DSM-5 Criteria for Mania
Explore DSM-5 criteria for bipolar mania, detailing symptoms, duration, and impairment, which are essential for understanding bipolar disorder diagnosis and treatment.


What is a manic episode?
A manic episode, often called "mania," is a distinct period characterized by an intense and elevated mood. This elevated mood typically lasts at least a week, though it can be shorter if hospitalization is required. Mania is a core feature of Bipolar I Disorder.
During a manic episode, individuals commonly experience a surge in energy levels, feelings of euphoria, or heightened irritability. They may also engage in impulsive or risky behaviors, such as excessive spending, reckless driving, or substance abuse.
These behaviors can significantly disrupt daily life and functioning. Manic episodes often alternate with periods of depression in individuals with bipolar disorder. Seeking professional help is crucial for managing mania, as untreated episodes can lead to severe consequences.
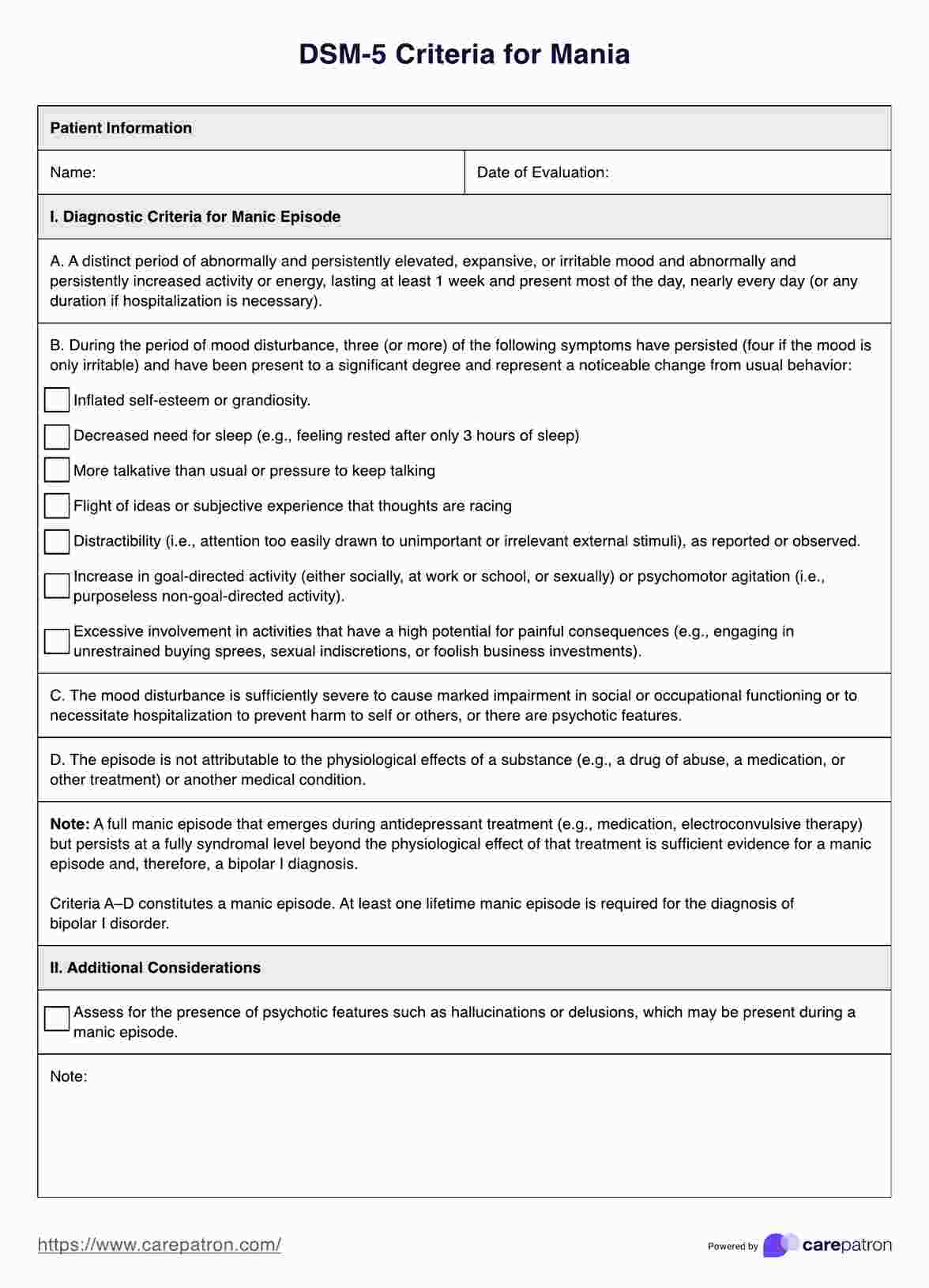
DSM-5 Criteria for Mania Template
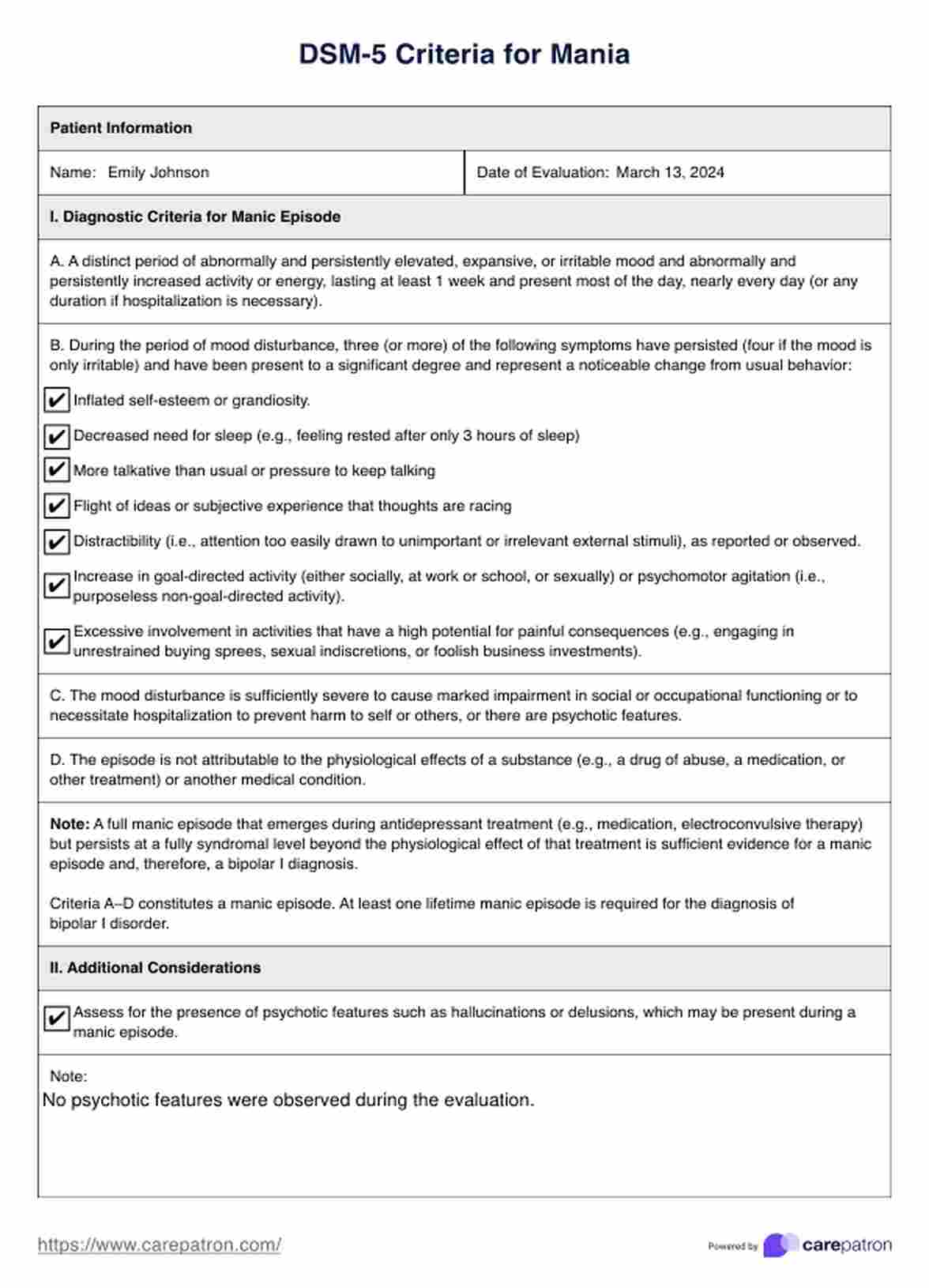
DSM-5 Criteria for Mania Example
What is bipolar disorder?
Bipolar disorder is a mental health condition characterized by extreme mood swings that include emotional highs (mania or hypomania) and lows (depression). These mood swings can affect sleep, energy levels, behavior, judgment, and the ability to think clearly. Bipolar disorder is a chronic illness, but with proper treatment, people with this condition can lead entire and productive lives.
Types of bipolar disorder include:
Bipolar I disorder
This type involves manic episodes that last at least seven days or are severe enough to require immediate hospital care. Depressive episodes typically occur as well, lasting at least two weeks. Some people may experience mixed episodes, which involve symptoms of both mania and depression simultaneously.
Bipolar II disorder
In this type, a person experiences a pattern of depressive episodes and hypomanic episodes (less severe than full-blown mania). Hypomanic episodes don't usually cause significant problems in social or work settings, but they can be noticeable to others.
Cyclothymic disorder (cyclothymia)
This type involves numerous periods of hypomanic symptoms as well as numerous periods of depressive symptoms lasting for at least two years (one year in children and adolescents). However, the symptoms do not meet the criteria for a hypomanic episode and a depressive episode.
Bipolar disorder affects both men and women and usually begins in late adolescence or early adulthood. The exact cause is unknown, but genetic, biological, and environmental factors likely contribute to its development. Treatment typically involves a combination of medication, psychotherapy, and lifestyle adjustments to manage symptoms and prevent relapses.
How to diagnose mania?
Understanding and diagnosing mania is essential in mental health, especially for conditions like bipolar disorder. Mental health professionals use standardized criteria to diagnose manic episodes. The DSM-5 outlines the requirements and describes the characteristics and duration of elevated mood and activity levels necessary for diagnosis.
Let us discuss the DSM-5 diagnostic criteria for mania and explore the process used by mental health professionals to diagnose manic episodes.
DSM-5 diagnostic criteria for mania
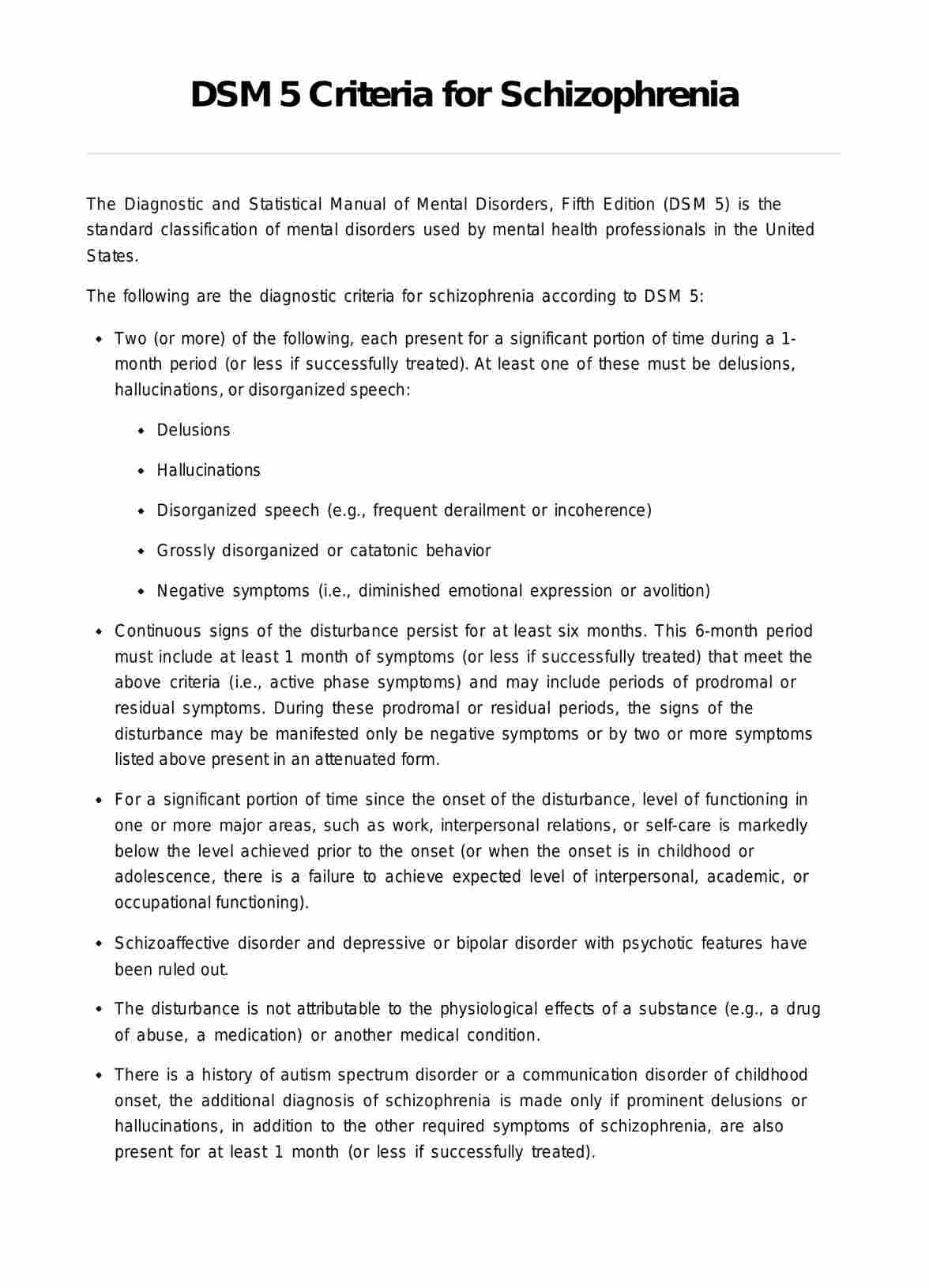
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), outlines the criteria for diagnosing mania as part of bipolar disorder. Here are the DSM-5 criteria for a manic episode:
A. A distinct period of abnormally and persistently elevated, expansive, or irritable mood and abnormally and persistently increased goal-directed activity or energy, lasting at least one week and present most of the day, nearly every day (or any duration if hospitalization is necessary).
B. During the period of mood disturbance and increased energy or activity, three (or more) of the following symptoms have persisted (four if the mood is only irritable) and have been present to a significant degree and represent a noticeable change from usual behavior:
- Inflated self-esteem or grandiosity.
- Decreased need for sleep (e.g., feeling rested after only three hours of sleep).
- More talkative than usual or pressure to keep talking.
- Flight of ideas or subjective experience that thoughts are racing.
- Distractibility (i.e., attention too easily drawn to unimportant or irrelevant external stimuli), as reported or observed.
- Increase in goal-directed activity (either socially, at work or school, or sexually) or psychomotor agitation (i.e., purposeless non-goal-directed activity).
- Excessive involvement in activities with a high potential for painful consequences (e.g., engaging in unrestrained buying sprees, sexual indiscretions, or foolish business investments).
C. The mood disturbance is sufficiently severe to cause marked impairment in social or occupational functioning or to necessitate hospitalization to prevent harm to self or others, or there are psychotic features.
D. The episode is not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication, or other treatment) or another medical condition.
A full manic episode that emerges during antidepressant treatment (e.g., medication, electroconvulsive therapy) but persists at a fully syndromal level beyond the physiological effect of that treatment is sufficient evidence for a manic episode and, therefore, a bipolar I diagnosis. Criteria A–D constitute a manic episode. At least one-lifetime manic episode is required for the diagnosis of bipolar I disorder.
What is the Diagnostic and Statistical Manual (DSM-5)?
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) is a reference book on mental health published by the American Psychiatric Association (APA). It serves as the main guide for mental health providers in the U.S., offering detailed definitions, signs, and symptoms of mental health conditions.
The DSM-5 is a resource that organizes various mental health conditions into groups to aid accurate diagnosis. It includes diagnostic codes for cross-referencing with the World Health Organization's International Classification of Diseases and Related Health Problems. The DSM-5 is a technical medical reference intended for experts and professionals, focusing on mental health and brain-related conditions (Cleveland Clinic).
Differential diagnosis: Psychiatric conditions mimicking mania in DSM-5
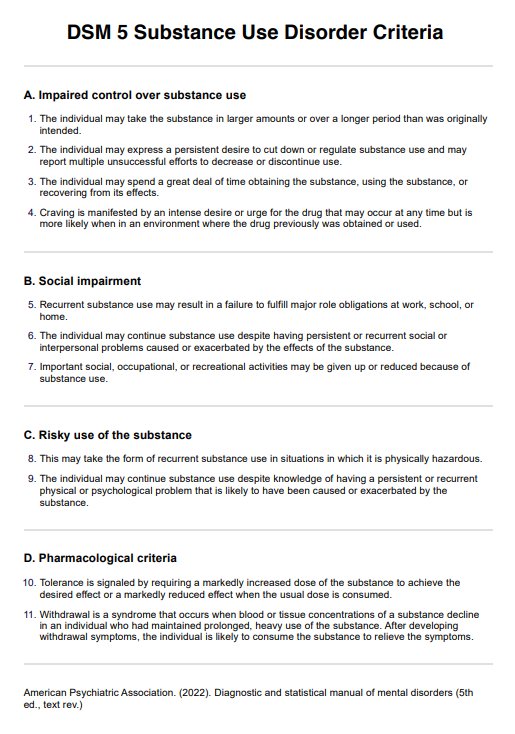
Consider medical mimics or secondary psychosis when diagnosing psychiatric conditions that mimic mania. These conditions can arise from substance abuse or preexisting physical health diagnoses, and the DSM-5 addresses this phenomenon through two diagnostic categories: substance-induced disorders and unspecified mental disorders due to another medical condition.
When evaluating a patient with an acute psychiatric presentation, a careful and consistent evaluation framework is crucial to minimize the risk of overlooking an underlying medical issue that may be causal. The DSM-5-TR Handbook of Differential Diagnosis is a guide that provides a six-step framework for diagnosing patients, starting with determining if the presenting symptoms are due to a substance/medication or a medical condition and ending with differentiating adjustment disorders from other mental disorders.
It is essential to consider medical mimics that may present with symptoms such as confusion, disorientation, agitation, mood lability, hallucinations, and delusions. These symptoms may be multifactorial and require a thorough medical evaluation to ensure accurate diagnosis and treatment. The DSM-5 offers decision trees and differential diagnosis tables that provide detailed decision points and head-to-head comparisons of each disorder, highlighting similarities and differences.
Several psychiatric conditions can mimic the symptoms of mania, bipolar, and related disorders, making a differential diagnosis crucial. Here are some psychiatric conditions to consider:
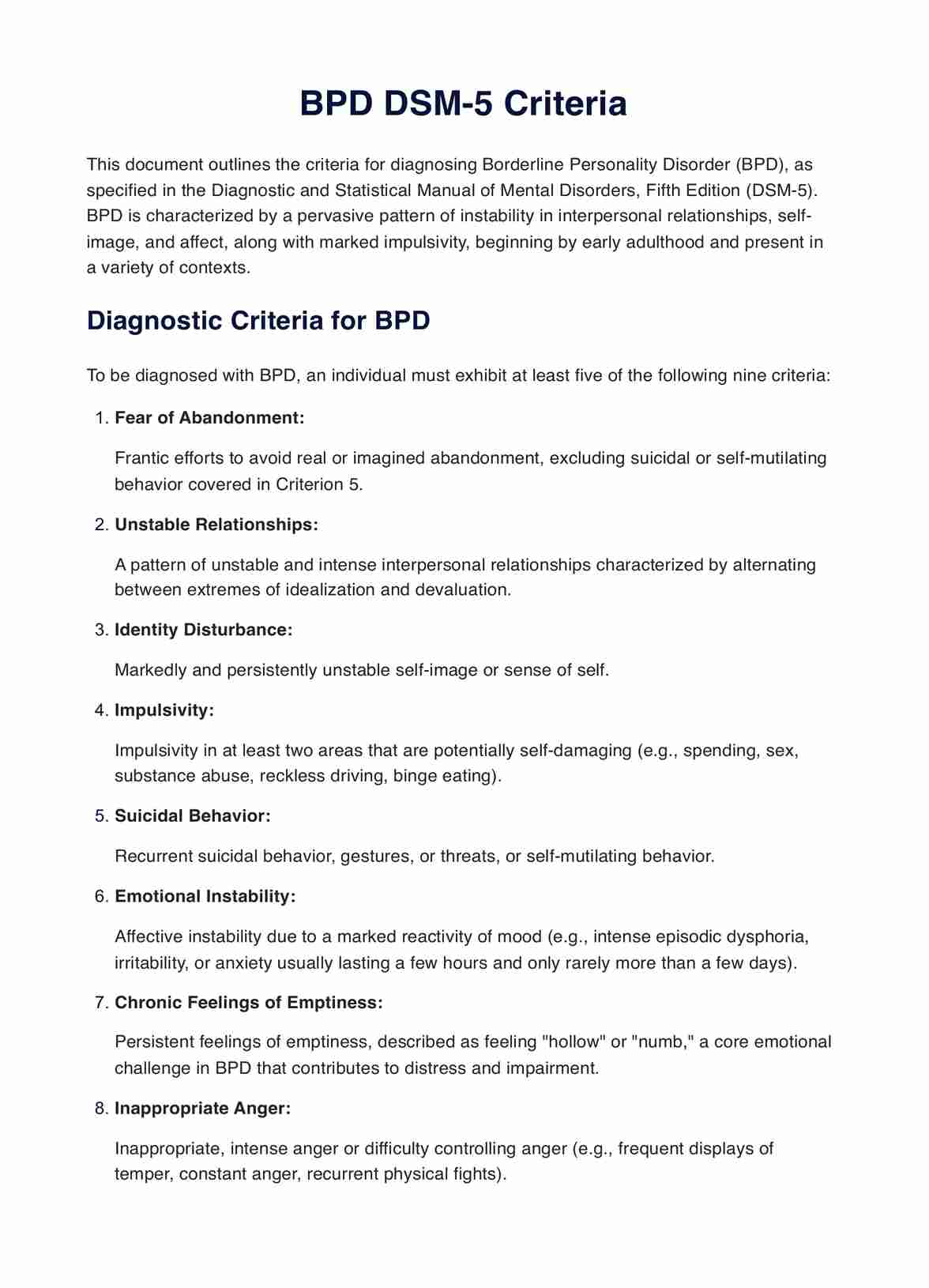
- Borderline personality disorder (BPD): Individuals with BPD may experience mood swings, impulsivity, and intense emotions, which can resemble manic symptoms. However, in BPD, these symptoms typically occur in response to interpersonal stressors and lack the distinct periods of elevated mood characteristic of manic episodes.
- Attention-deficit/hyperactivity disorder (ADHD): ADHD can present with impulsivity, distractibility, and hyperactivity, which may overlap with symptoms of mania. However, individuals with ADHD typically do not experience the distinct periods of elevated mood seen in bipolar disorder.
- Generalized anxiety disorder (GAD): While anxiety disorders like GAD can co-occur with bipolar disorder, excessive worry, restlessness, and irritability in GAD may be mistaken for symptoms of mania. However, in GAD, the mood disturbances are not as intense or prolonged as in manic episodes.
- Narcissistic personality disorder (NPD): Individuals with NPD may exhibit grandiosity, inflated self-esteem, and a need for admiration, which can resemble symptoms of mania. However, these traits are persistent and part of their personality rather than episodic mood disturbances.
Differences between DSM-IV and DSM-5 criteria for manic episodes
The main differences between the DSM-IV and DSM-5 criteria for a manic episode are as follows:
- Name and class: In DSM-IV, Bipolar I Disorder with a Single Manic Episode is classified under Bipolar Disorders. However, in DSM-5, Bipolar I Disorder with a Manic Episode is categorized under Bipolar and Related Disorders.
- Criteria changes: DSM-IV requires a distinct period of abnormally elevated mood lasting at least 1 week, while DSM-5 adds the requirement of persistently increased goal-directed behavior or energy, lasting at least 1 week and present most of the day, nearly every day. DSM-5 specifies that the symptoms must represent a noticeable change from usual behavior (Substance Abuse and Mental Health Services Administration).
- Symptom: DSM-5 includes distractibility as a symptom criterion, in addition to the existing criteria like inflated self-esteem, decreased need for sleep, talkativeness, flight of ideas, increased goal-directed activity, and excessive involvement in pleasurable activities with potentially negative consequences.
- Exclusion: DSM-IV had an exclusion criterion related to manic-like episodes caused by somatic antidepressant treatment, which DSM-5 revised to focus on episodes not attributable to the direct physiological effects of substances or medical conditions.
- Severity and impairment: DSM-IV emphasizes marked impairment in occupational functioning or social activities, while DSM-5 specifies marked impairment in social or occupational functioning or the need for hospitalization to prevent harm to self or others or the presence of psychotic features.
These changes reflect a more detailed and refined approach in DSM-5, aiming to improve diagnostic accuracy and provide more precise guidelines for identifying and diagnosing manic episodes in individuals.
Commonly asked questions
Mania involves more severe psychotic symptoms and can cause a significant degree of impairment in social or occupational functioning, often requiring hospitalization. Hypomania, on the other hand, has similar symptoms but to a lesser extent and does not lead to marked impairment or hospitalization.
Mania is a symptom characteristic of bipolar disorder, which is a separate mental health condition. However, it can also occur in other situations, such as bipolar disorders such as schizoaffective disorder, substance-induced mood disorder, or as a feature of medical conditions like hyperthyroidism.
The exact causes of mania are not fully understood but likely involve a combination of genetic, biological, and environmental factors. Imbalances in neurotransmitters such as dopamine and serotonin, genetic predisposition, stressful life events, and disruptions in sleep-wake cycles may contribute to the onset of manic episodes.
















-template.jpg)



















































































