Delusional Disorder DSM-5
Guide your diagnostic process with our Delusional Disorder DSM-5 checklist tool and create more aligned treatment plans. Download your free PDF here.


What is delusional disorder?
Delusional disorder is a psychiatric condition characterized by the presence of one or more delusions that persist for at least one month. Unlike other psychotic disorders, delusional disorder does not involve frequent hallucinations, and its symptoms are generally non-bizarre. The delusions involve situations that could occur in real life, such as being followed, poisoned, deceived by a spouse, or having a disease.
Typically, this mental disorder presents itself in the middle to late life, and its exact cause is usually attributed to different factors, such as genetic, biological, and environmental factors. Individuals with delusional disorders often function relatively well in daily life apart from the impact of their delusions.
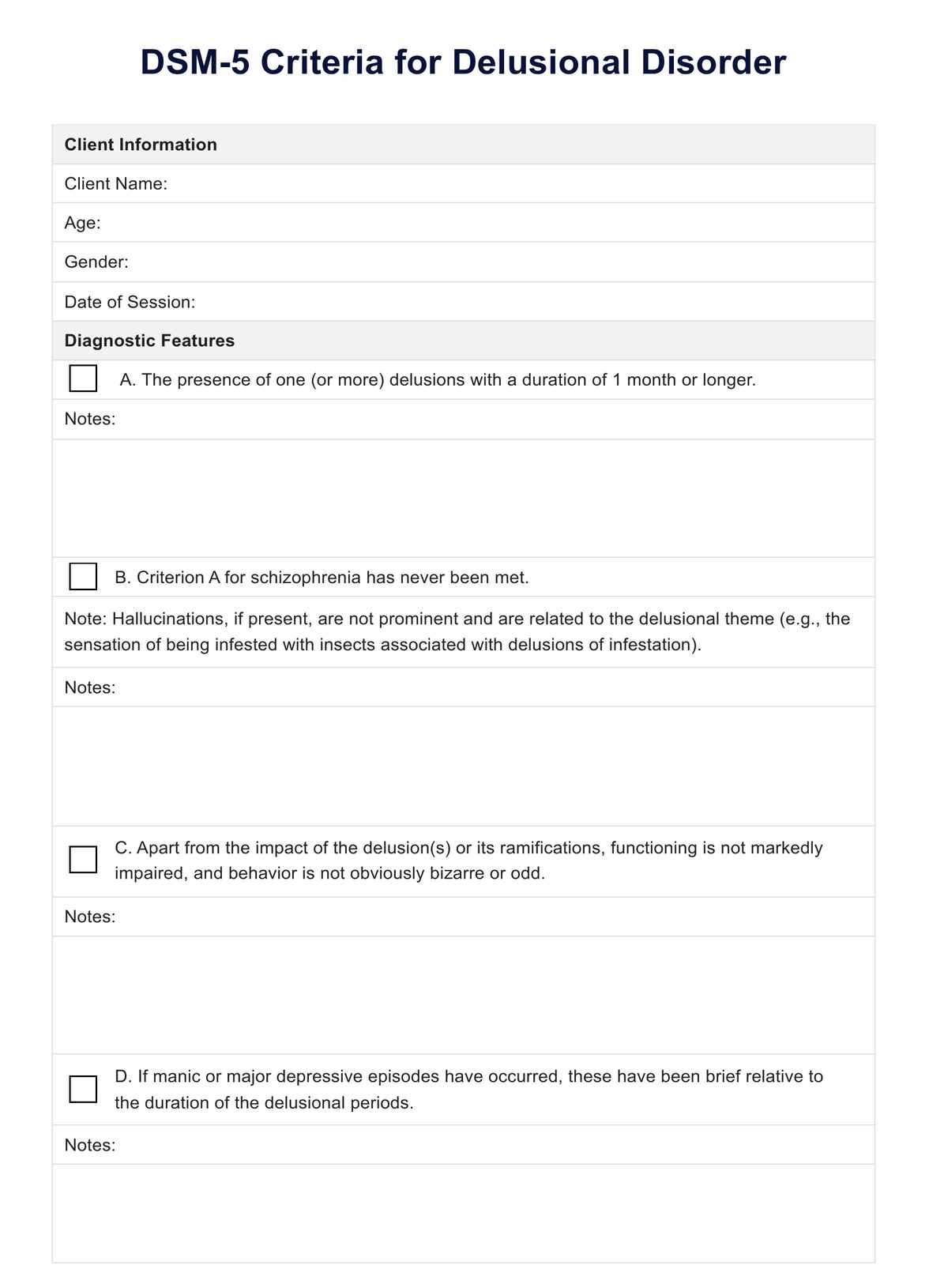
Delusional Disorder DSM-5 Template
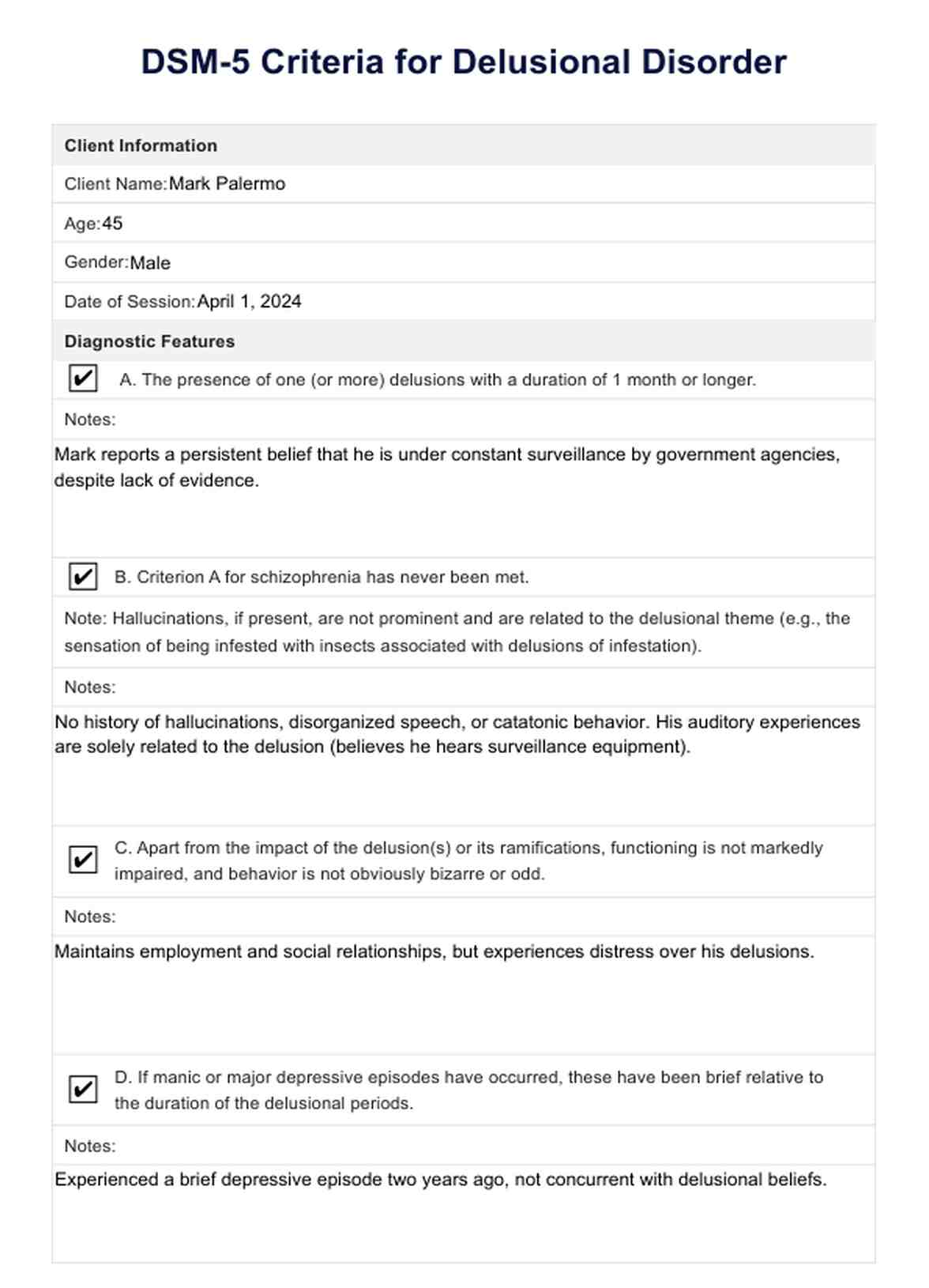
Delusional Disorder DSM-5 Example
Types of delusional disorders
Delusional disorder, recognized within the DSM-5 framework, manifests in various forms, each distinguished by the predominant theme of the individual's delusions. Understanding these types is crucial for effective diagnosis and management. Here's a closer look at each subtype:
- Erotomanic type: Individuals with erotomanic type delusions firmly believe that another person, often of higher status or completely unattainable, is in love with them. This conviction remains unchanged despite clear evidence to the contrary. These delusions can lead to significant distress or behavioral changes, including attempts to contact or stalk the object of their affection.
- Grandiose type: This subtype involves delusions of exceptional ability, wealth, or fame. Individuals may believe they have made a groundbreaking discovery or possess a unique talent despite no evidence supporting such beliefs. The grandiose type can lead to behaviors that reflect an inflated sense of self-importance or entitlement.
- Jealous type: Characterized by the unwavering belief that the individual's spouse or partner is unfaithful, jealous-type delusions are often accompanied by constant scrutiny and accusations, which can strain or destroy relationships. Despite a lack of evidence, the conviction of their partner's infidelity remains unshakable.
- Persecutory type: Individuals with this subtype believe they are being persecuted, mistreated, or conspired against. Common delusions include being followed, poisoned, or deceived by loved ones or colleagues. These delusions can provoke significant distress, legal problems, or even retaliatory actions based on perceived threats.
- Somatic type: Somatic delusions involve a preoccupation with health and bodily functions. Individuals may be convinced they have a severe disease or a physical deformity, leading to excessive health-related behaviors or medical consultations despite assurances from health professionals that no such issue exists.
- Mixed type: In some cases, individuals do not fit neatly into a single category but instead display a mix of delusional themes without one predominating. This complexity can pose additional challenges for diagnosis and treatment.
How to diagnose delusional disorders?
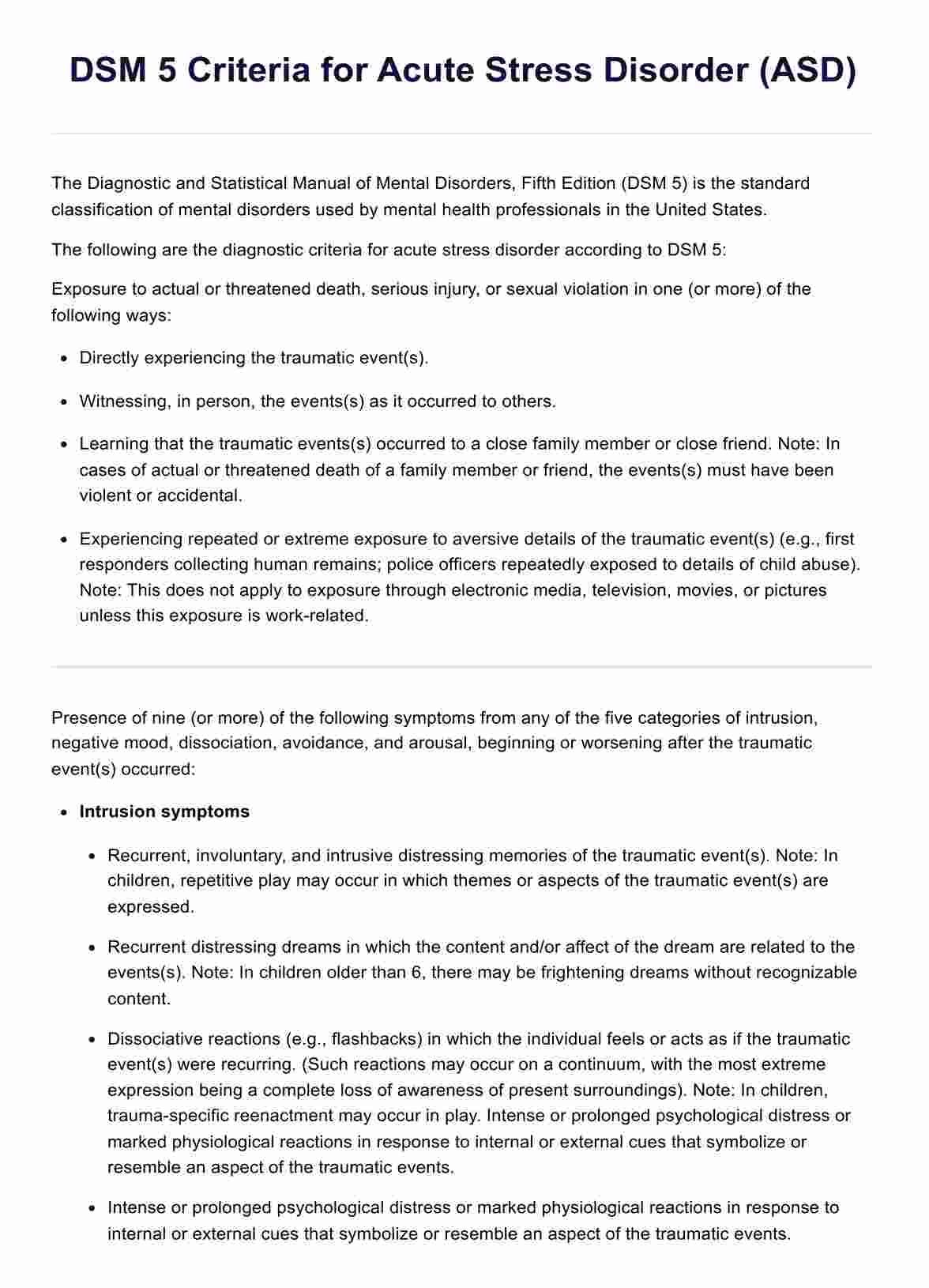
Diagnosing Delusional Disorder involves a thorough clinical assessment guided by criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-5). This manual, published by the American Psychiatric Association (2013), provides criteria for the classification and diagnosis of mental disorders. Clinicians and researchers widely use it to help diagnose and treat mental health conditions. Successful diagnosis also rests on distinguishing it from other mental health conditions that also feature delusions. The following measures are commonly taken to diagnose delusional disorder.
Clinical interview and assessment
A comprehensive clinical interview is valuable, supported with collateral information from family, friends, or previous medical records when possible. Self-report tests and questionnaires such as the Brown Assessment of Beliefs Scale can also be helpful in indicating areas in an individual's functioning that might need further exploration. This holistic approach offers insight into the historical and current presentation of symptoms, which can help establish the presence and nature of delusions.
Rule out other psychotic disorders
Since delusions also occur in conditions like schizophrenia, schizoaffective disorder, and bipolar disorder, it's important to determine that another psychotic disorder cannot better explain these symptoms. In delusional disorder, the core symptoms of schizophrenia (such as disorganized speech or behavior, catatonia, or negative symptoms) are not prominent.
Consider the role of substances and medical conditions
Another critical diagnostic step involves ruling out the effects of substances (e.g., drugs, medication) or another medical condition that could account for the delusions. This is to rule out a possible substance-induced psychotic disorder or disorder due to a medical condition. This involves a comprehensive medical history, possible lab tests, and sometimes a physical examination to uncover any underlying medical issues that could present with psychosis-like symptoms.
Evaluate the impact on functioning
Although individuals with delusional disorders might function relatively well in daily life, their delusions can cause distress and markedly impaired social and occupational functioning. Evaluating the extent of this impact is essential. However, it's notable that apart from the direct consequences of the delusions, their overall functioning might remain intact, differentiating them from disorders with more pervasive symptoms.
Refer to DSM-5 criteria for specific subtypes
Once a diagnosis of Delusional Disorder is considered, the DSM-5 provides criteria for specific subtypes (e.g., erotomanic, grandiose, jealous, persecutory, somatic, mixed). Identifying the subtype involves understanding the main theme of the delusions, which can guide treatment planning.
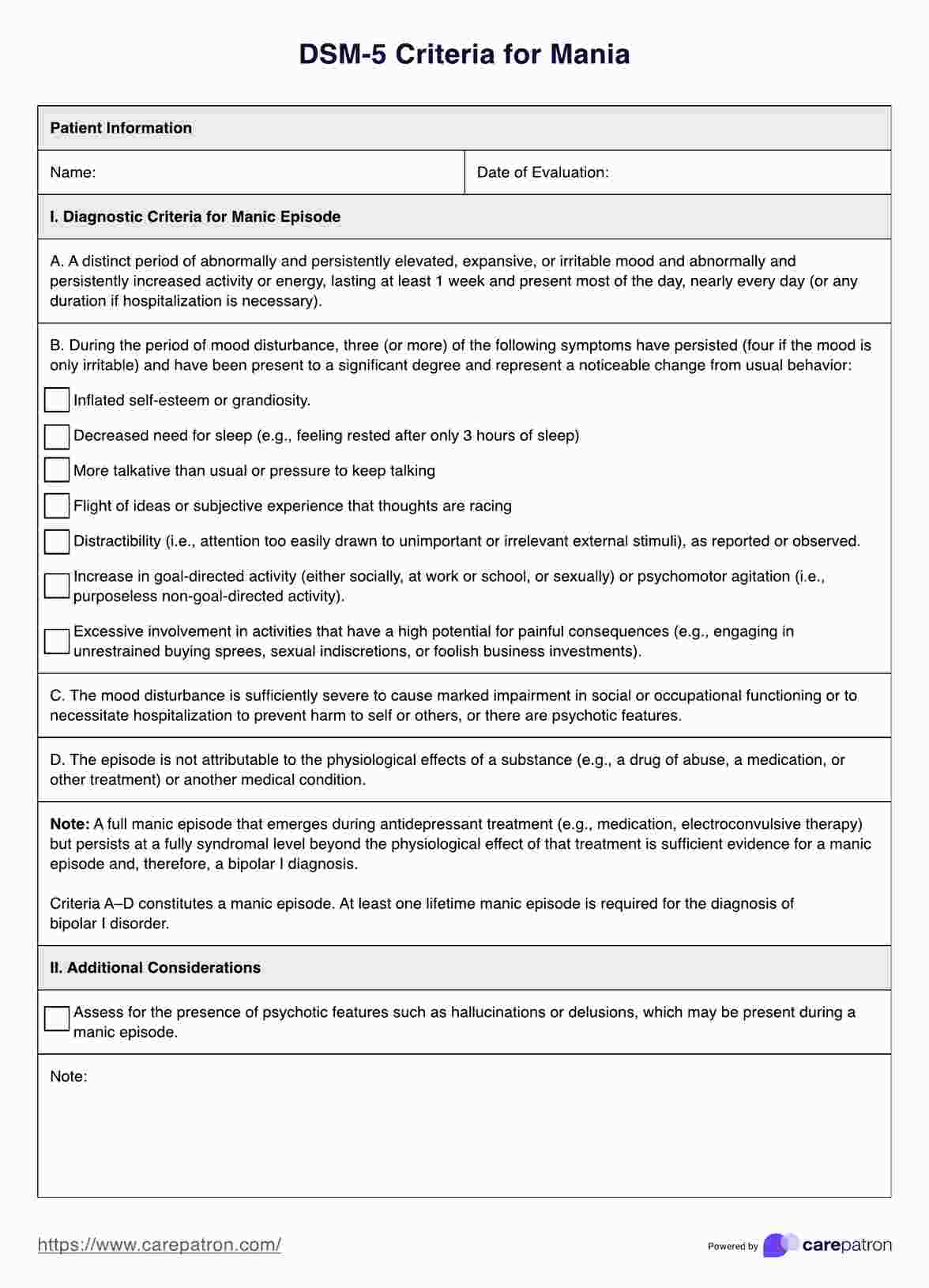
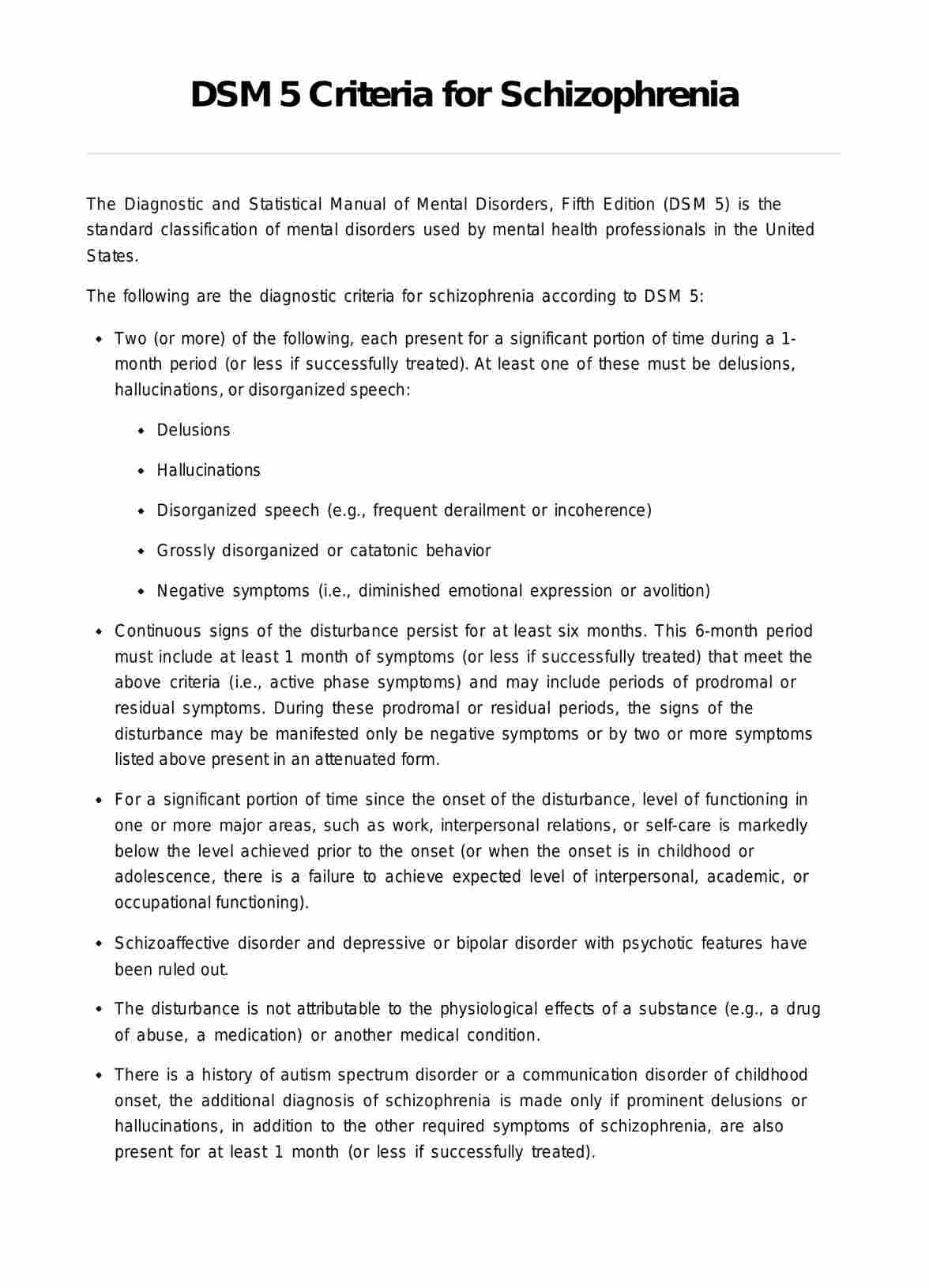
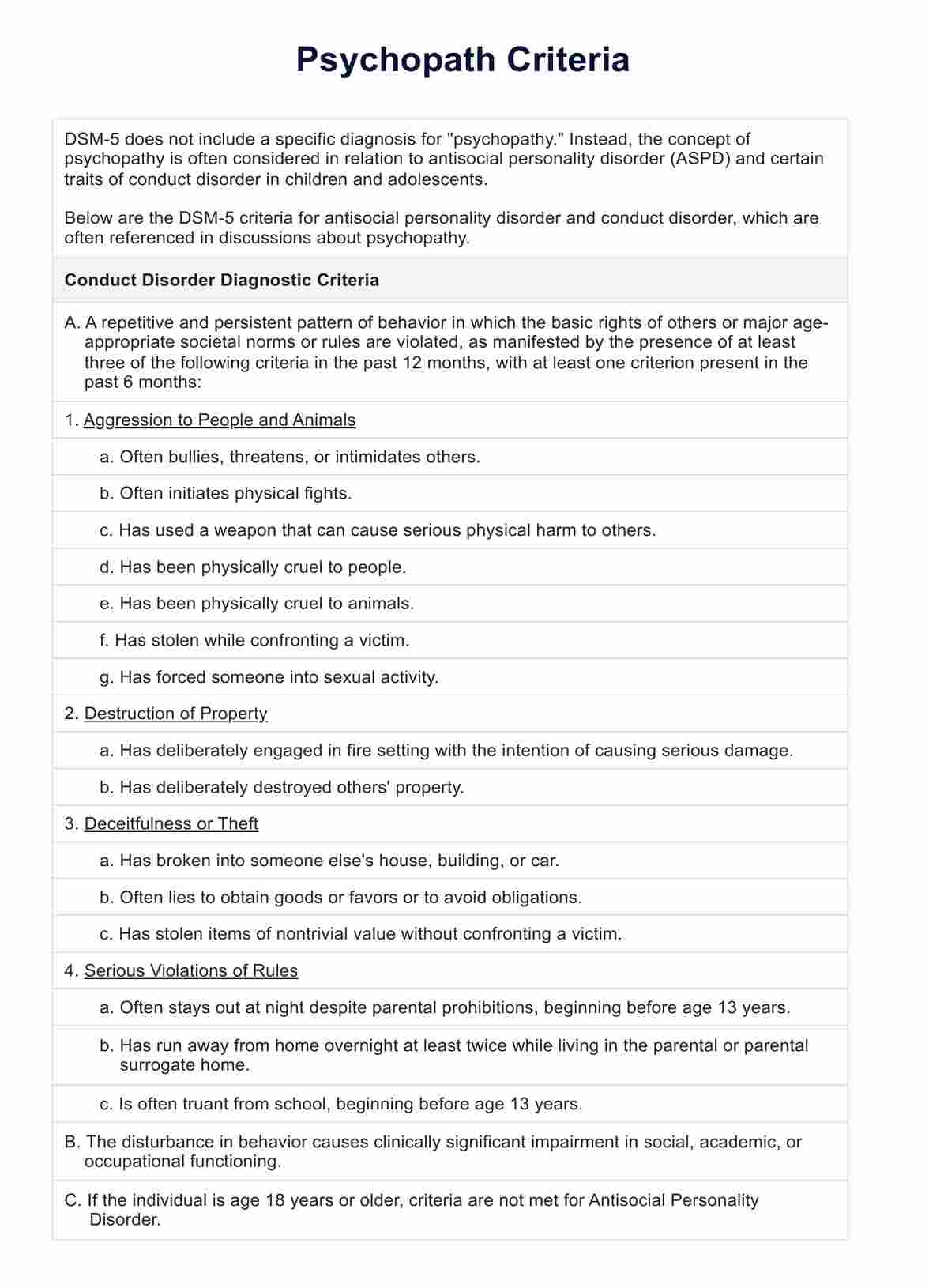
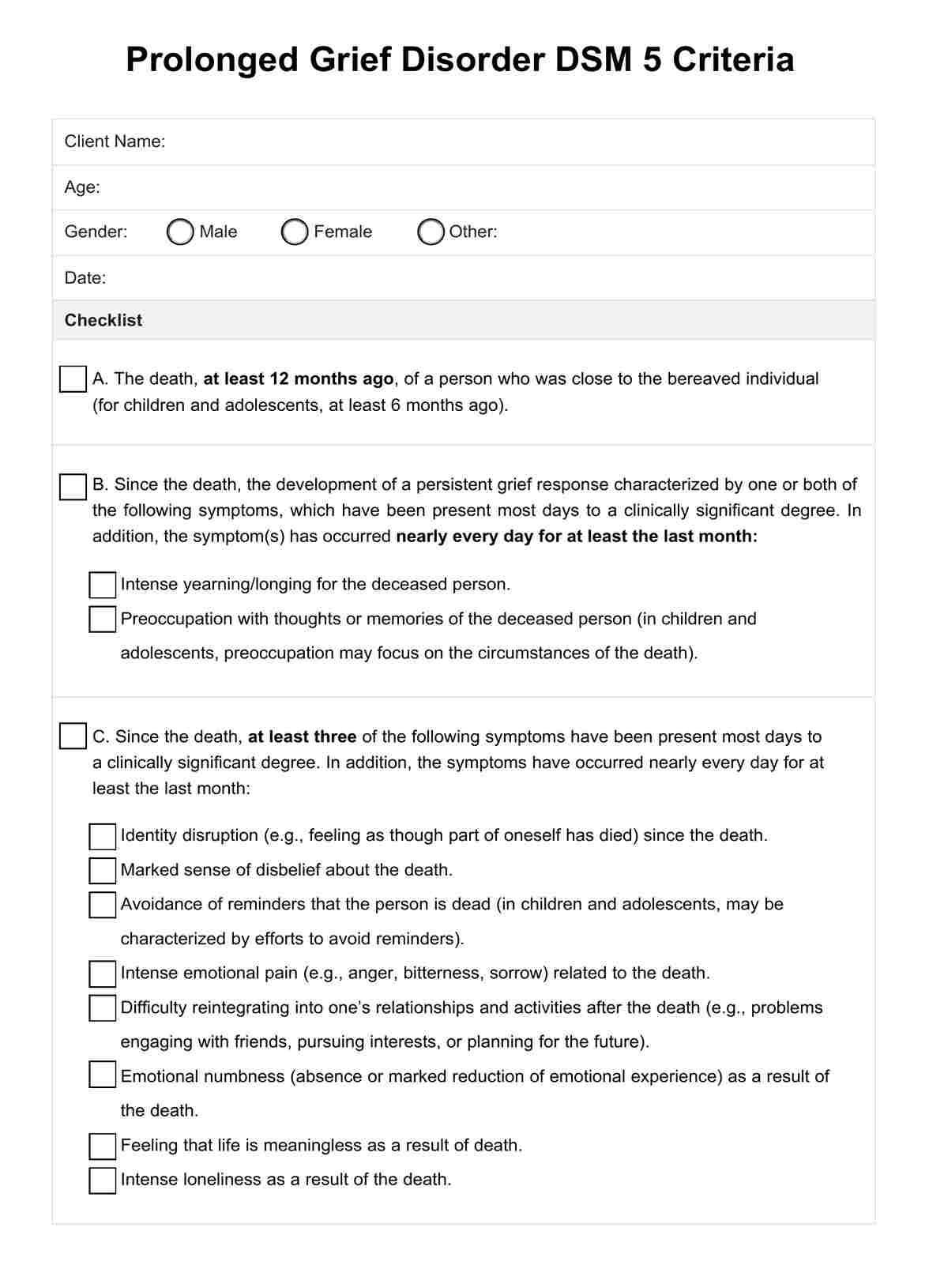
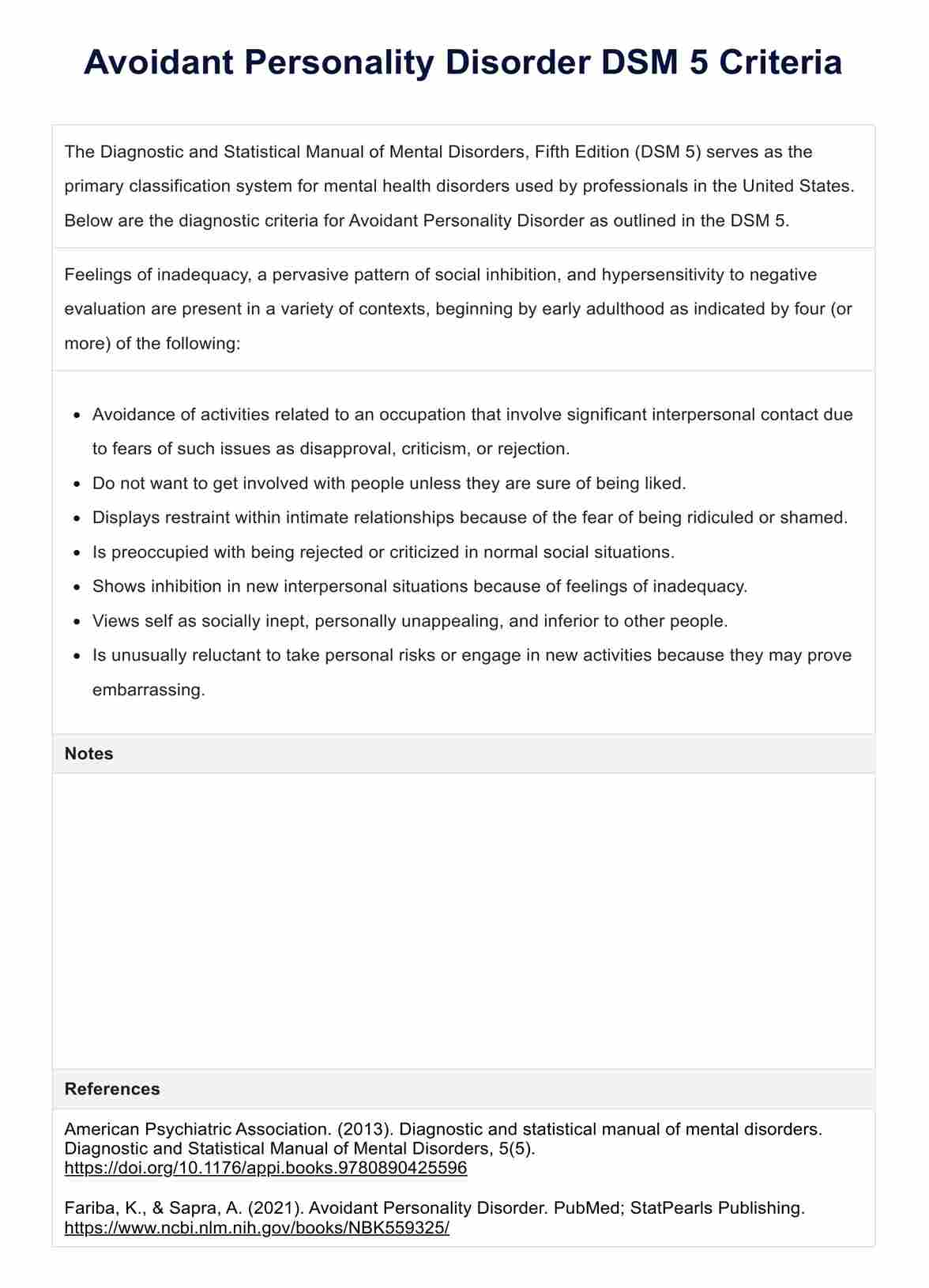
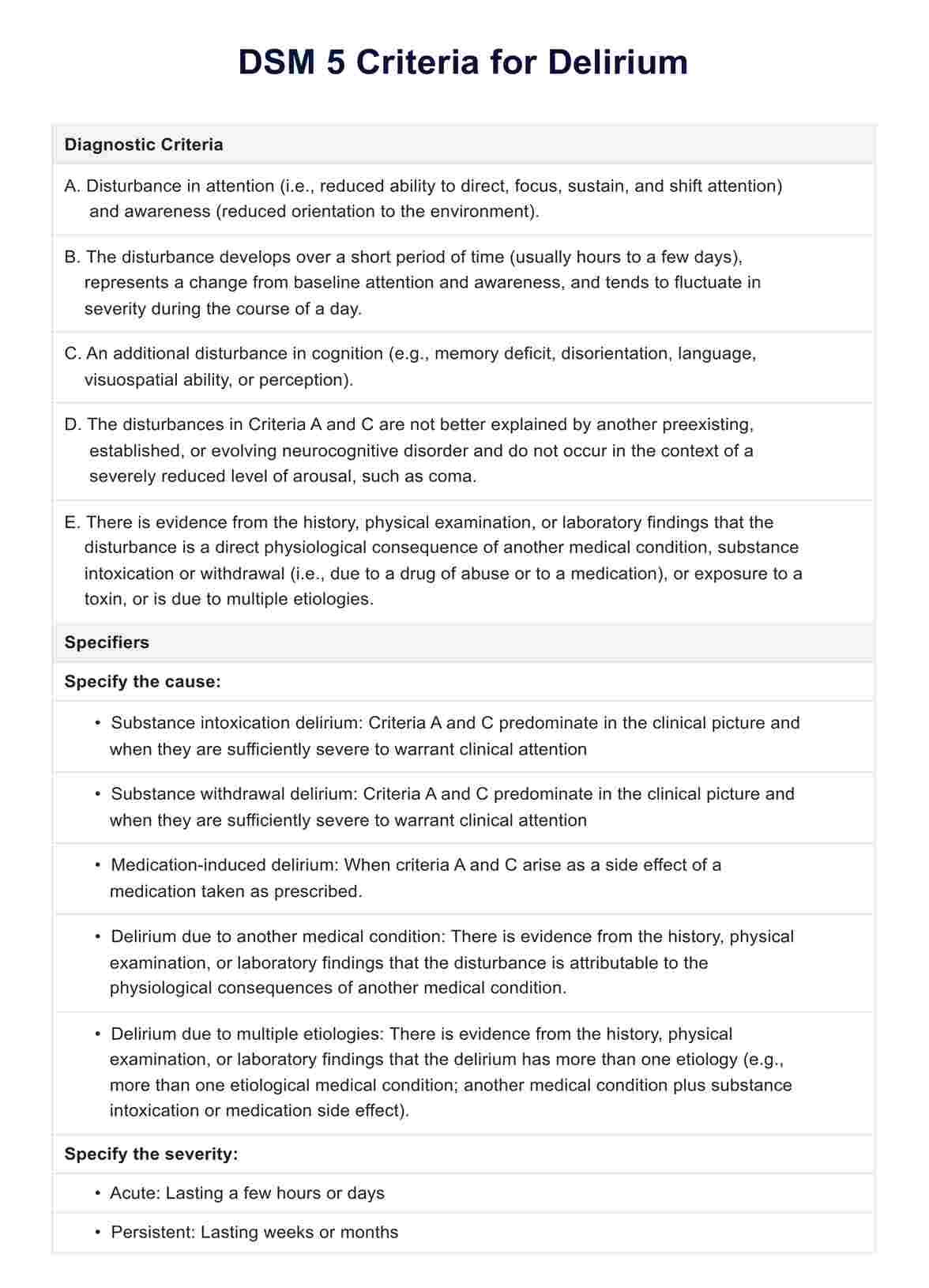
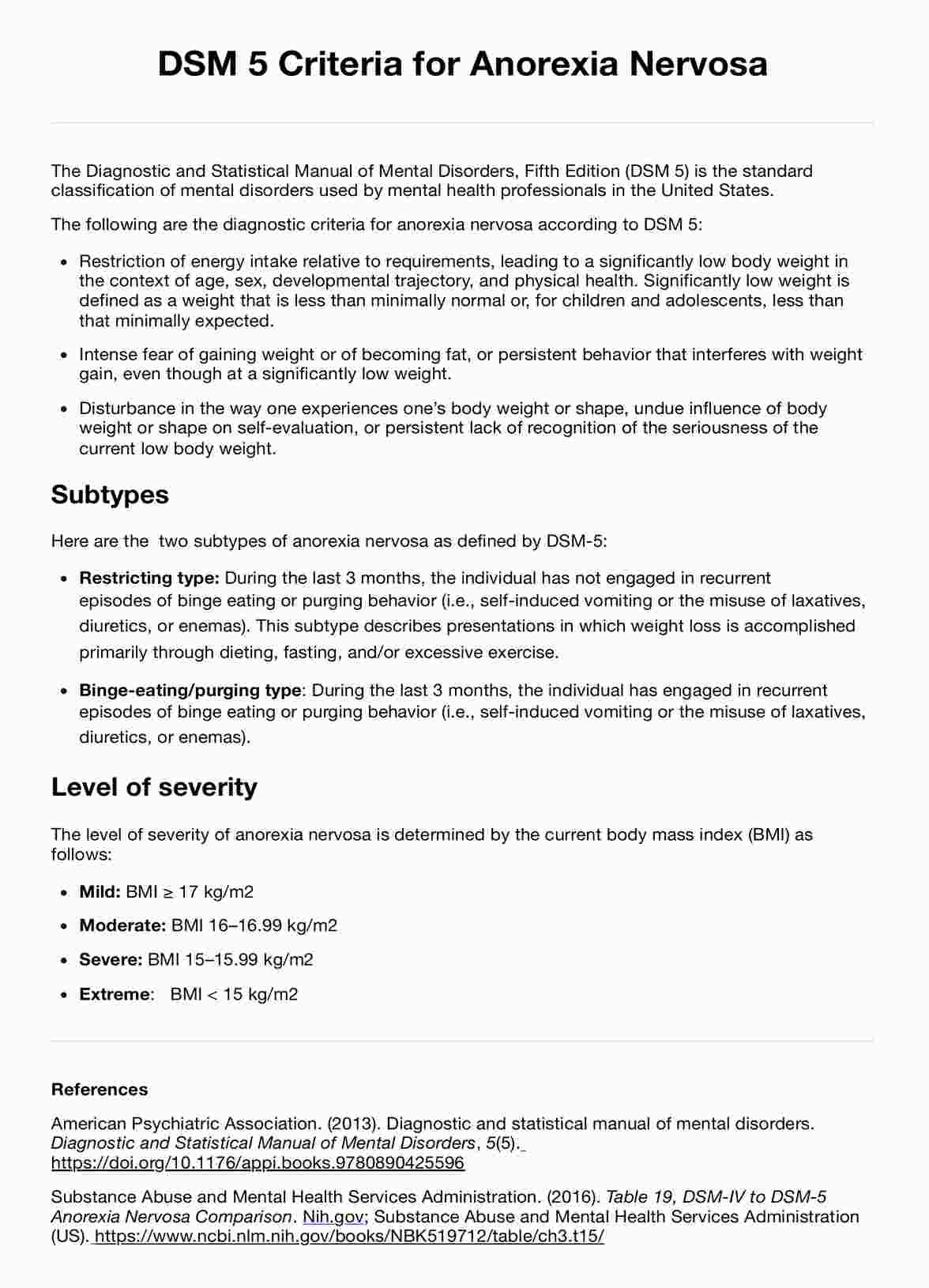
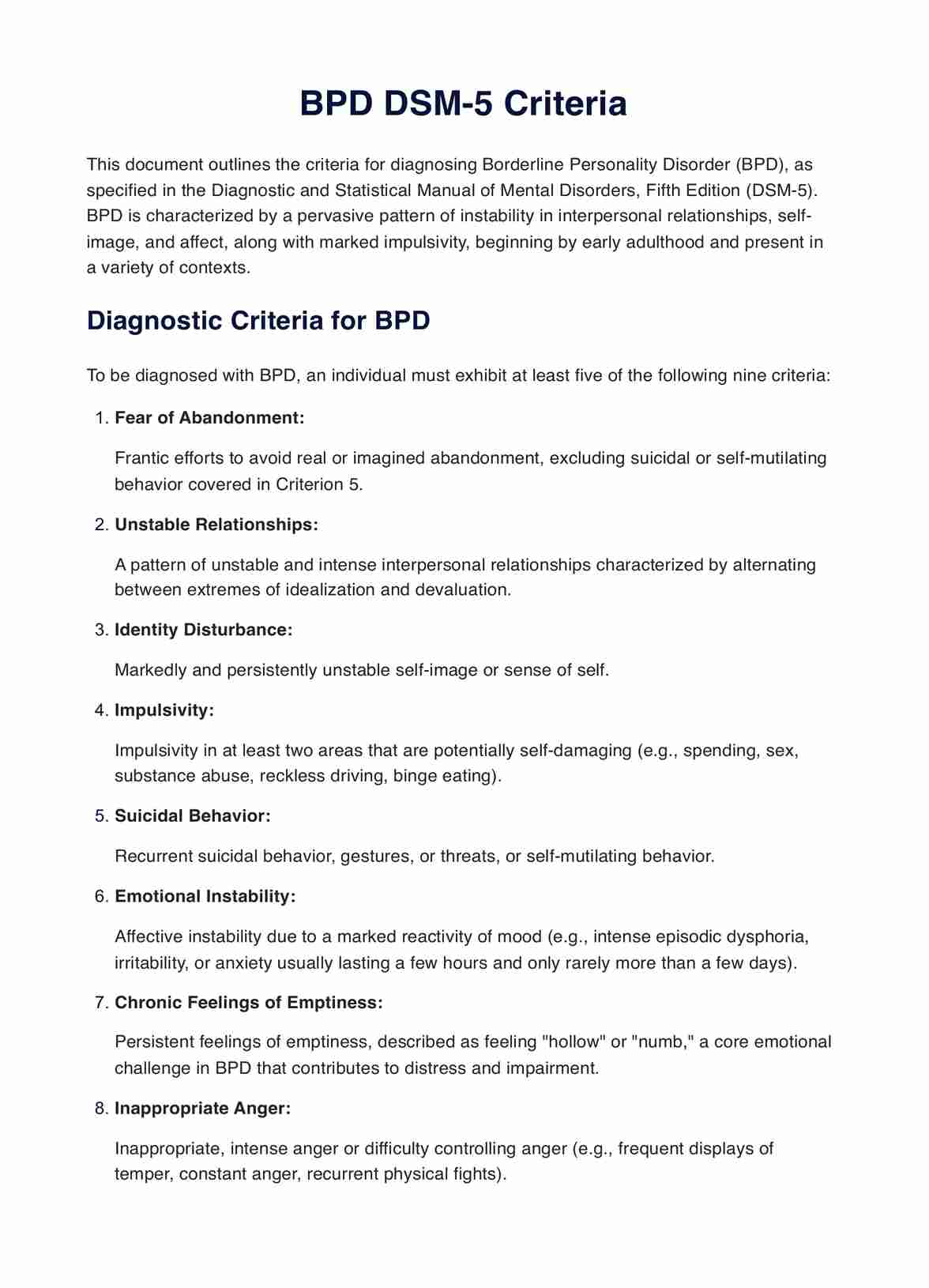
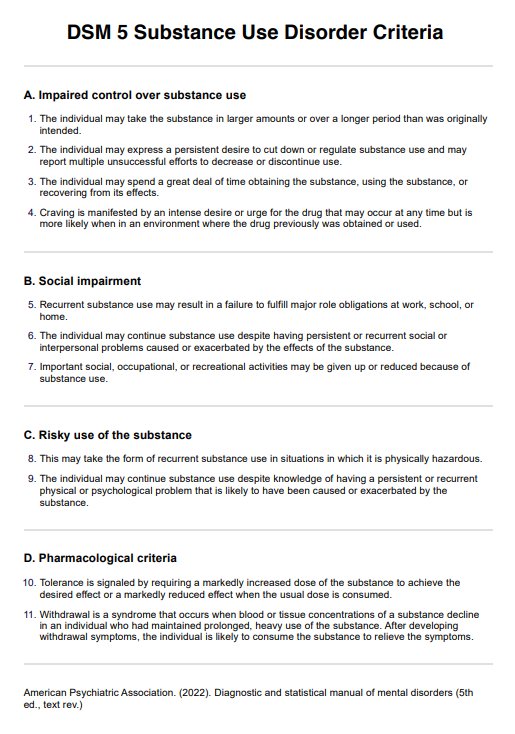
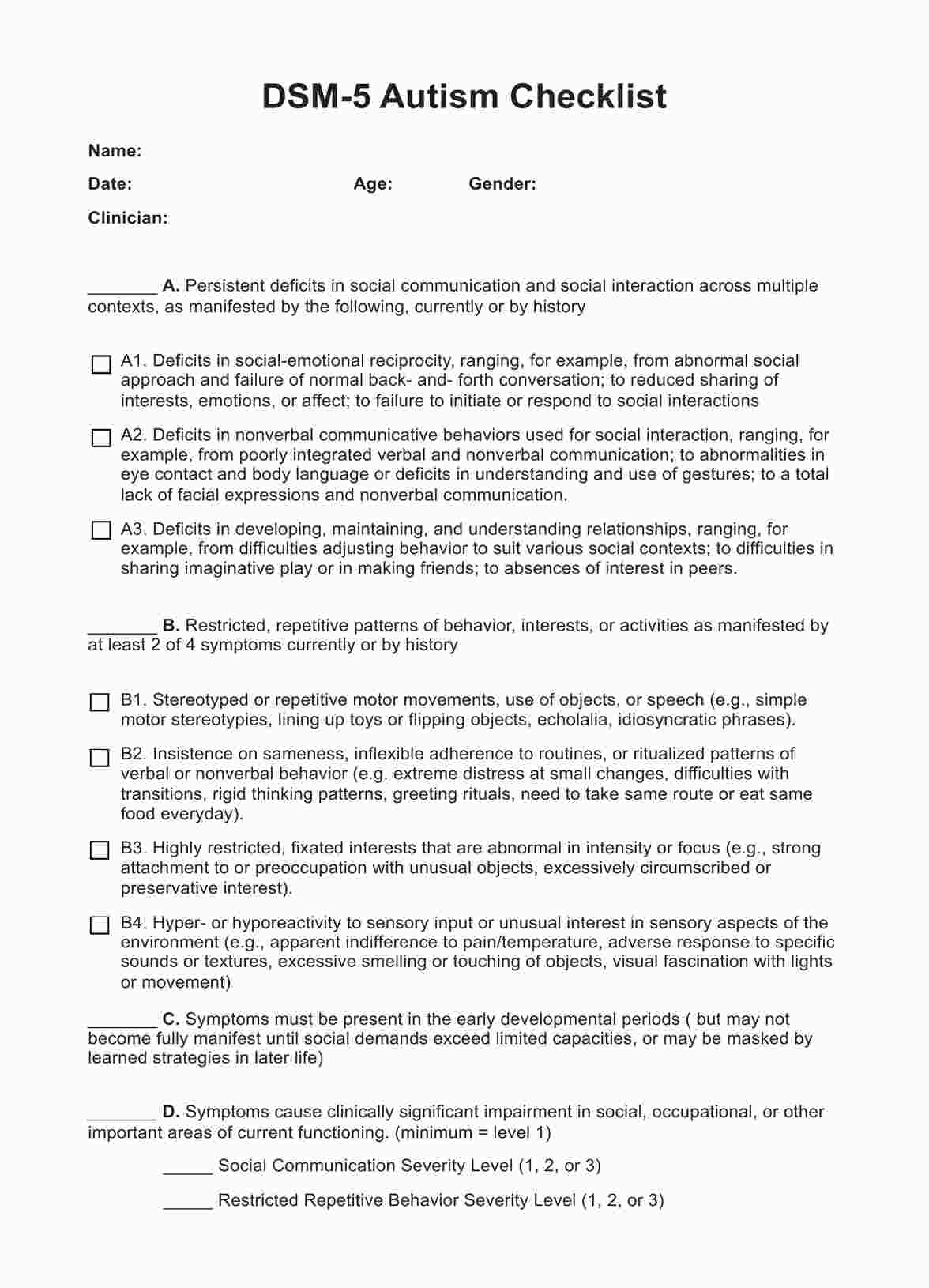
Diagnostic criteria for delusional disorder
The foundation of diagnosing Delusional Disorder is to follow the DSM-5 criteria, which provide a structured framework to assess the present symptoms in patients.
Clinicians should look for the following components when diagnosing the disorder:
Criterion A: Presence of delusions
The primary feature is the presence of one or more delusions with a duration of one month or longer. Delusions are firm beliefs in something that cannot be true or isn't based on reality.
Criterion B: Exclusion of other psychotic disorders
Delusions must not occur exclusively during the course of schizophrenia, bipolar disorder, depressive disorder with psychotic features, and other psychotic disorders.
Criterion C: Functionality
Apart from the direct impact of the delusions, functioning is not markedly impaired. Behavior is neither odd nor bizarre. It is not unusual to find individuals maintaining normal life activities and social relations despite harboring persistent delusional beliefs.
Criterion D: Exclusion of substance influence or medical condition
If substance use, withdrawal, or exposure to a toxin explains the delusions, then Delusional Disorder is not a suitable diagnosis. The same holds true for any general medical condition that might cause psychotic symptoms.
Criterion E: Coexistence with mood disorders
If mood episodes have occurred concurrently with delusions, their total duration has been brief relative to the duration of the delusional periods.
Beyond the core criteria, specifying the subtype of Delusional Disorder is encouraged based on the predominant delusional theme and if there are bizarre delusions. After a 1-year duration of the disorder, it is also important to specify the current status of the condition through the following:
- First episode, currently in acute episode: Initial presentation of the disorder with symptoms fully meeting diagnostic criteria.
- First episode, currently in partial remission: Initial episode showing significant improvement, with symptoms partially meeting diagnostic criteria.
- First episode, currently in full remission: Period following the first episode with no disorder-specific symptoms.
- Multiple episodes, currently in acute episode: Recurrent episodes with symptoms fully meeting diagnostic criteria.
- Multiple episodes, currently in partial remission: Recurrent episodes showing significant improvement, with symptoms partially meeting the criteria.
- Multiple episodes, currently in full remission: Period following multiple episodes with no disorder-specific symptoms.
- Continuous: Symptoms persist throughout the majority of the illness course, with only brief periods of subthreshold symptoms.
- Unspecified: Not enough information to specify the disorder's course.
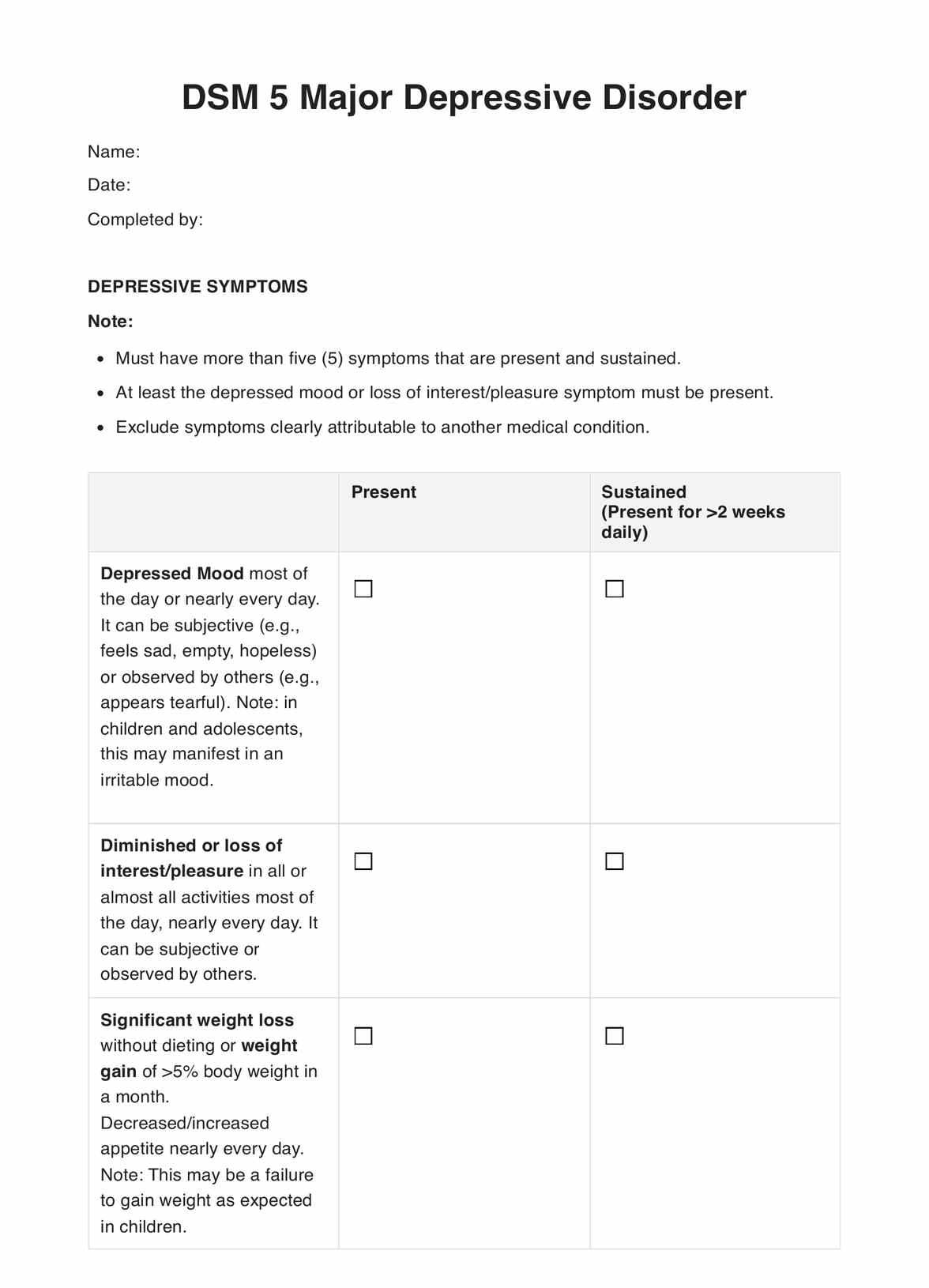
How to use our Delusional Disorder DSM-5 criteria template?
Incorporating the DSM-5 criteria guides clinicians in making more accurate diagnoses, which is the first step toward facilitating effective treatment strategies. Here is a step-by-step process for using our Delusional Disorder DSM-5 criteria template when working with clients:
Step 1: Familiarize with the criteria
Before engaging with clients, ensure a thorough understanding of the DSM-5 criteria for Delusional Disorder. This foundational knowledge is crucial for recognizing the nuanced symptoms that differentiate this disorder from other psychiatric conditions.
Step 2: Use the checklist to note symptoms of delusional disorder
While interacting with the client, actively use the checklist to identify and record any symptoms that align with the DSM-5 criteria. This step is essential for gathering concrete evidence of delusions and other relevant symptoms. This can also help rule out other psychotic symptoms and mental disorders in making a diagnosis.
Step 3: Document additional notes
Beyond the checklist, make detailed notes regarding the client's condition, including any observations that may not neatly fit into the checklist categories. Including context and subjective insights can provide a fuller picture of the client's mental health state.
Step 4: Evaluate insights from the checklist
Review the completed checklist and supplementary notes to analyze the gathered information. In this retrospective evaluation, you synthesize observed symptoms with clinical knowledge to form a preliminary assessment.
Step 5: Incorporate data into treatment planning
Use the collected data and your diagnostic assessment to plan a tailored treatment. Integrating the insights from the checklist ensures that treatment strategies directly address the individual's specific manifestations of delusional disorder.
How to treat and manage delusional disorder?
The treatment of Delusional Disorder requires an interdisciplinary approach that combines pharmacotherapy with psychotherapy, often tailored to the individual’s specific needs and the nature of their dominant delusional belief. The following strategies are often taken in managing and treating delusional disorder:
Pharmacotherapy
Medication is often a primary intervention. Antipsychotics are essential in pharmacological treatment and are selected based on their efficacy, side-effect profile, and patient response. In some cases, other medications like antidepressants or mood stabilizers may complement antipsychotic treatment, particularly when there are co-morbid conditions.
Psychotherapy
Cognitive-behavioral therapy (CBT) is frequently employed to help patients recognize and challenge the validity of their delusions in a non-confrontational manner. CBT can be instrumental in alleviating the distress associated with delusions and improving day-to-day functioning.
Supportive therapy provides a stable and understanding environment in which patients can express their concerns and receive reassurance. This mode of therapy often focuses on stress management, improving self-esteem, and promoting adaptive coping mechanisms.
Family therapy can also be helpful, offering education about the disorder to family members, which helps in creating a supportive home environment that can reduce the frequency and intensity of delusional episodes. Involving family members can also prepare them to detect early signs of relapse and seek timely intervention.
Social interventions
Social skills training and vocational rehabilitation may also be necessary as these interventions help individuals re-engage with community activities and work environments, which their delusions can disrupt. Building a network of social support, including support groups specifically for delusional disorder, can address feelings of isolation.
Reference
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC.
Commonly asked questions
Delusional Disorder is differentiated by the presence of one or more delusions for one month or longer without the significant hallucinations typical of schizophrenia. In contrast, other psychotic disorders present with broader symptomatology, including hallucinations, disorganized speech, and behavior, which are not the central features of delusional disorder.
The exact cause of delusional disorder is not yet fully understood, but a combination of genetic, biological, environmental, and psychological factors is considered contributors. Biologically, it may involve imbalances in neurotransmitters in the brain. Genetic factors may include a family history of Delusional Disorder or related conditions. Environmental triggers could involve significant stress or trauma, while psychological aspects might involve personality traits or a tendency to mistrust others.
Psychosis is a broad term that describes a state in which an individual has lost touch with reality, and it can include a wide range of clinical symptoms like hallucinations, delusions, disorganized thinking, and behavior. delusional disorder is a specific type of psychosis where the primary feature is one or more delusions.





















-template.jpg)





















































































