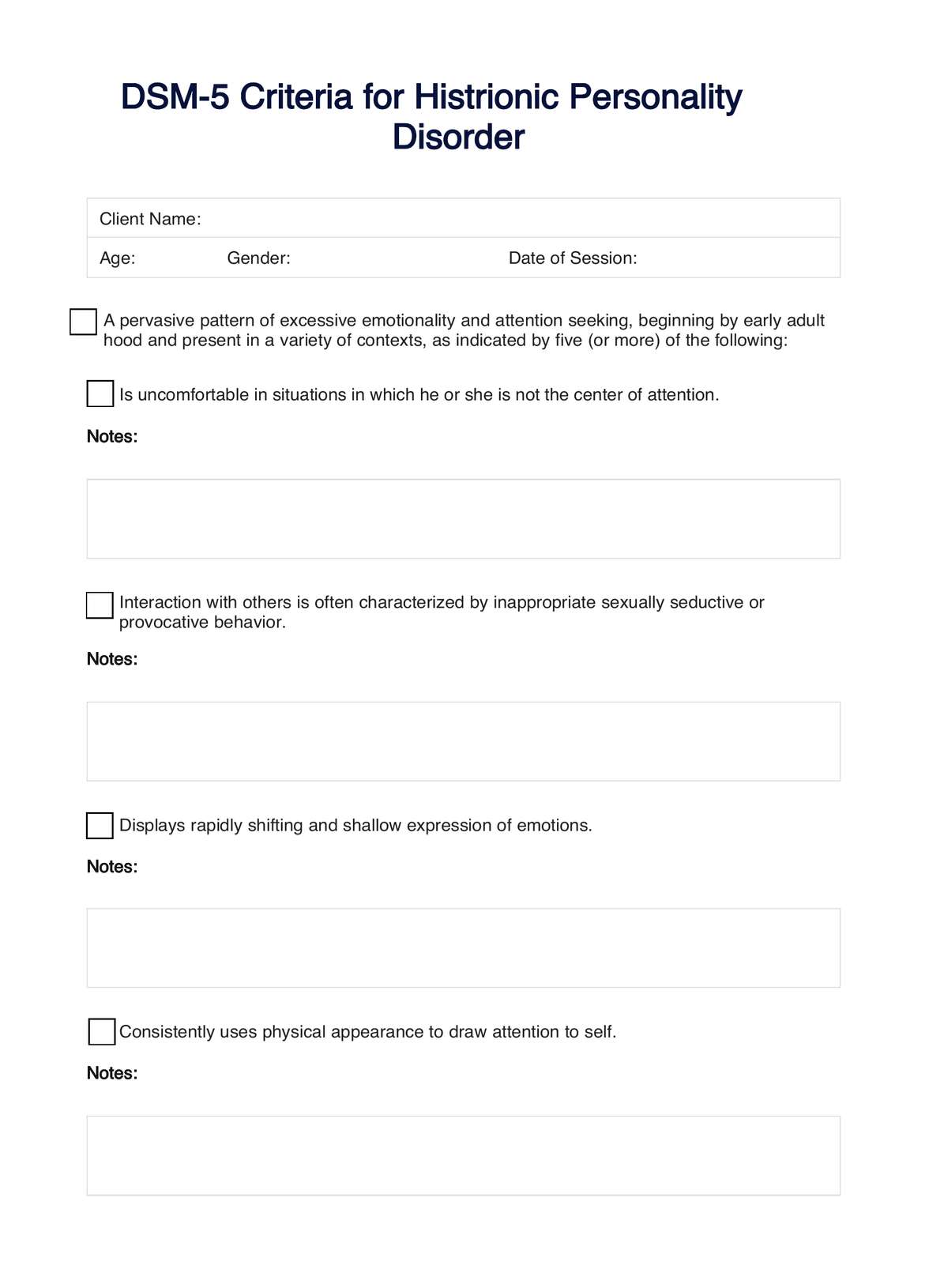
Access an evidence-based checklist of symptoms to screen for Histrionic Personality Disorder among clients. Download a free PDF here.
Use Template
Histrionic Personality Disorder DSM 5 PDF Template
Commonly asked questions
Cognitive-behavioral therapy and psychodynamic therapy are commonly used, focusing on increasing self-awareness and modifying negative thinking and behaviors.
Diagnosis uses the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) criteria through clinical interviews, psychological evaluations, and assessment of symptoms and behavior patterns.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











