DSM 5 Criteria for Anorexia Nervosa
Learn the DSM 5 criteria for Anorexia Nervosa, including diagnostic features and characteristic symptoms. Get a free PDF download for your reference.


What is anorexia nervosa?
Anorexia nervosa is a serious eating disorder characterized by an intense fear of gaining weight and a distorted body image that leads individuals to see themselves as overweight even when they have significantly low body weight. This condition drives people to engage in extreme behaviors to lose weight or prevent weight gain, regardless of the health consequences.
Unlike other eating disorders that may involve binge eating followed by purging, individuals with anorexia nervosa typically maintain a severely restricted diet, and any weight gain is met with extreme distress.
Moreover, anorexia nervosa is not a choice or a lifestyle but rather a serious mental illness that requires proper diagnosis and treatment. According to the Diagnostic and Statistical Manual (DSM 5), an individual must meet specific criteria to be diagnosed with anorexia nervosa.
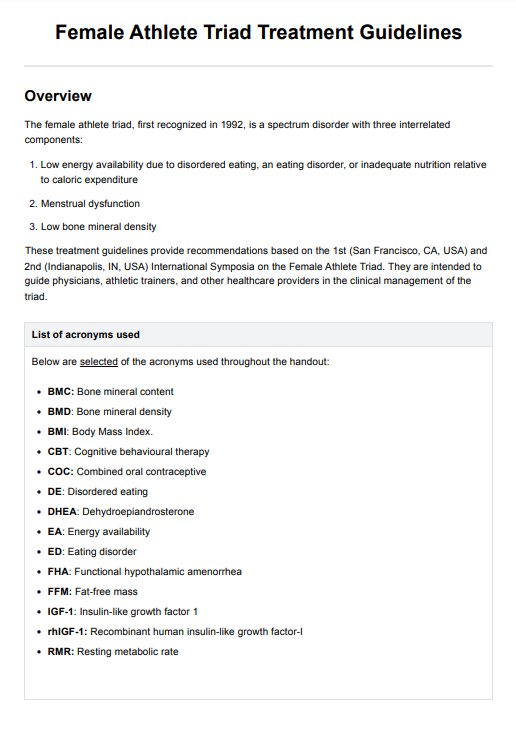
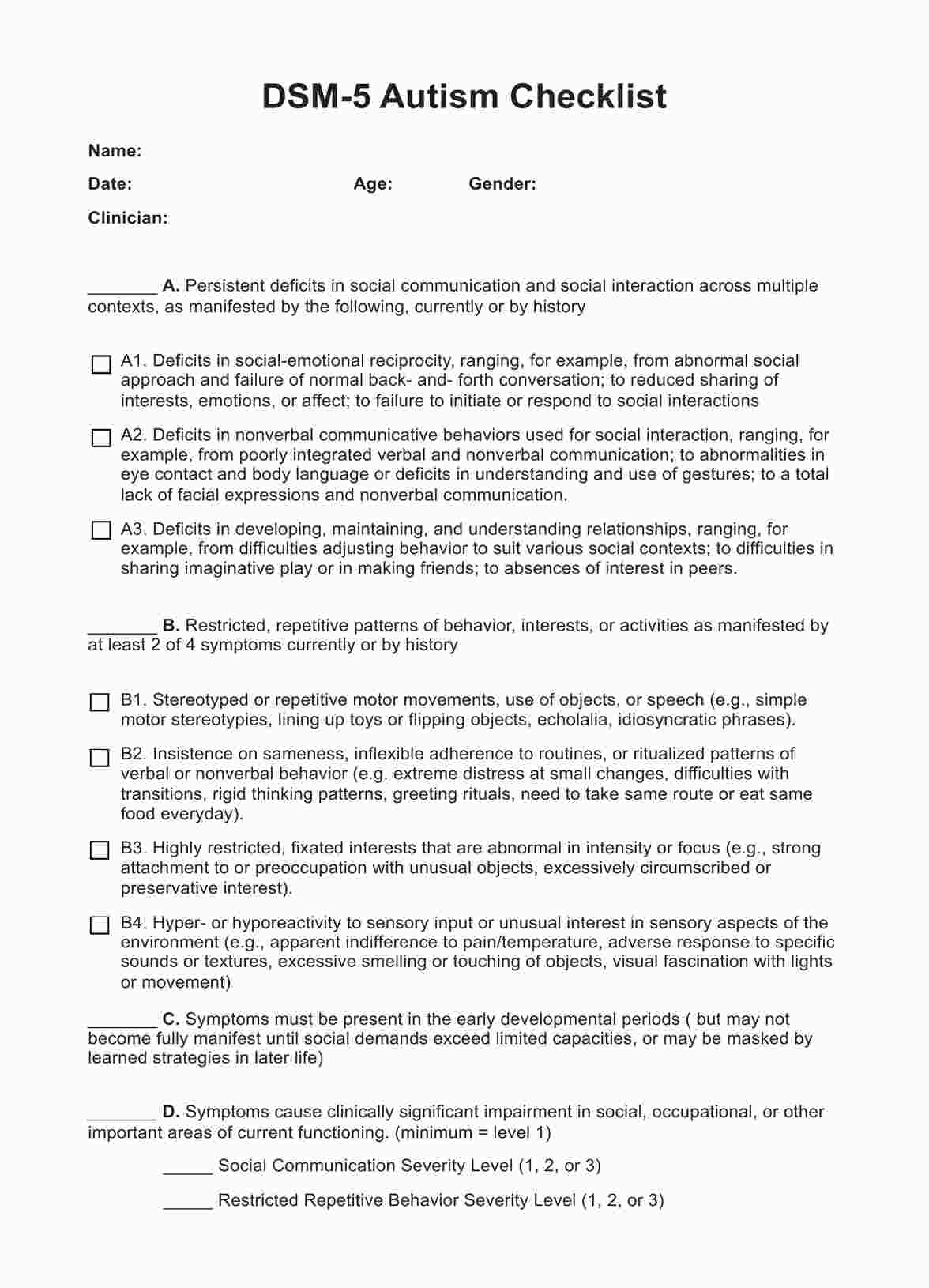
DSM 5 Criteria for Anorexia Nervosa Template
DSM 5 Criteria for Anorexia Nervosa Example
Causes and symptoms
The exact cause of anorexia nervosa is unknown, but experts believe that a combination of biological, environmental, and psychological factors may contribute to its development. Some potential risk factors include genetics, trauma or abuse, societal pressure to be thin, and certain personality traits such as perfectionism (Moore & Bokor, 2023).
Symptoms of anorexia nervosa often include:
- Significant weight loss or failure to gain weight during a period of growth, leading to an abnormally low body weight
- Intense fear of gaining weight or becoming fat, even when underweight
- Distorted body image and self-worth heavily influenced by body shape and weight
- Amenorrhea (absence of at least three menstrual cycles) in females who have reached puberty
- Obsessive thoughts and behaviors related to food include counting calories, avoiding certain foods, or strict meal rituals
- Extreme exercise routines despite exhaustion or injury
If left untreated, anorexia nervosa can lead to severe physical and mental health consequences. These may include:
- Malnutrition and vitamin deficiencies can cause damage to organs and systems in the body
- Cardiovascular problems, such as low heart rate and blood pressure, which can be life-threatening
- Osteoporosis or bone loss due to a lack of nutrients and hormones that maintain bone density
- Anemia and other blood disorders
- Gastrointestinal issues like constipation, bloating, and gastroparesis (delayed emptying of the stomach)
- Weakened immune system, leading to increased risk of infections and illnesses
- Depression, anxiety, and other mental health disorders
- Suicidal thoughts or behaviors
Societal influences on anorexia
While various factors contribute to the development of anorexia nervosa, societal pressures and influences play a significant role. The constant bombardment of unrealistic beauty standards, the glorification of thinness, and the stigmatization of overweight individuals can all contribute to the development of disordered eating behaviors.
Additionally, certain industries, such as fashion and modeling, have been known to perpetuate these harmful societal ideals, leading individuals to believe that their worth is solely based on their appearance and body size.
It is essential to recognize and challenge these societal influences, as well as promote body positivity and diversity, in order to prevent and reduce the prevalence of anorexia nervosa. Education and awareness are crucial in breaking down harmful beauty standards and promoting a more inclusive and accepting society.
The role of family dynamics
In some instances, family dynamics can significantly influence the development of anorexia nervosa. Within a dysfunctional family setting characterized by heightened levels of conflict, frequent criticism, or excessively controlling behaviors, individuals may experience a decline in self-esteem and harbor feelings of inadequacy, exacerbating the disorder.
Moreover, specific family dynamics can perpetuate disordered eating habits. For instance, continuous remarks about weight and appearance or rigid dietary restrictions may reinforce unhealthy behaviors.
Additionally, family members may also unknowingly contribute to the development of anorexia nervosa by placing excessive emphasis on external success and achievement, leading individuals to equate thinness with success and worth.
Treatment
Treatment for anorexia nervosa often involves a multidisciplinary approach, including medical professionals such as doctors, dietitians, therapists, and psychiatrists. The main goal is to restore the individual's physical health, address any psychological issues, and promote healthy eating habits and self-esteem.
The treatment plan may involve therapy, medication, and nutritional counseling. Cognitive behavioral therapy (CBT) is commonly used to help patients identify and change negative thoughts and behaviors associated with their eating disorder. Family-based therapy may also be recommended for younger patients, involving the family in the treatment process and addressing any underlying family issues.
In severe cases, hospitalization or residential treatment may be necessary to monitor weight restoration and ensure proper nutrition. Medications may also be prescribed to help manage symptoms such as depression, anxiety, or obsessive-compulsive tendencies.
Recovery from anorexia nervosa is a long and difficult journey, but with proper treatment and support, individuals can overcome this eating disorder and lead a healthy, fulfilling life. Continued therapy and regular check-ins with medical professionals can help prevent relapse and maintain recovery.
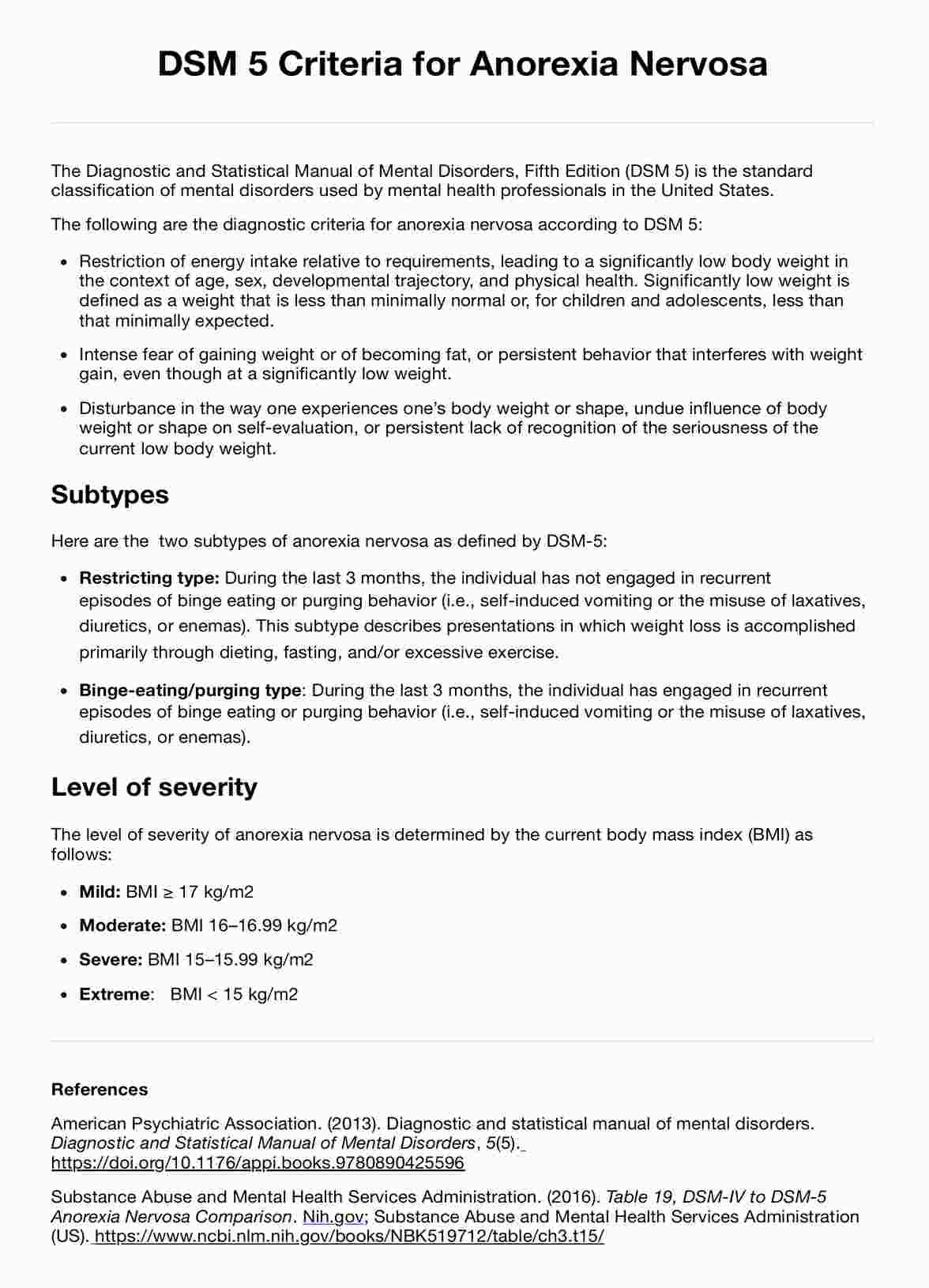
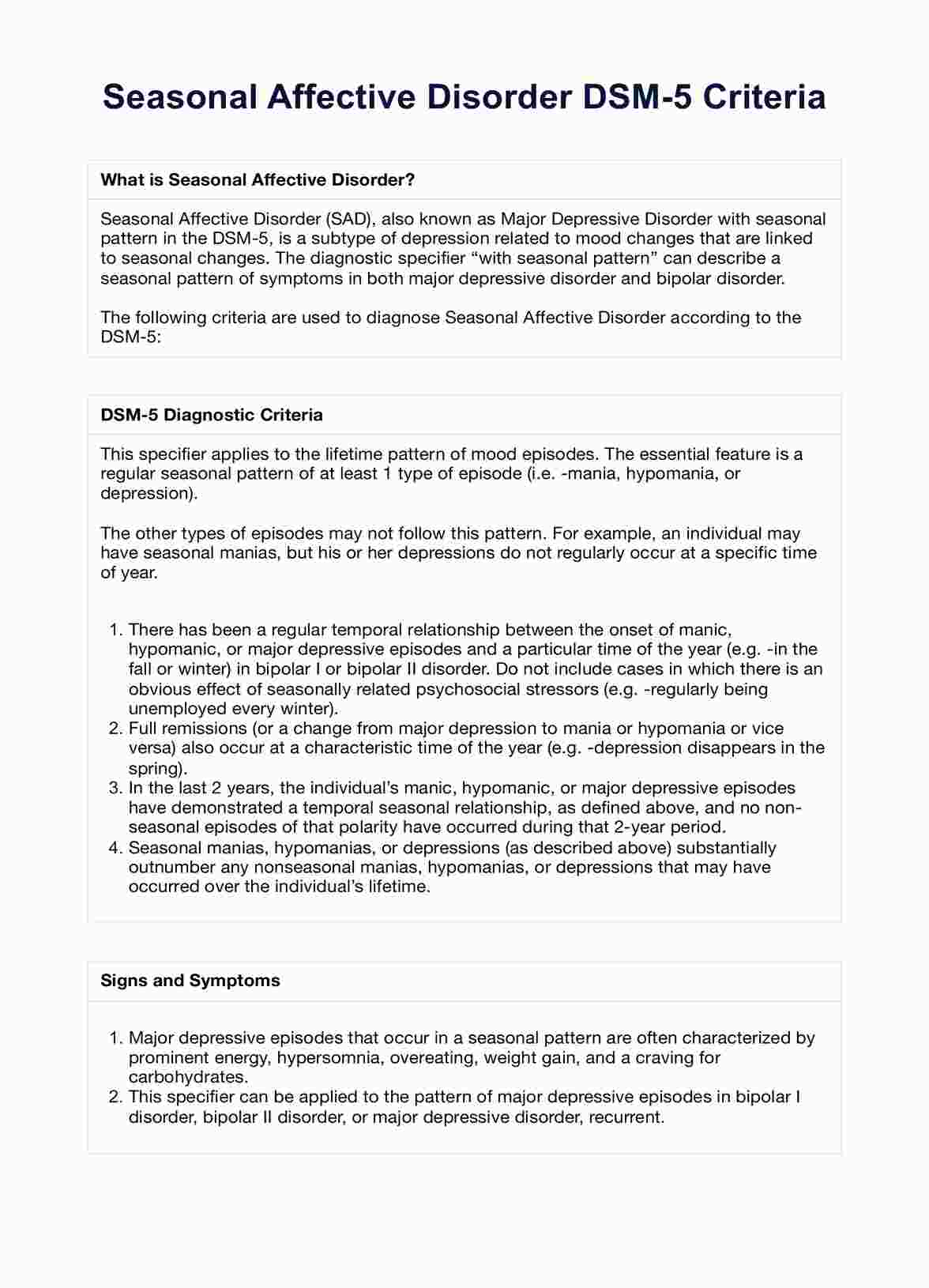
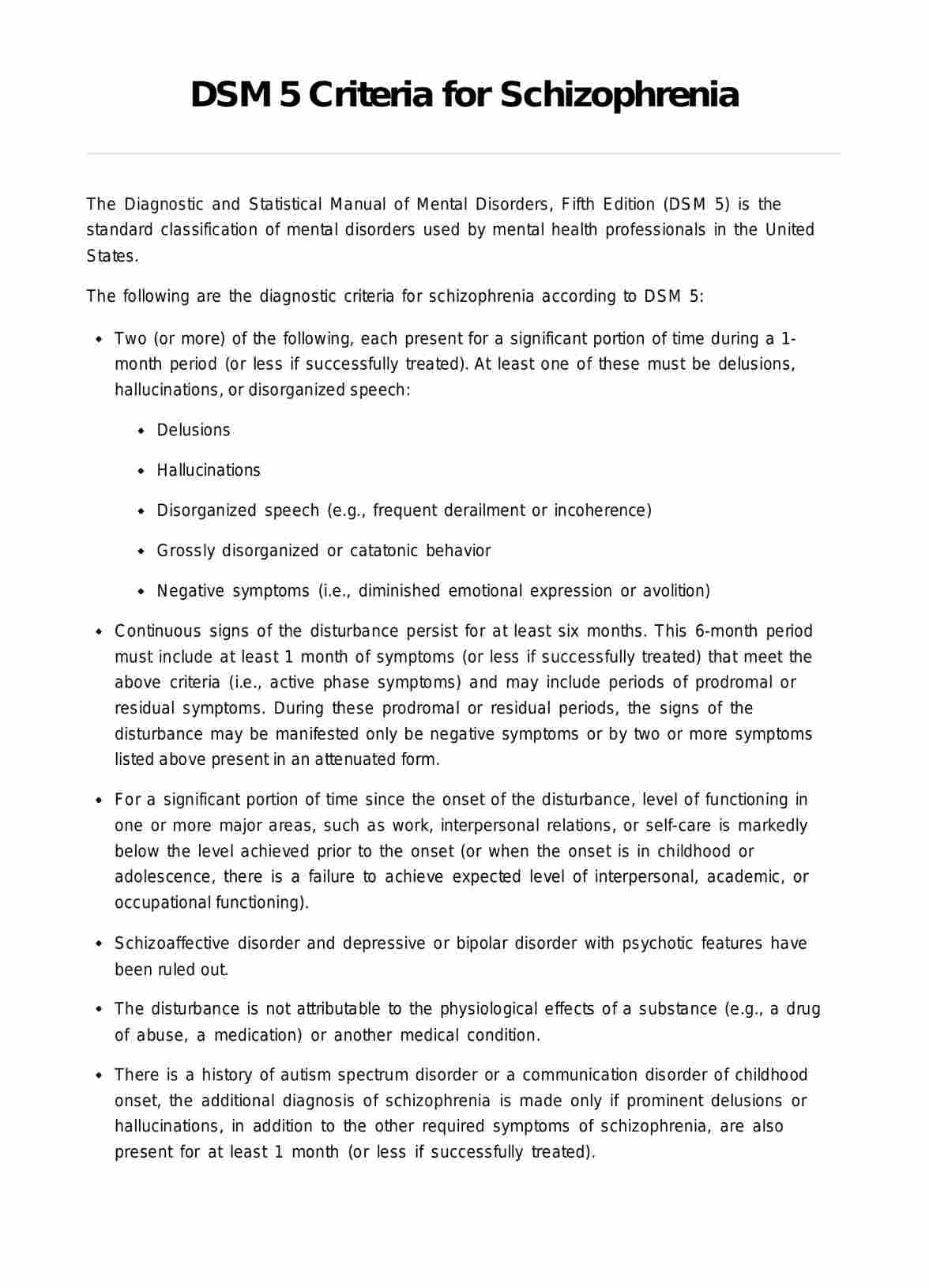
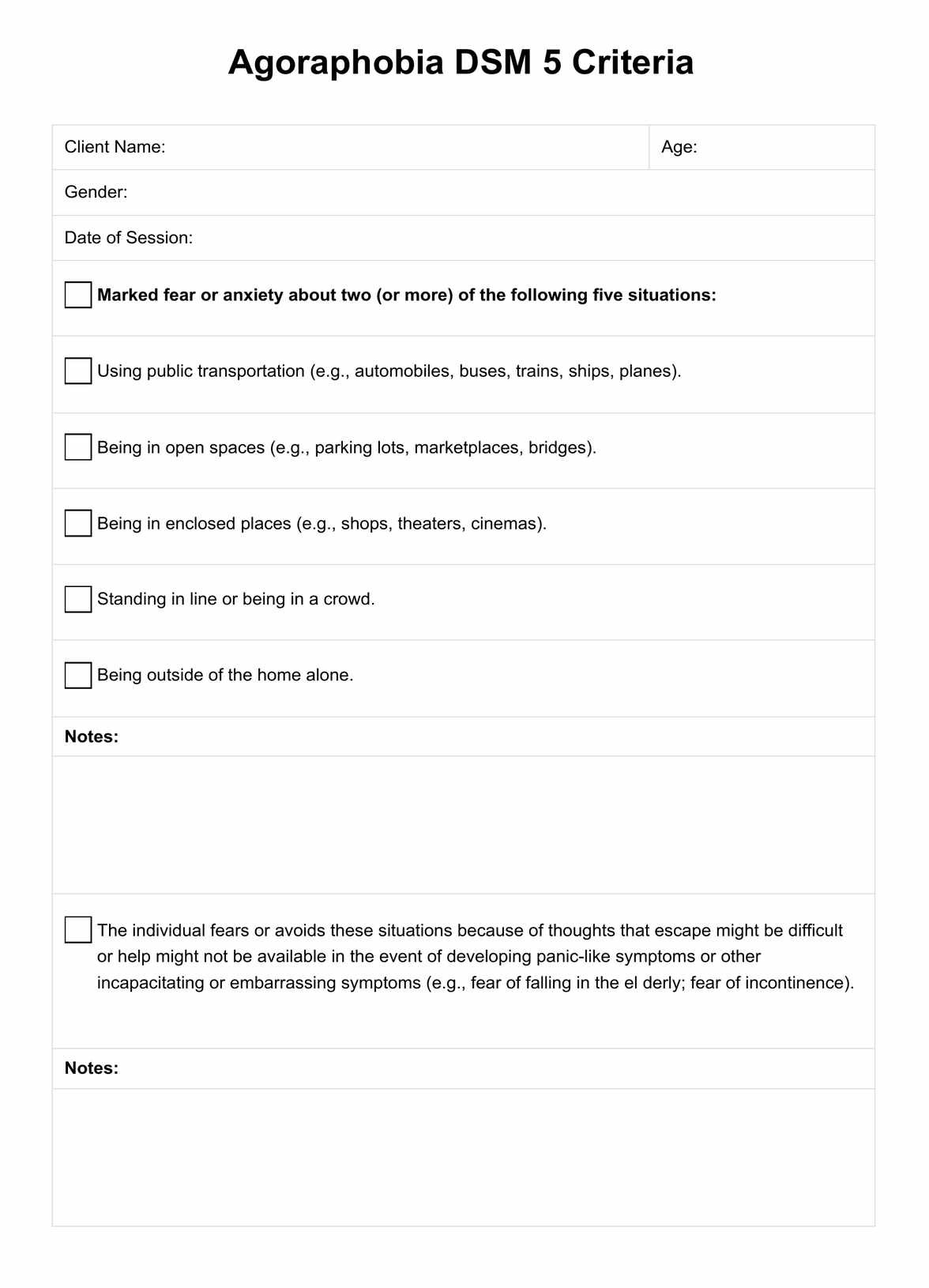
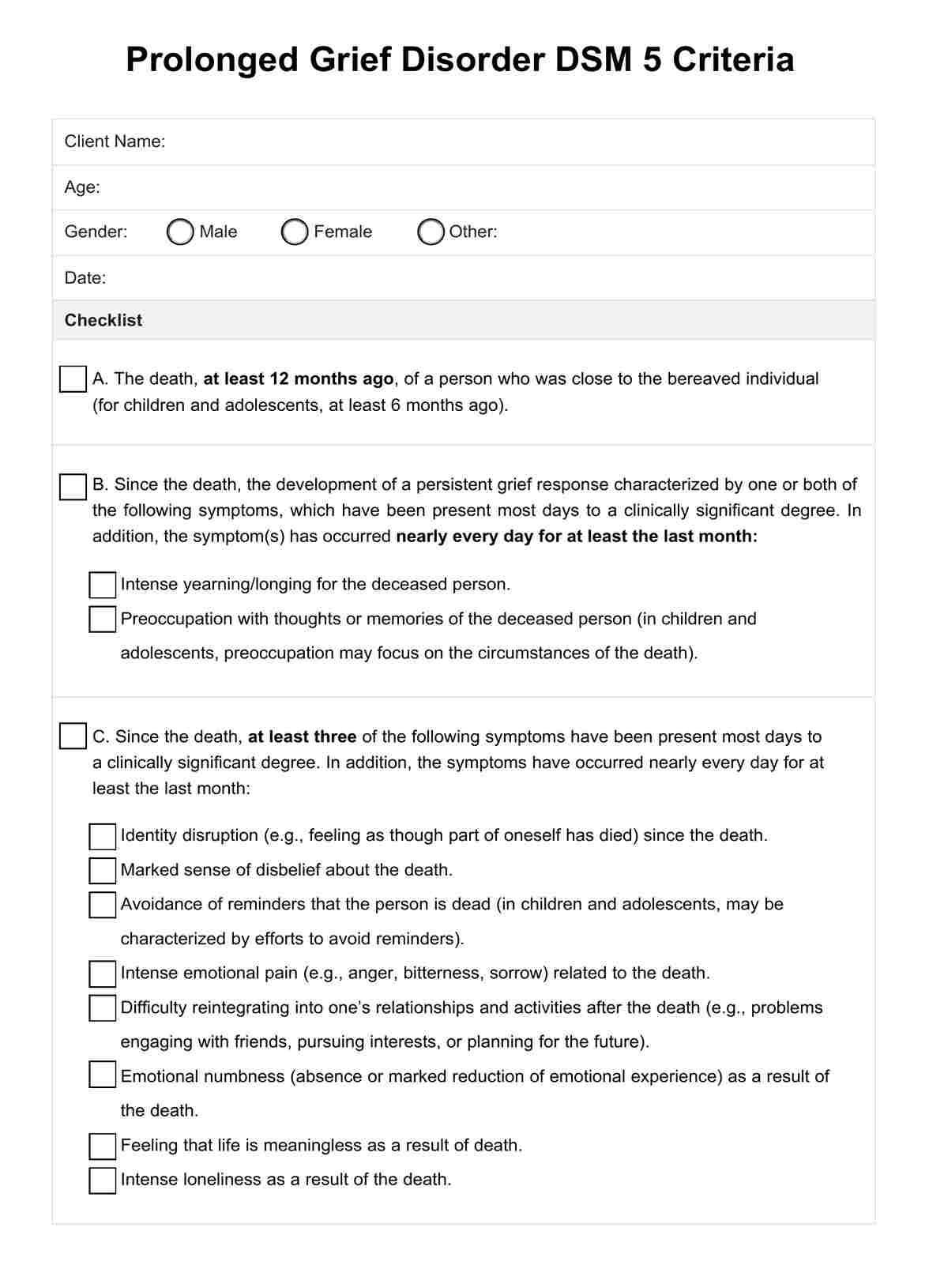
DSM 5 Criteria for Anorexia Nervosa
The Diagnostic and Statistical Manual of Mental Disorders (DSM 5) is a significant publication by the American Psychiatric Association, serving as a fundamental tool for diagnosing a wide range of mental health conditions, including anorexia nervosa. It provides standardized criteria to aid trained clinicians in accurately identifying mental disorders within a comprehensive case formulation assessment.
The criteria for diagnosing anorexia in the DSM 5 include:
- Restriction of food intake leading to significantly low body weight in relation to age, sex, developmental trajectory, and physical health.
- Intense fear of gaining weight or becoming fat, even though underweight.
- Disturbance in the way one experiences one's body weight or shape, undue influence of body weight or shape on self-evaluation, or denial of the seriousness of low body weight.
To be diagnosed with anorexia nervosa, a person must meet all three criteria. In addition, several specifiers can be used to characterize the disorder further, such as severity, remission status, and body mass index (BMI).
Download our comprehensive template for the full criteria.
Co-occurring disorders
Anorexia nervosa often co-occurs with other mental health disorders, such as anxiety, depression, or obsessive-compulsive disorder. These disorders may share similar underlying factors, such as genetics or neurotransmitter imbalances, and can exacerbate the symptoms of anorexia nervosa.
Here are some common co-occurring disorders with anorexia nervosa:
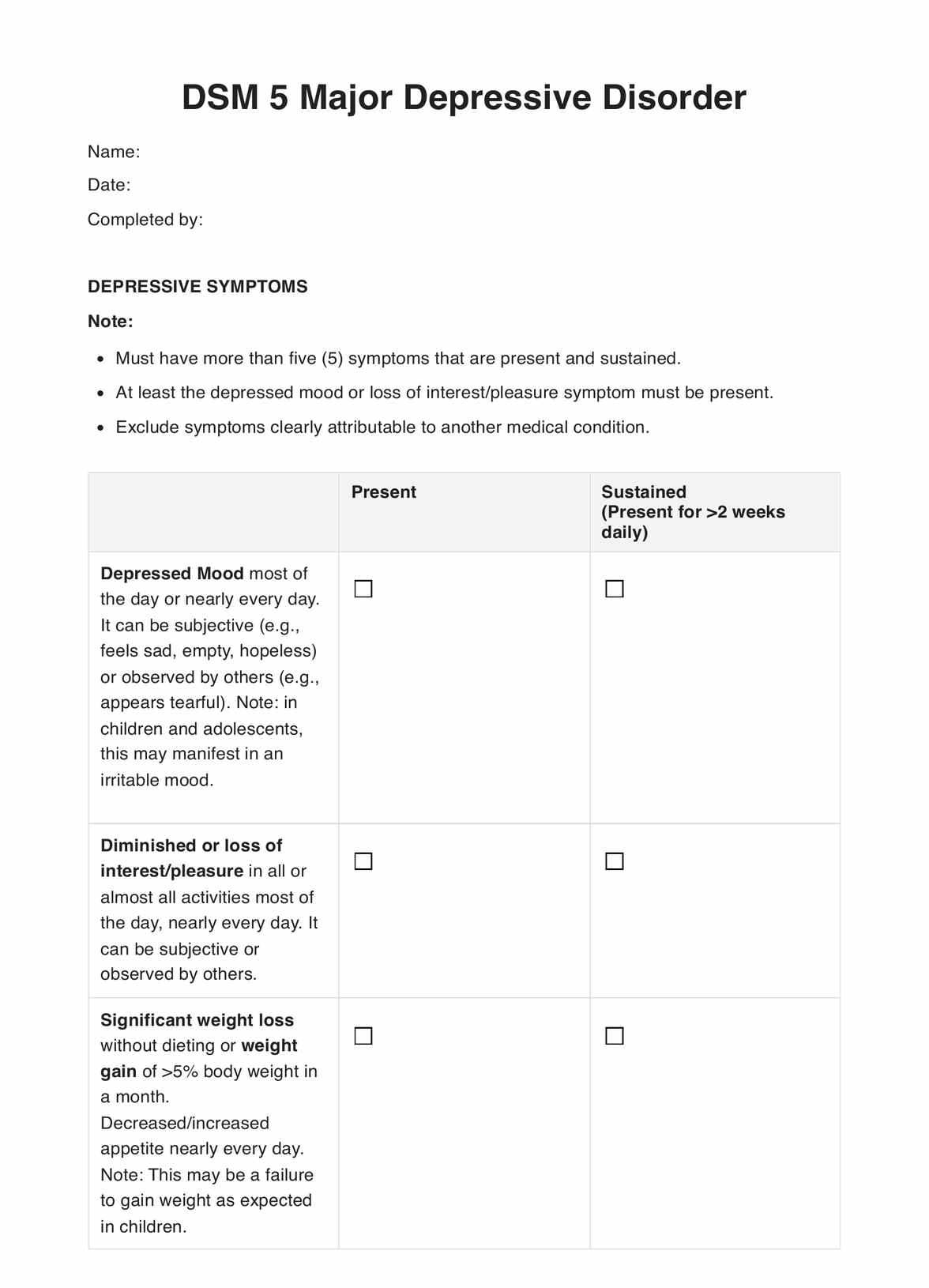
Depression
Individuals with anorexia nervosa may experience low mood, lack of energy, and feelings of hopelessness, which can further perpetuate disordered eating behaviors. Moreover, individuals with depression may also have body image issues and engage in excessive exercise or restrictive eating as a way to cope with negative emotions.
Anxiety
Anxiety can manifest as intense worry, fear, or panic, and these symptoms can contribute to the development and maintenance of anorexia nervosa. Individuals with anxiety may use disordered eating behaviors as a way to gain control over their thoughts and emotions.
Obsessive-compulsive disorder (OCD)
OCD and anorexia nervosa share similarities in terms of obsessive thoughts and compulsive behaviors. For example, an individual with anorexia may have obsessive thoughts about food or weight and engage in compulsive behaviors such as excessive exercising or restriction of food intake.
Substance abuse
Eating disorders and substance abuse often co-occur, with individuals turning to drugs or alcohol as a way to cope with the emotional distress and negative thoughts associated with anorexia nervosa.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders. Diagnostic and Statistical Manual of Mental Disorders, 5(5). https://doi.org/10.1176/appi.books.9780890425596
Moore, C. A., & Bokor, B. R. (2022). Anorexia nervosa. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK459148/
Substance Abuse and Mental Health Services Administration. (2016). Table 19, DSM-IV to DSM-5 anorexia nervosa comparison. Nih.gov; Substance Abuse and Mental Health Services Administration (US). https://www.ncbi.nlm.nih.gov/books/NBK519712/table/ch3.t15/
Commonly asked questions
Atypical anorexia nervosa shares many behaviors and psychological symptoms with classic anorexia nervosa, such as an intense fear of gaining weight and body image distortion. However, individuals with atypical anorexia nervosa do not meet the low weight criteria but still experience significant health complications and distress related to their eating disorder.
Self-induced vomiting is often associated with bulimia nervosa, a severe eating disorder characterized by binge eating followed by behaviors to avoid weight gain, such as self-induced vomiting. This behavior can also occur in individuals with anorexia nervosa as a method to control weight despite its severe health consequences.
While anorexia nervosa and binge eating disorder are typically viewed as distinct conditions, it's possible for an individual to exhibit behaviors of both disorders, although this is less common. This complex presentation requires careful assessment and a tailored treatment approach to address the spectrum of eating behaviors.
Bulimia nervosa is characterized by a cycle of binge eating and compensatory behaviors, such as self-induced vomiting, but it is not limited to these actions. Other behaviors can include misuse of laxatives, fasting, or excessive exercise. Like other eating disorders, bulimia nervosa involves complex psychological and emotional issues that require comprehensive treatment.




















-template.jpg)