Mood Disorder DSM 5 Criteria
Explore a comprehensive reference tool to help diagnose bipolar and depressive disorders.


What is a mood disorder?
Mood disorders are mental health conditions that affect your emotional state in a significant and persistent way. They can disrupt your daily life, relationships, and overall well-being.
The American Psychiatric Association (APA) categorizes mood disorders in its Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Here's a breakdown of the two main groups:
- Depressive disorders: Characterized by prolonged sadness, emptiness, and a loss of interest in activities you used to enjoy. Examples include major depressive disorder and dysthymia (persistent depressive disorder).
- Bipolar and related disorders: Involve cycles of extreme emotional states, including mania (intense euphoria) or hypomania (elevated mood) and depression. Bipolar I and bipolar II disorders fall under this category.
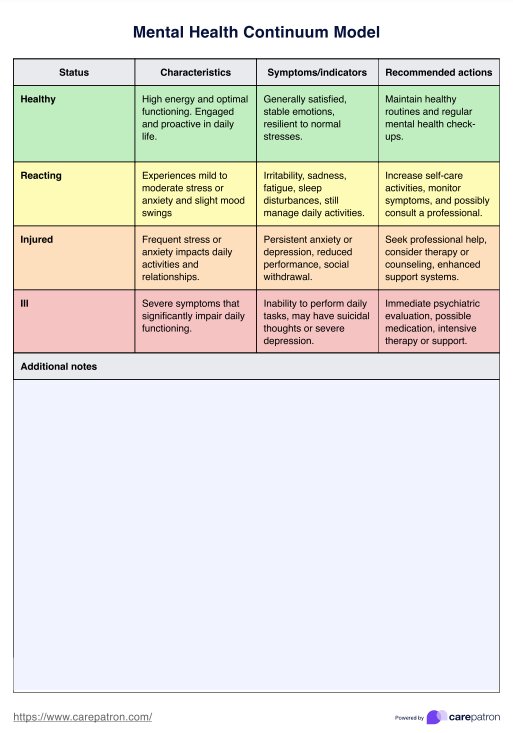
Early and accurate diagnosis of mood disorders is crucial for effective treatment and management. Healthcare professionals should be familiar with the signs and symptoms of these conditions to ensure appropriate interventions and improve patient outcomes.
Mood disorder symptoms and characteristics
Mood disorders are characterized by a range of symptoms that can significantly impact an individual's daily life and functioning. The specific symptoms and characteristics vary depending on the type of mood disorder. Here's an overview:
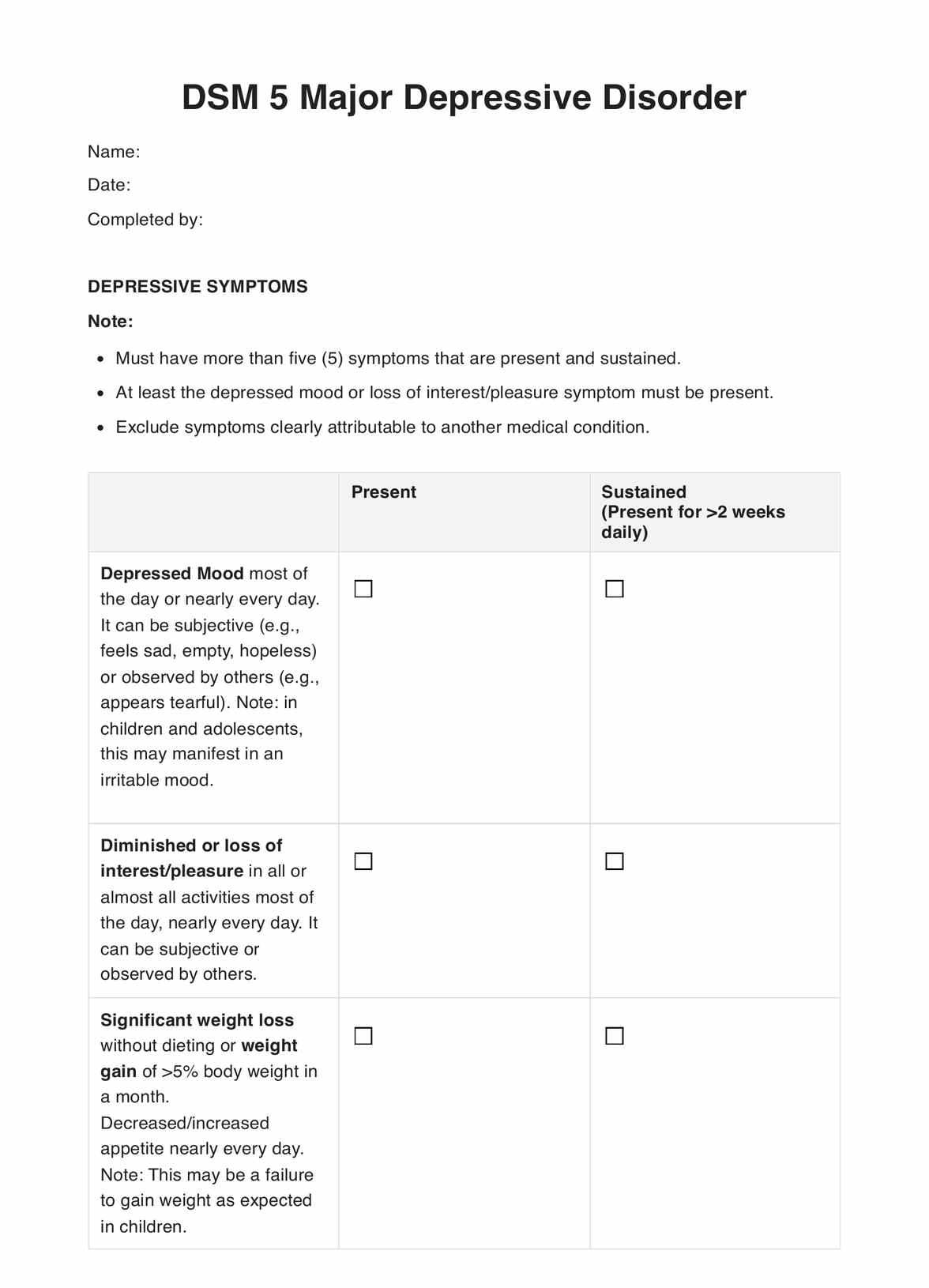
In depressive disorders, individuals experience a common profile with the following symptoms:
- Pervasive sadness, emptiness, or hopelessness
- Loss of interest or pleasure in activities
- Significant weight loss or gain, or decrease or increase in appetite
- Sleep disturbances (insomnia or hypersomnia)
- Fatigue or loss of energy
- Feelings of worthlessness or excessive guilt
- Difficulty concentrating or making decisions
- Recurrent thoughts of death, suicidal ideation, or suicide attempts
On the other hand, people with bipolar disorders involve the following:
- Abnormally elevated, expansive, or irritable mood
- Increased activity or energy levels lasting at least one week
- Inflated self-esteem or grandiosity
- Reduced need for sleep
- More talkative than usual or pressure to keep talking
- Flight of ideas or racing thoughts
- Distractibility
- Increased goal-directed activity (socially, at work, or school; sexually) or psychomotor agitation
- Excessive involvement in risky activities with the potential for painful consequences
Causes of mood disorders
Mood disorders can arise from a complex interplay of various factors, including biological, psychological, and environmental influences. Understanding the potential causes can help healthcare practitioners provide more effective treatment and support for individuals affected by these conditions.
- Genetics: Research suggests that mood disorders have a significant genetic component, with certain gene variations increasing the risk of developing conditions like major depressive disorder and bipolar disorder (Shadrina et al., 2018).
- Brain chemistry: Imbalances in neurotransmitters, such as serotonin, dopamine, and norepinephrine, have been linked to mood disorders. These chemical messengers play crucial roles in regulating mood, emotions, and cognitive functions.
- Hormonal factors: Hormonal fluctuations, particularly in estrogen and progesterone levels, can contribute to the development of certain mood disorders, such as premenstrual dysphoric disorder and postpartum depression.
- Cognitive patterns: Negative thought patterns, such as pessimistic thinking, low self-esteem, and distorted perceptions, can contribute to the onset and maintenance of mood disorders like depression (Beck, 2011).
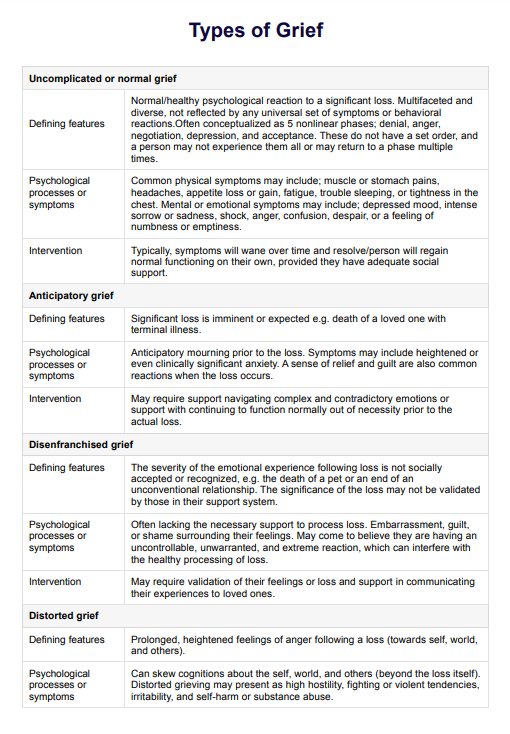
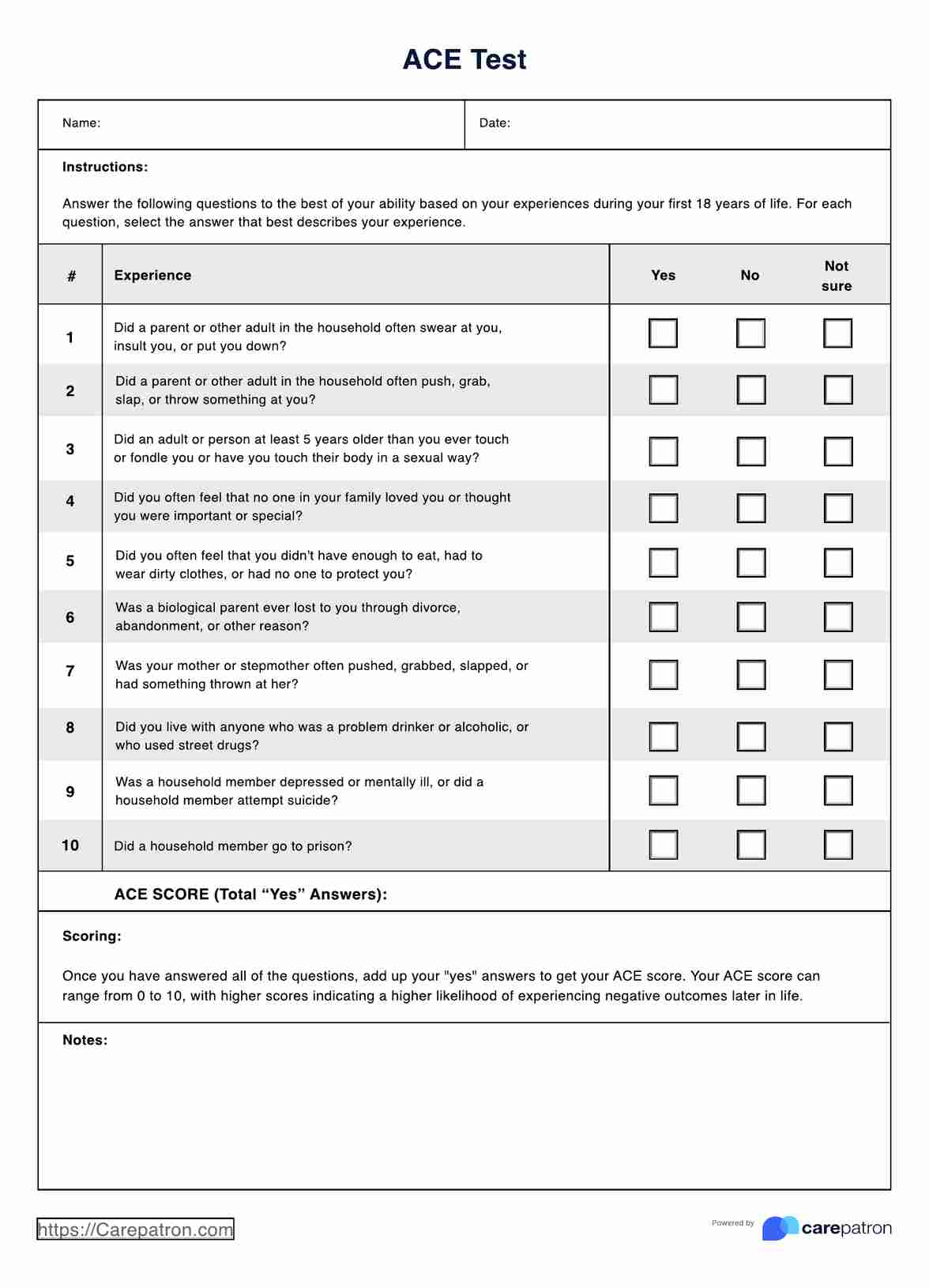
- Life events: Significant life stressors, such as trauma, loss, or major life transitions, can trigger or exacerbate mood disorders in susceptible individuals.
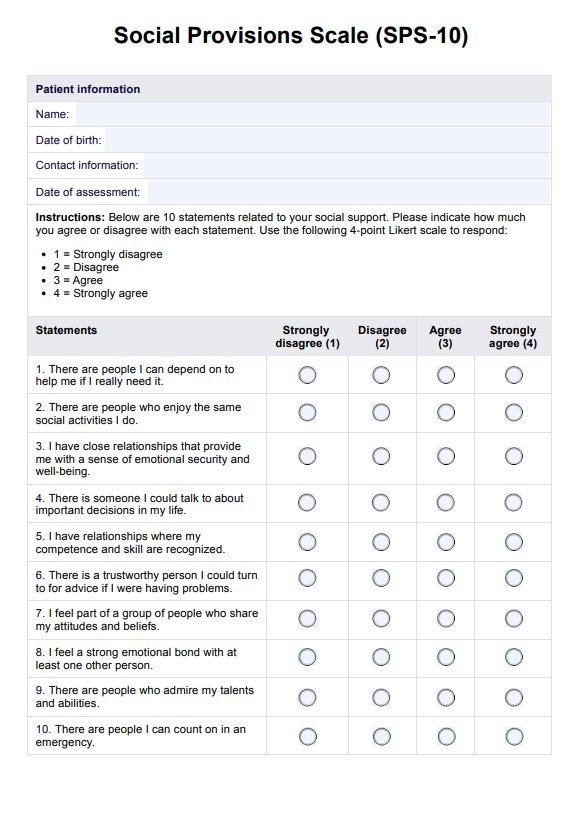
- Social support: Lack of strong social connections and support systems can increase the risk of developing mood disorders (Teo et al., 2013).
- Chronic stress: Persistent exposure to high levels of stress, whether from work, relationships, or other sources, can contribute to the development and exacerbation of mood disorders (Hammen, 2018).
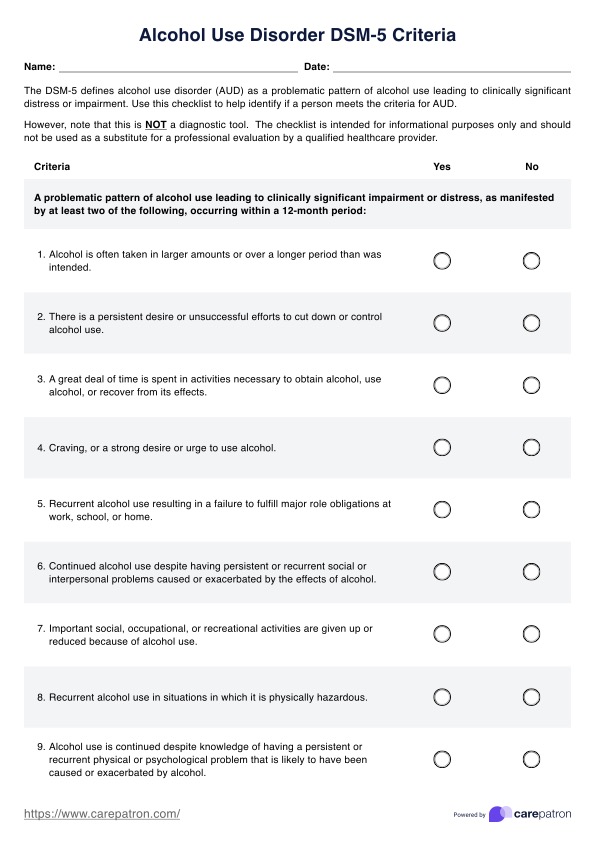
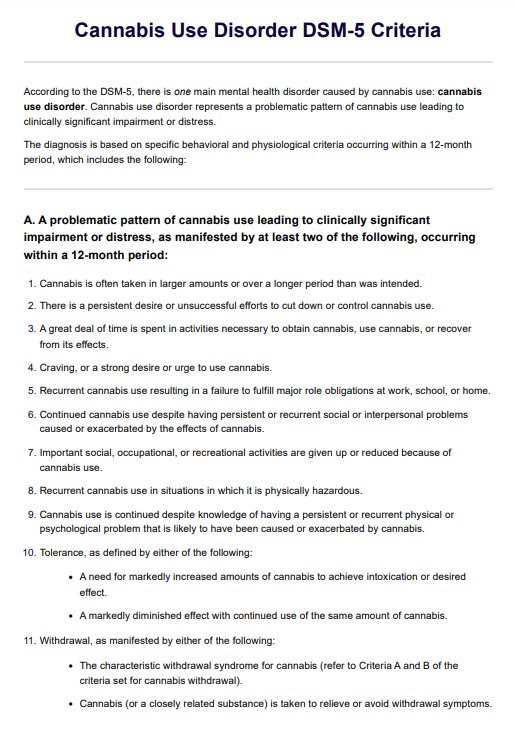
- Substance abuse: The use of certain substances, such as alcohol or drugs, can influence brain chemistry and increase the risk of developing mood disorders or worsen existing conditions.
It's important to note that mood disorders often result from a combination of these factors, and the specific causes may vary from individual to individual. Understanding the underlying causes can help healthcare practitioners develop personalized treatment plans and implement appropriate interventions.
Mood Disorder DSM 5 Criteria Template
Mood Disorder DSM 5 Criteria Example
Types of mood disorders
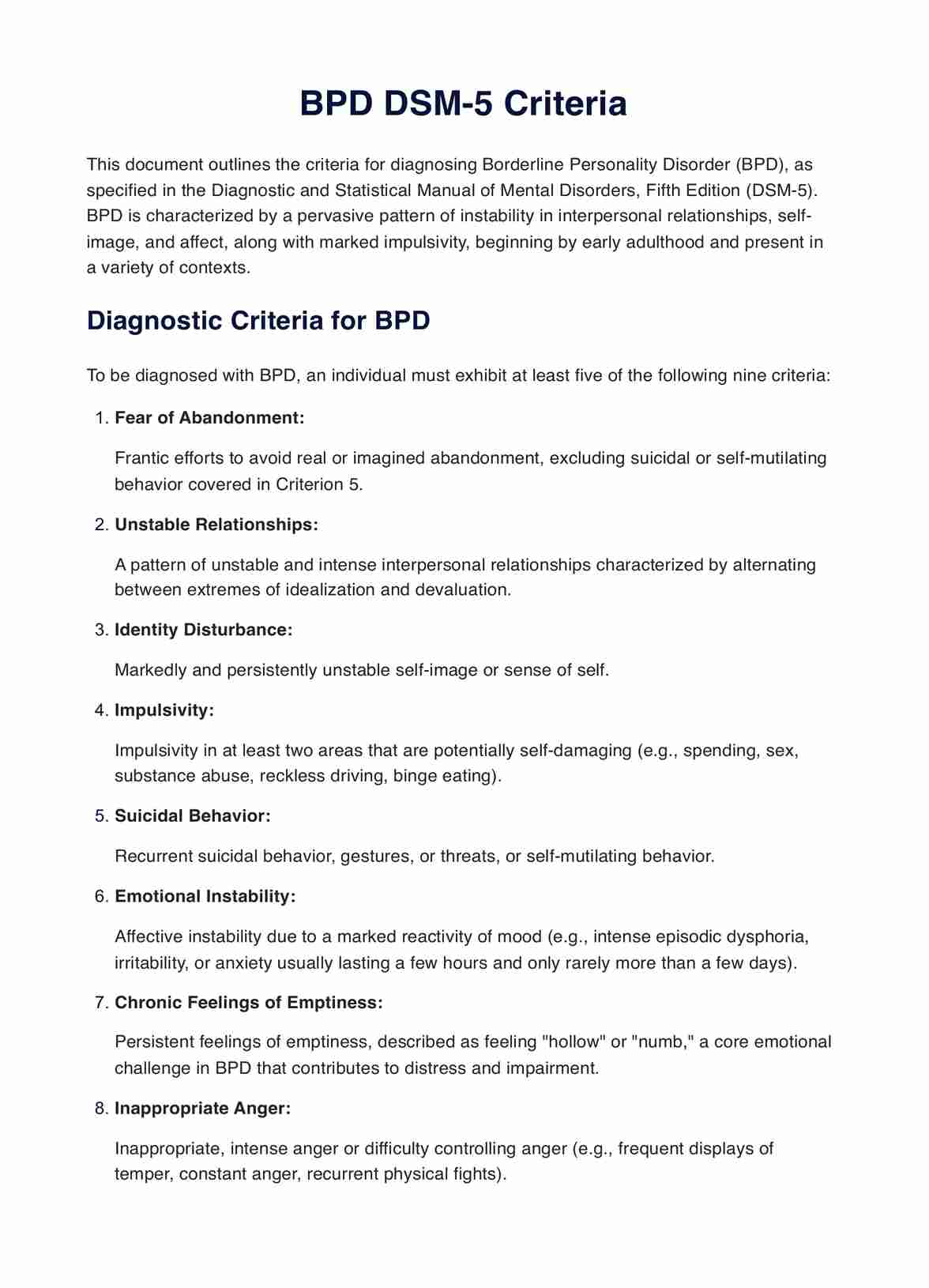
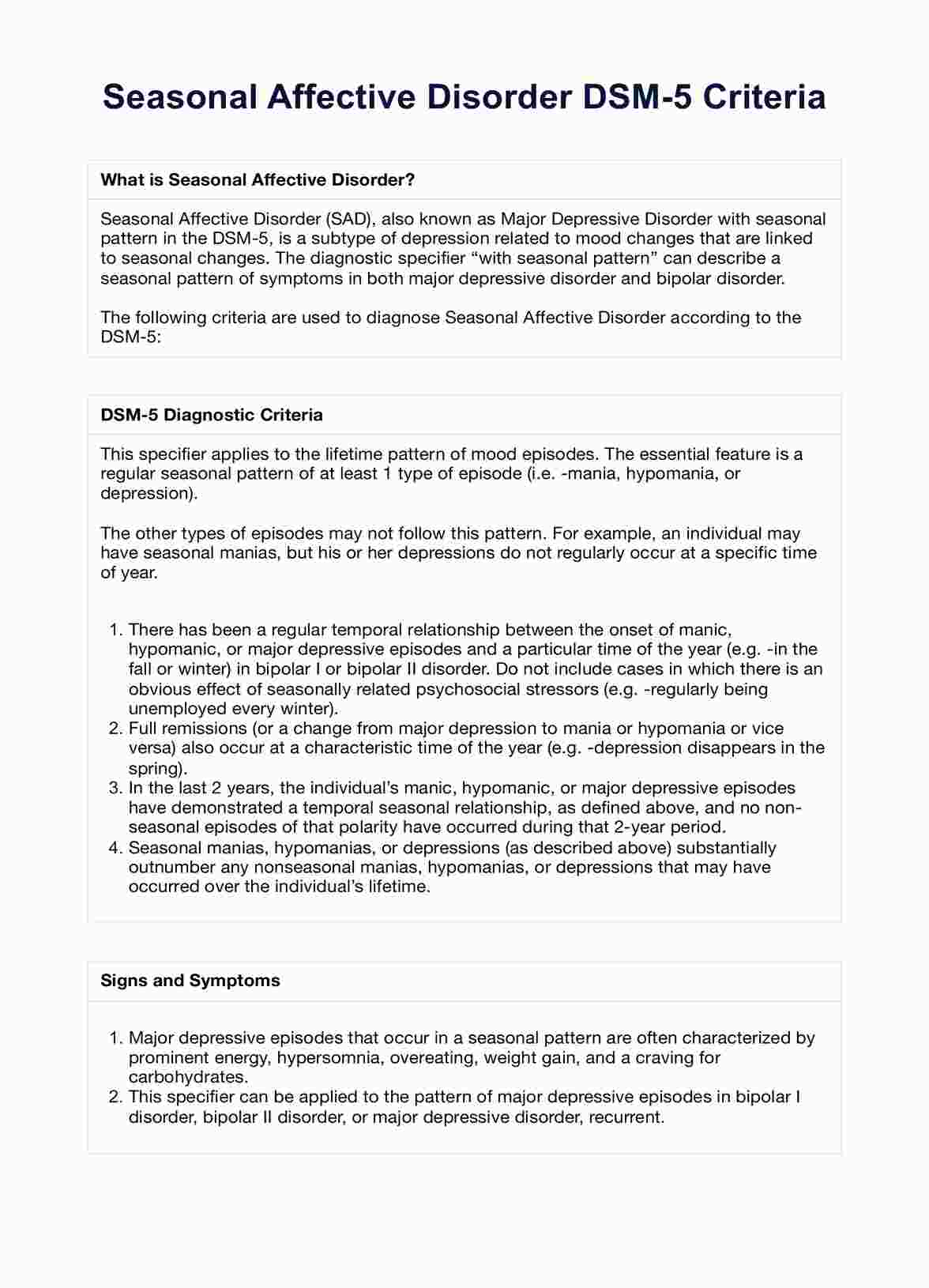
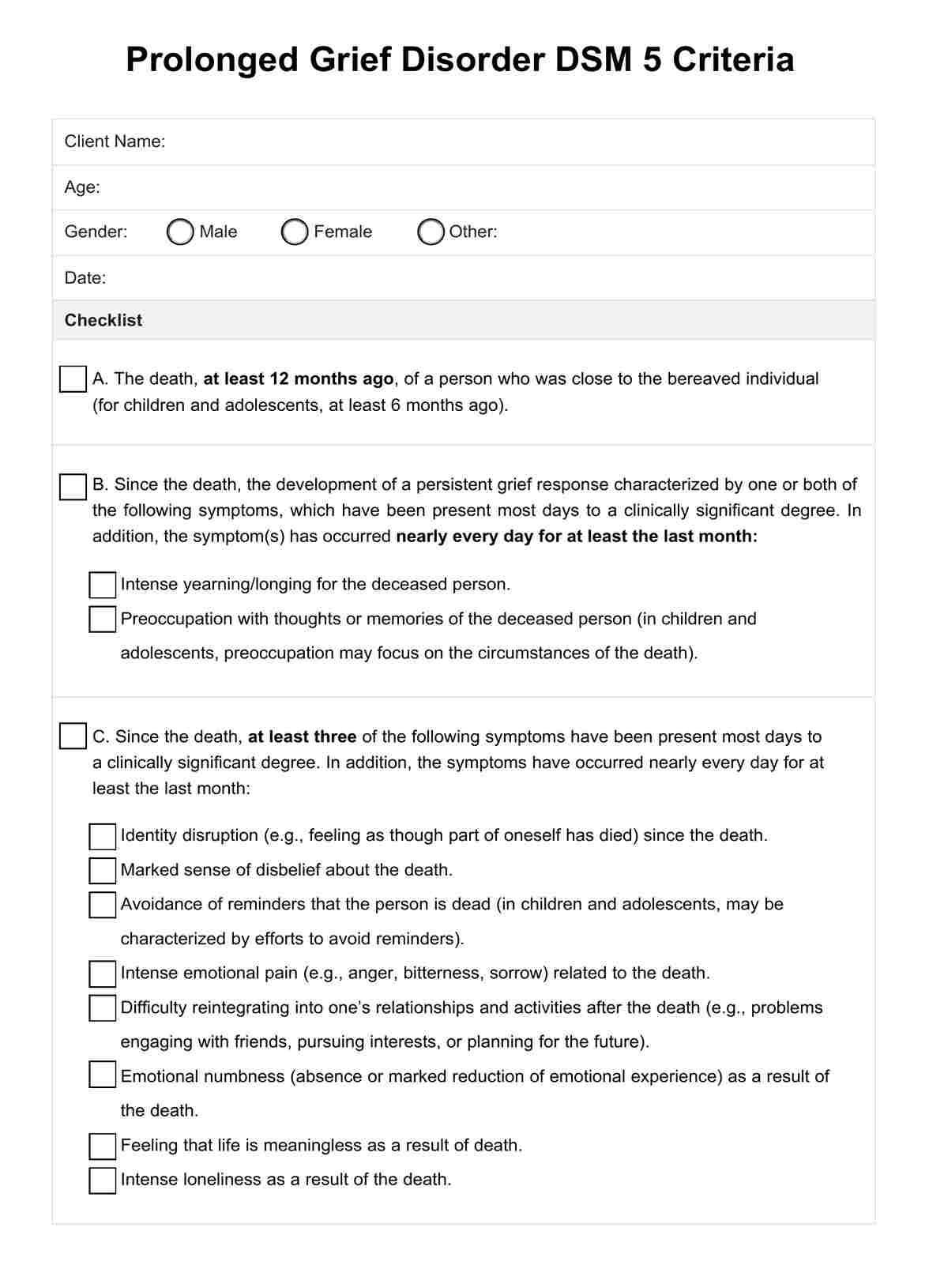
Engaging with the wide range of mood disorders outlined in the DSM-5 can be beneficial in casting a net over these conditions' various presentations. Understanding each disorder's unique characteristics is crucial in accurate diagnosis and effective treatment planning.
Major depressive disorder
This is a mood disorder characterized by persistent feelings of sadness, emptiness, hopelessness, and loss of interest or pleasure in activities once enjoyed. Symptoms include significant weight changes, sleep disturbances, fatigue, feelings of worthlessness or guilt, difficulty concentrating, and recurrent thoughts of death or suicidal ideation.
Persistent depressive disorder (dysthymia)
Dysthymia is a chronic form of depression with less severe but long-lasting symptoms lasting for at least two years. Individuals experience a depressed mood for most of the day, along with other depressive symptoms like low self-esteem, poor concentration, and feelings of hopelessness.
Disruptive mood dysregulation disorder
This refers to a childhood disorder characterized by persistent irritability and frequent, severe temper outbursts that are disproportionate to the situation and inconsistent with the child's developmental level.
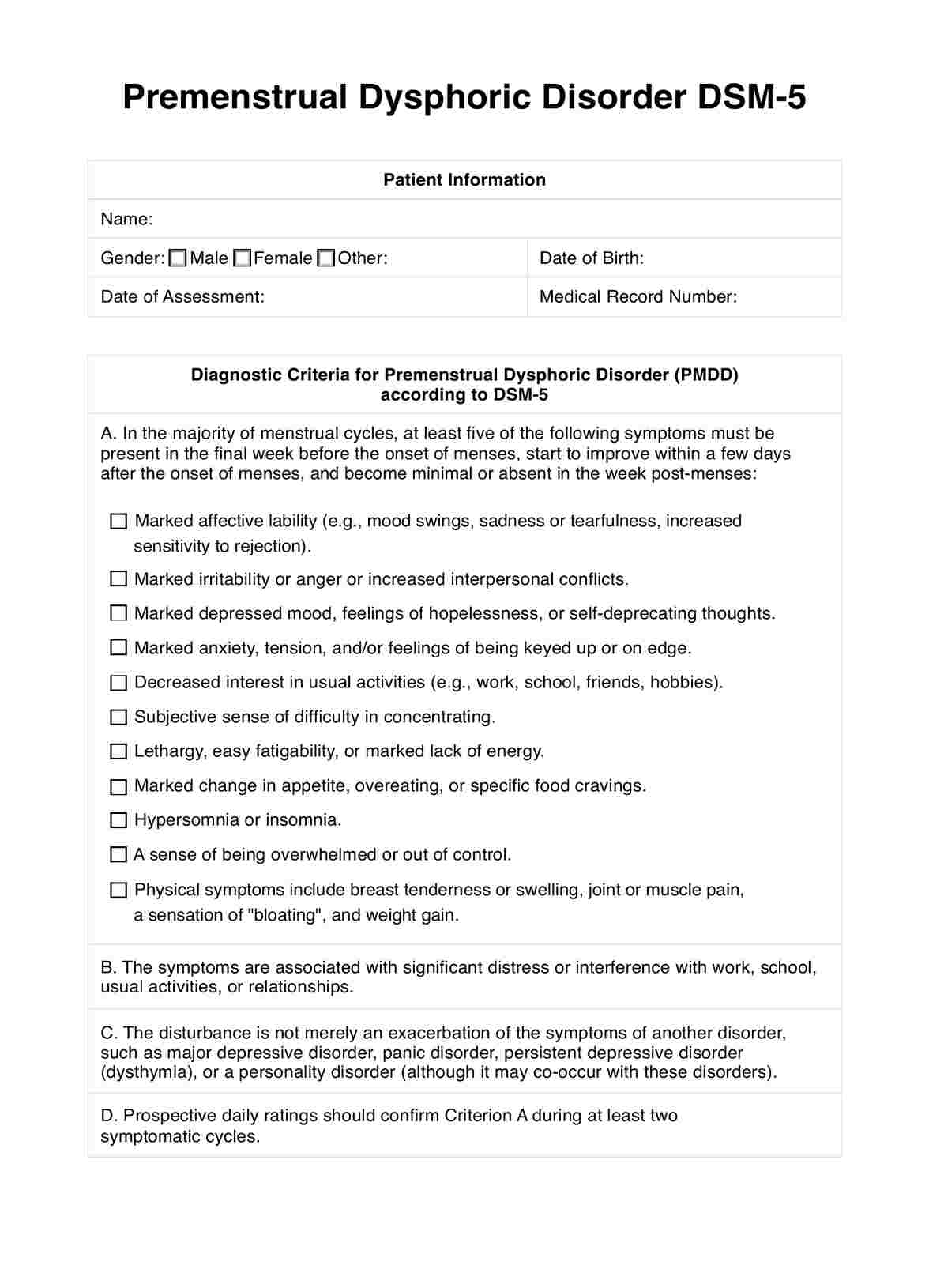
Premenstrual dysphoric disorder
This condition is marked by severe mood disturbances, irritability, and physical symptoms that occur during the luteal phase of the menstrual cycle and remit after the onset of menses.
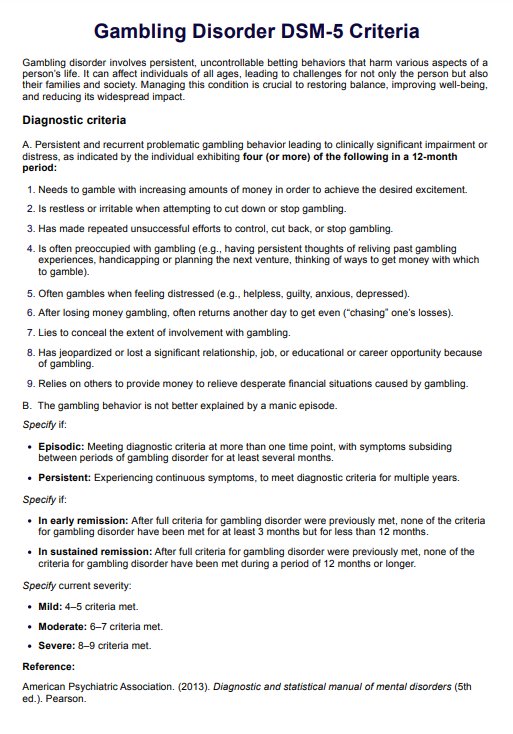
Substance/medication-induced depressive disorder
This depressive disorder results from the physiological effects of a substance (e.g., alcohol, drugs) or medication.
Depressive disorder due to another medical condition
Another medical condition, such as a neurological or endocrine disorder, directly causes this depressive disorder.
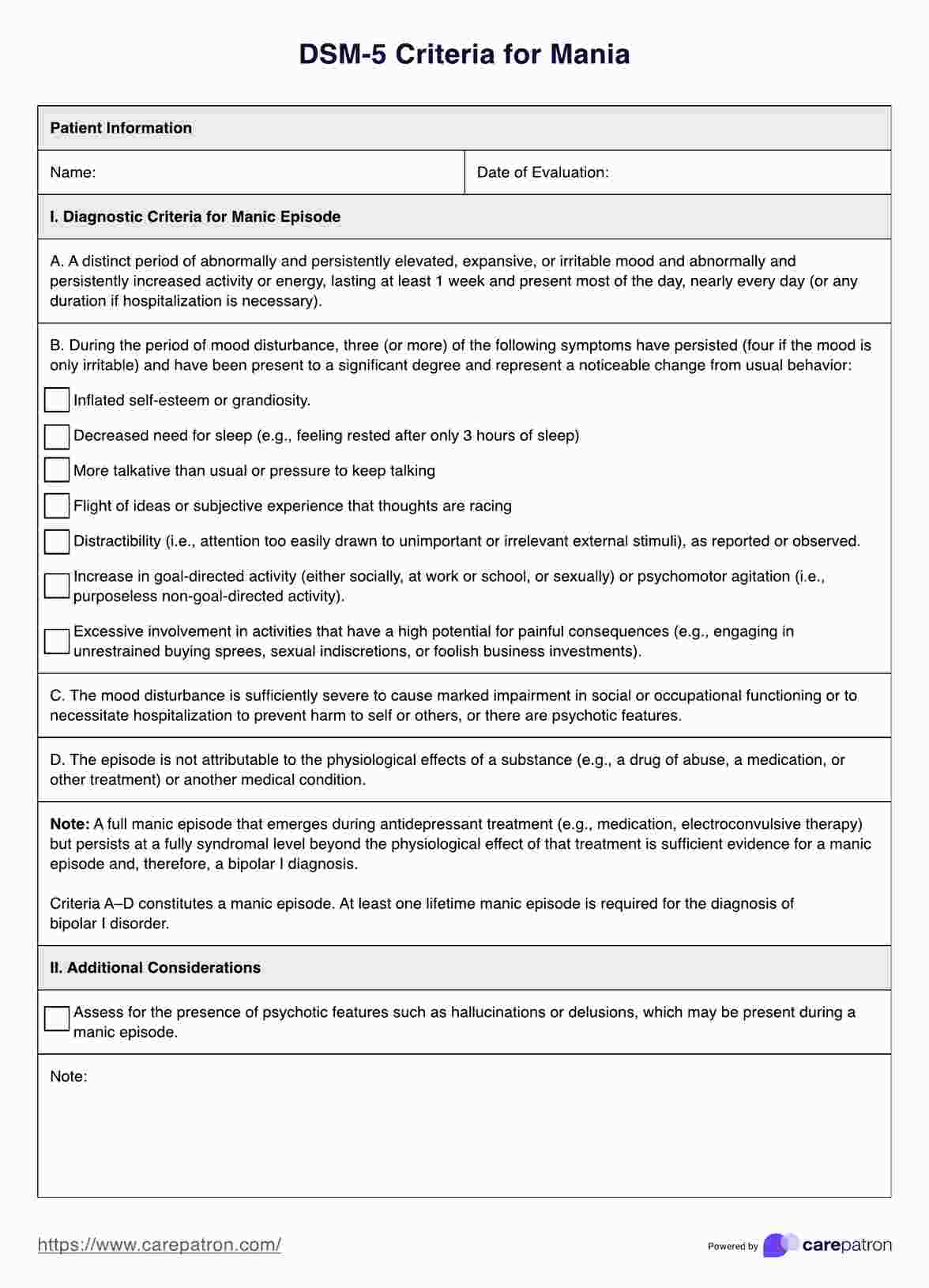
Bipolar I disorder
Bipolar I disorder is characterized by the occurrence of at least one manic episode, which may alternate with episodes of major depression. Manic episodes involve elevated or irritable mood, increased energy levels, inflated self-esteem, decreased need for sleep, racing thoughts, and impulsive or risky behaviors.
Bipolar II disorder
This involves the occurrence of at least one hypomanic episode (a less severe form of mania) and at least one major depressive episode.
Cyclothymic disorder
This is a chronic disorder involving numerous periods of hypomanic and depressive symptoms but not meeting the full criteria for a manic or major depressive episode.
Substance/medication-induced bipolar and related disorder
A bipolar and related disorder resulting from the physiological effects of a substance (e.g., alcohol, drugs) or medication.
Bipolar and related disorder due to another medical condition
Another medical condition, such as a neurological or endocrine disorder, directly causes a bipolar and related disorder.
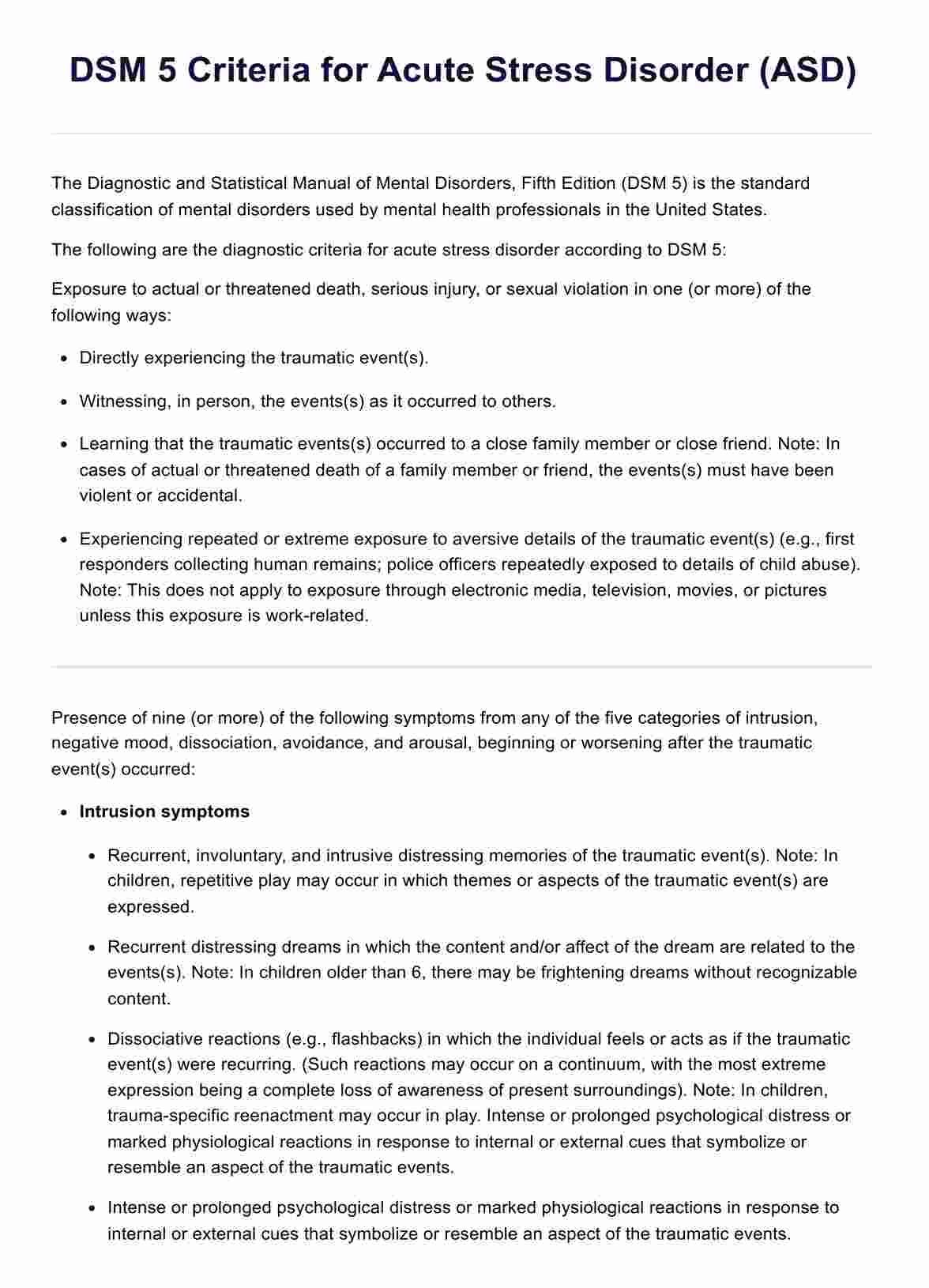
How do healthcare professionals diagnose mood disorders?
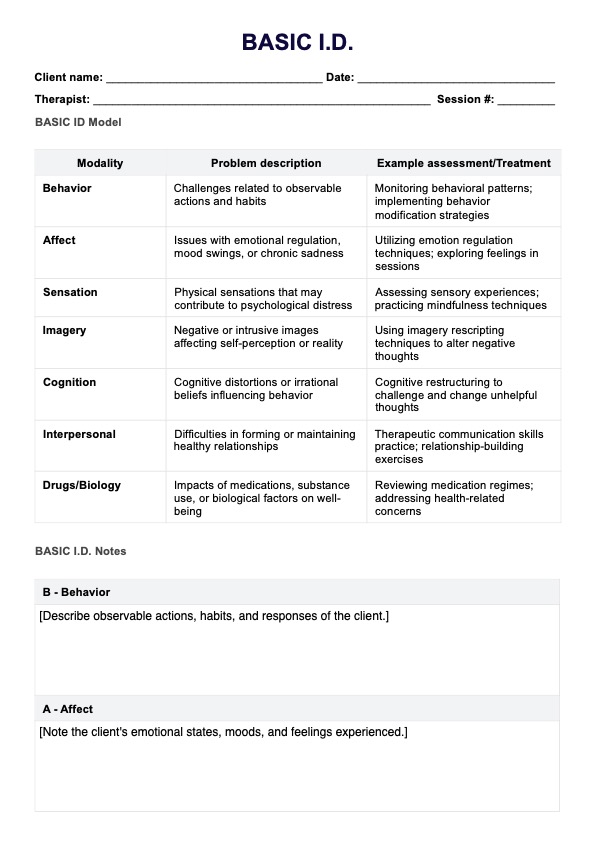
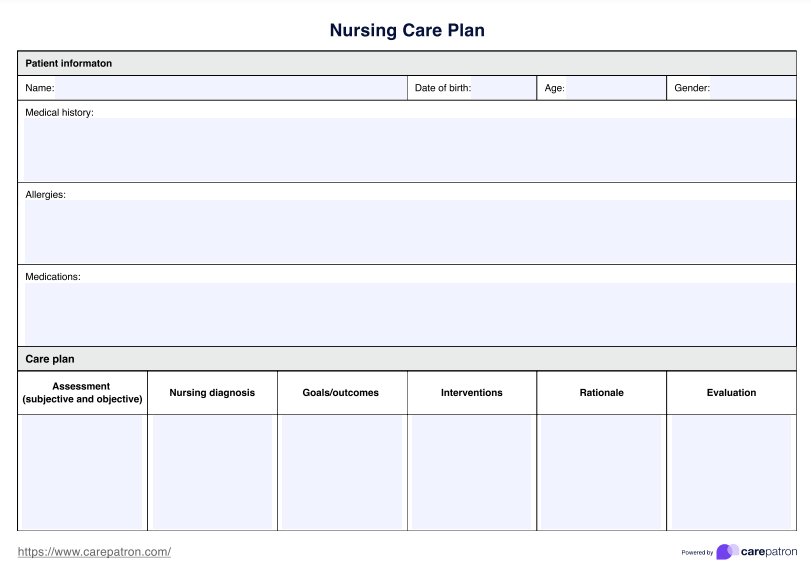
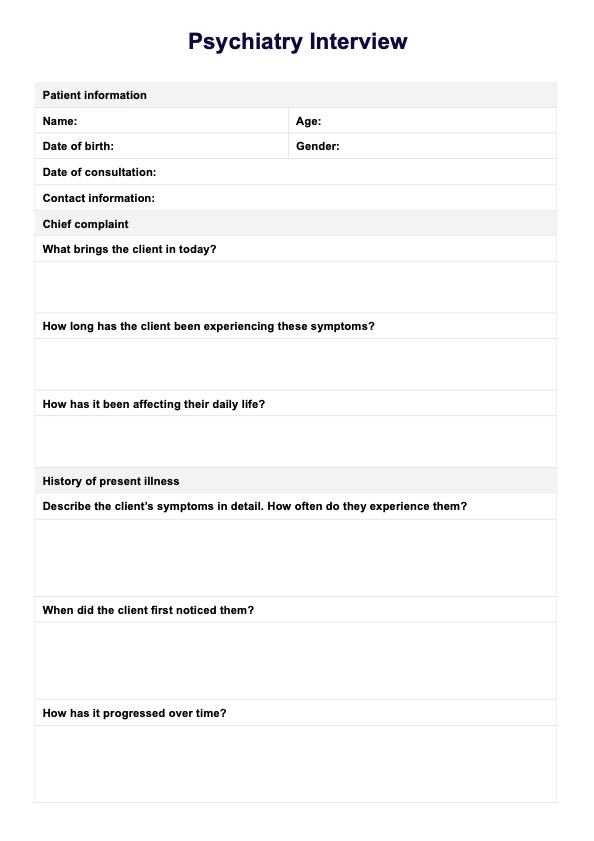
Healthcare professionals diagnose mood disorders by carefully evaluating a patient's symptoms, medical history, and mental health status. The process typically involves the following steps:
Step 1: Clinical interview
The healthcare professional will conduct a comprehensive clinical interview to gather information about the patient's symptoms, duration, severity, and impact on daily functioning. They will also inquire about the patient's personal and family medical history and any potential environmental or life stressors.
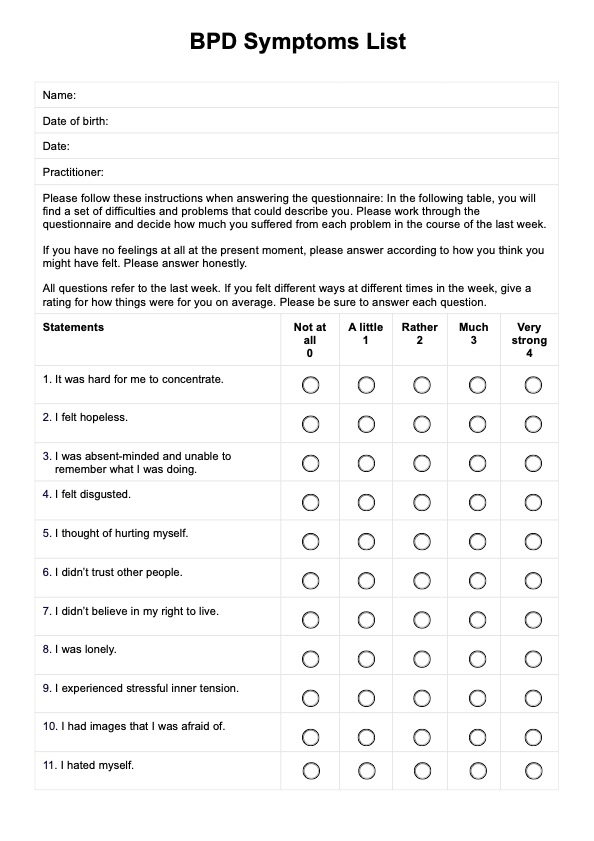
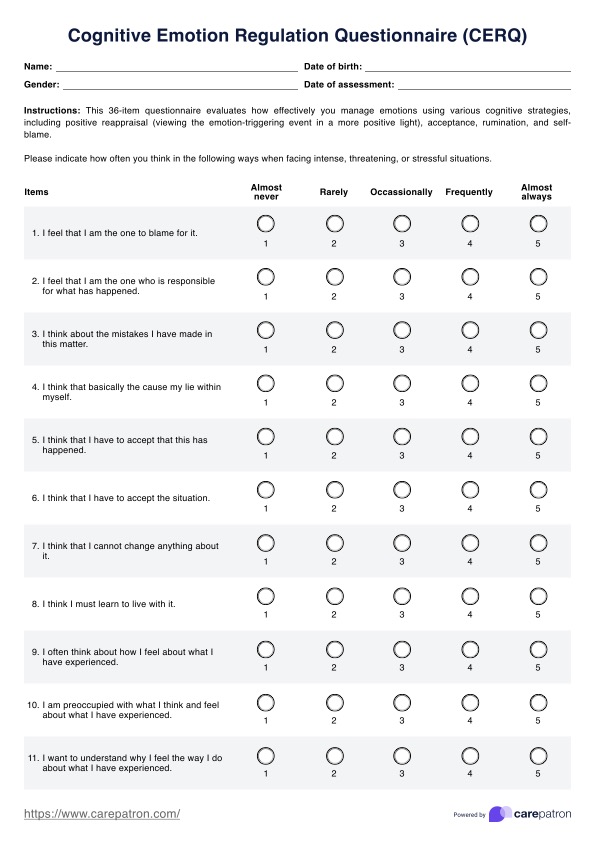
Step 2: Symptom assessment
Based on the clinical interview, the healthcare professional will assess whether the patient meets the specific diagnostic criteria for a mood disorder, as outlined in the DSM-5.
Step 3: Differential diagnosis
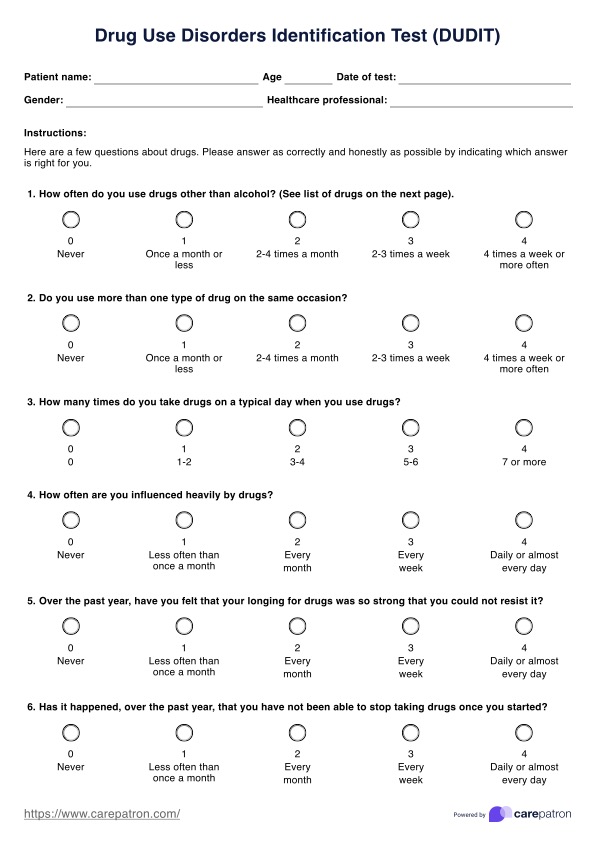
It is essential to rule out other potential causes of the patient's symptoms, such as medical conditions, substance use disorders, or other mental health disorders. The healthcare professional may order laboratory tests and physical examinations to ensure an accurate diagnosis.
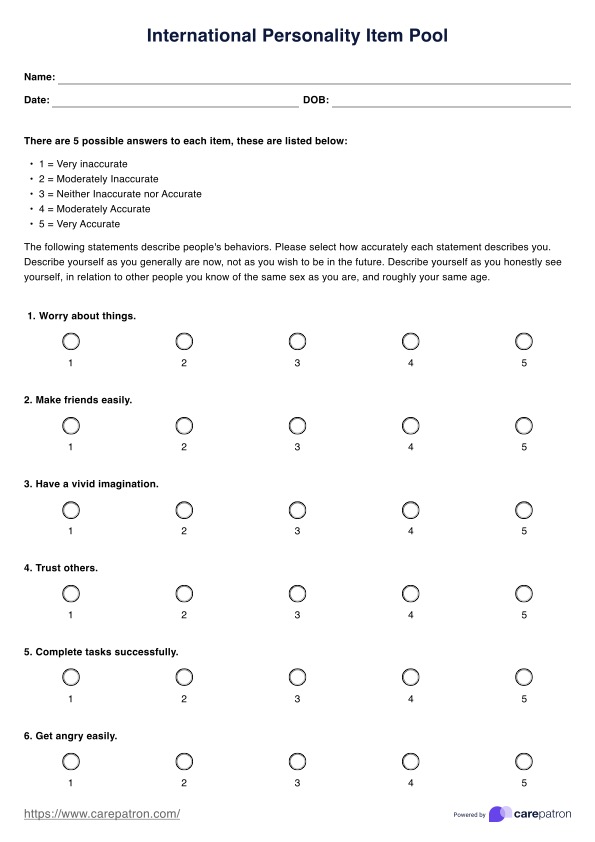
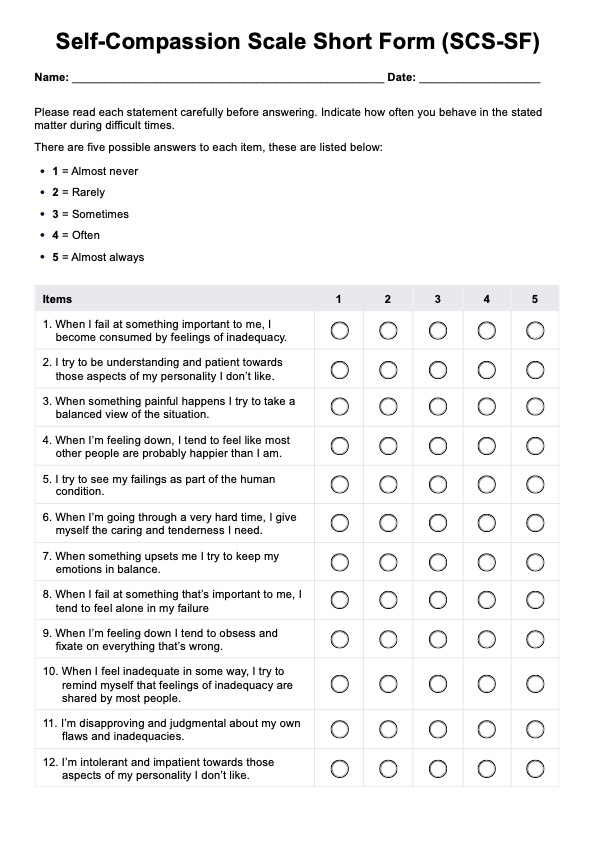
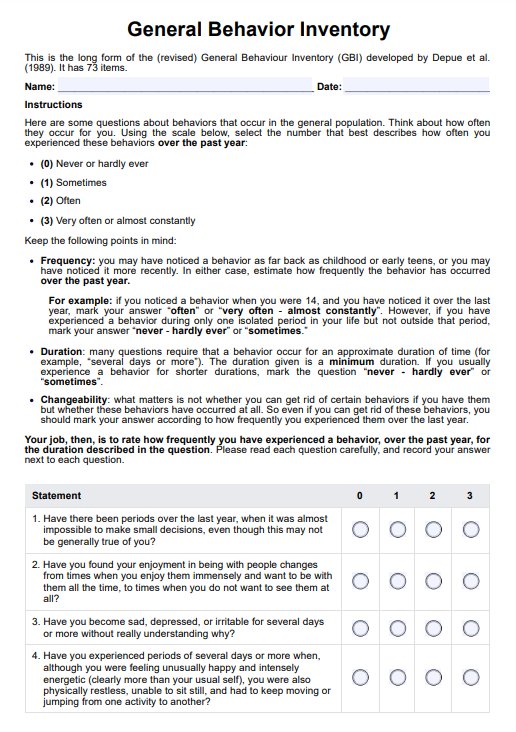
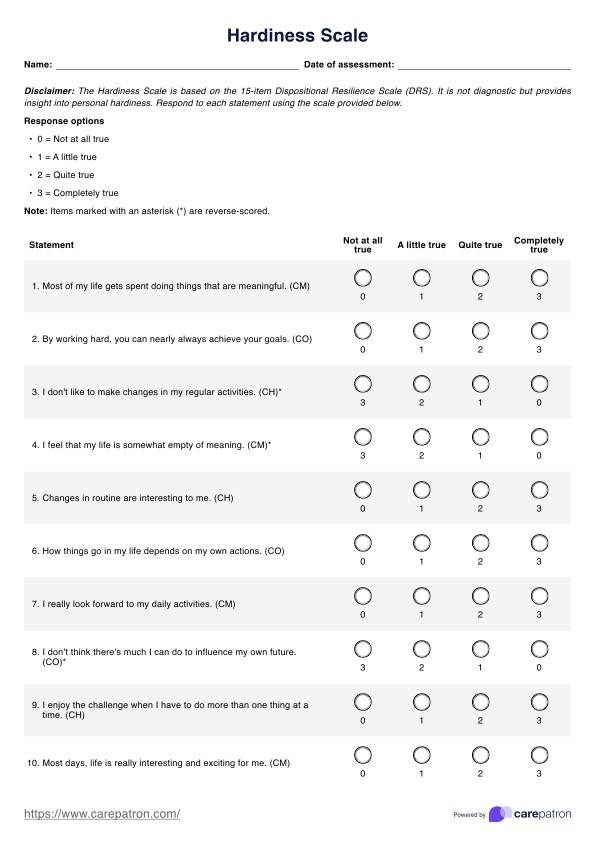
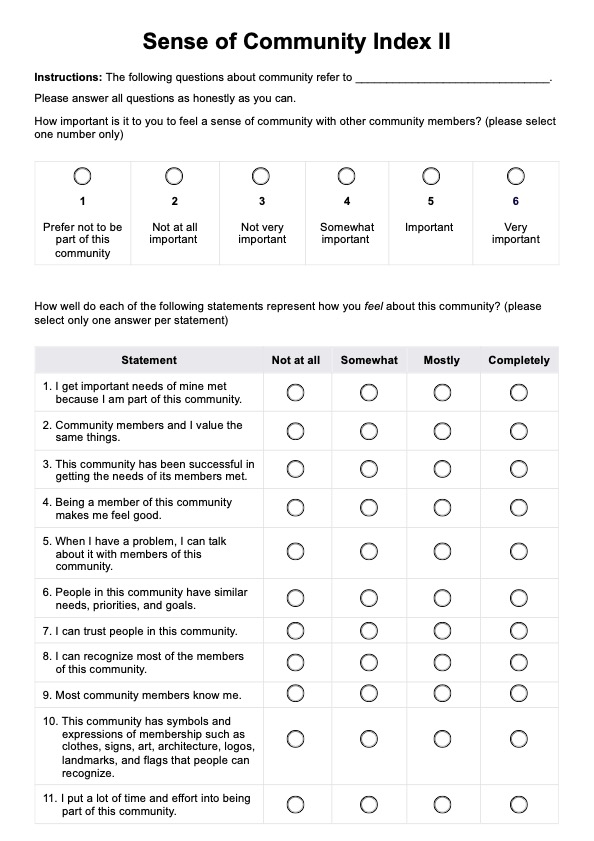
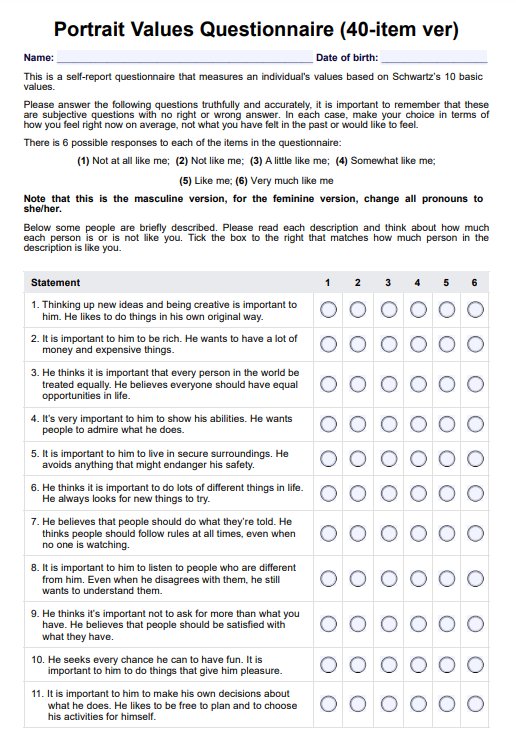
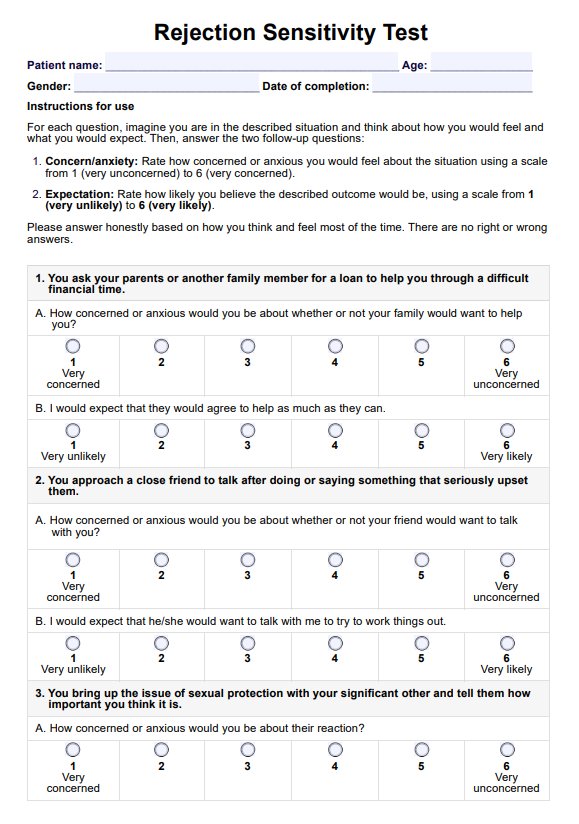
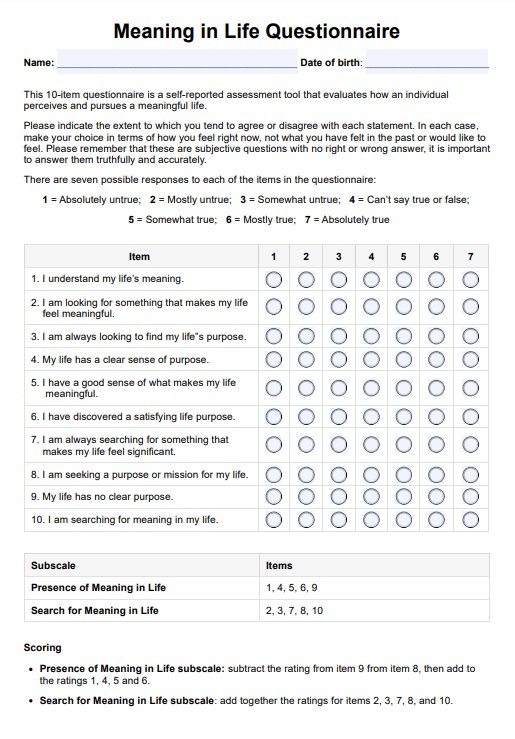
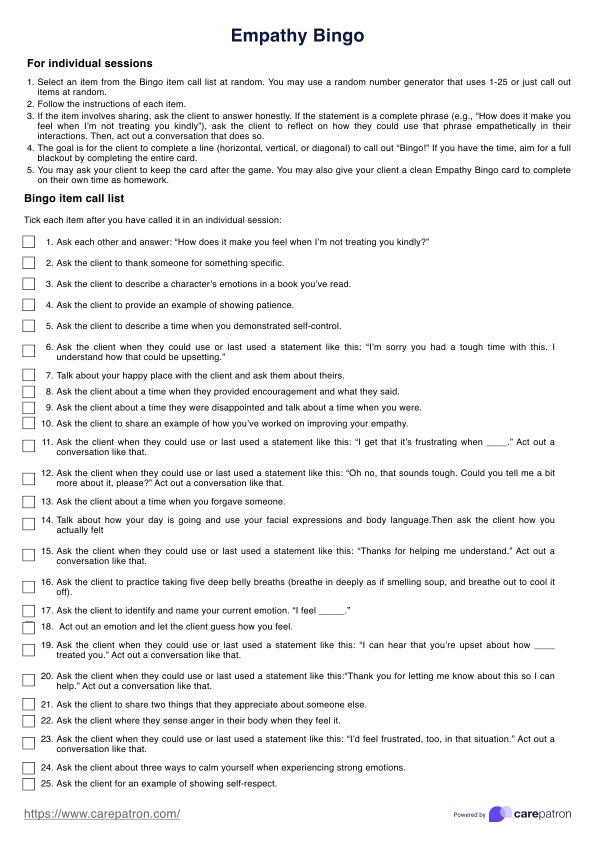
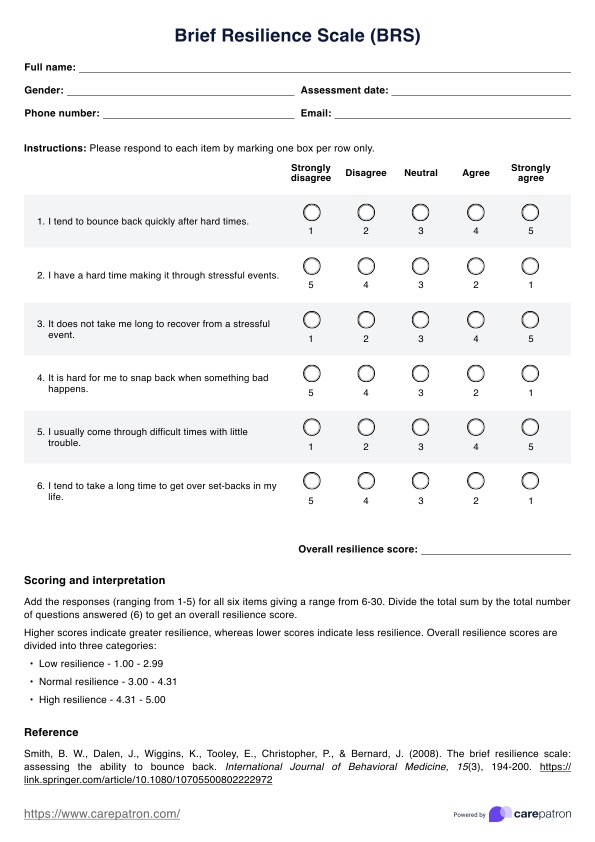
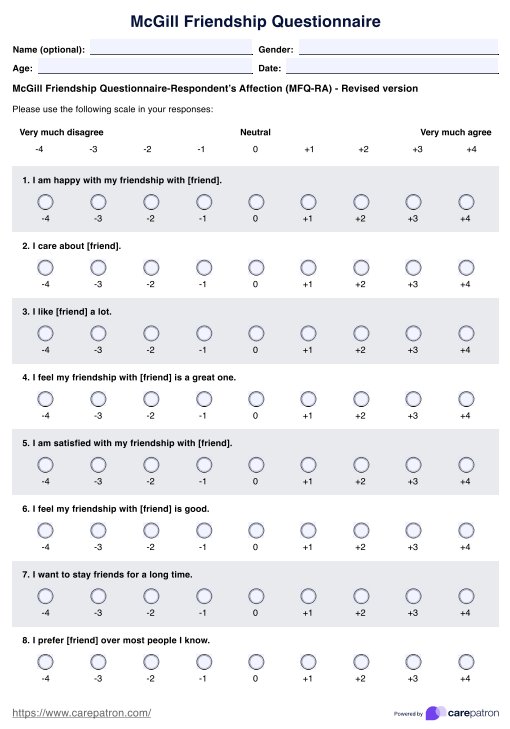
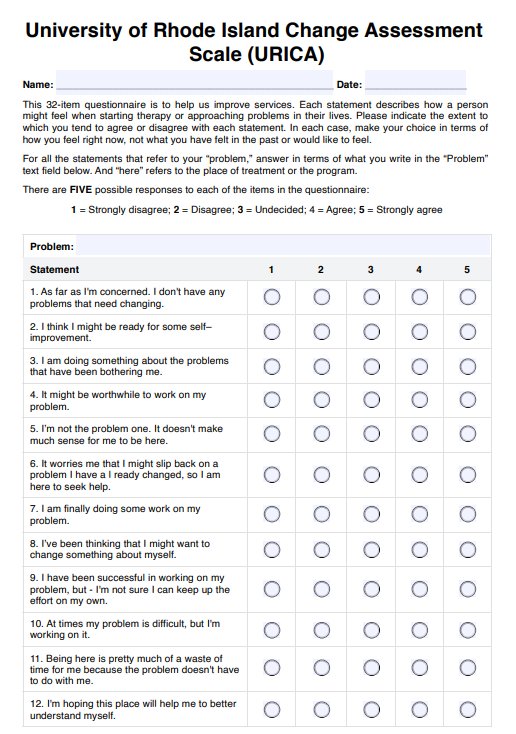
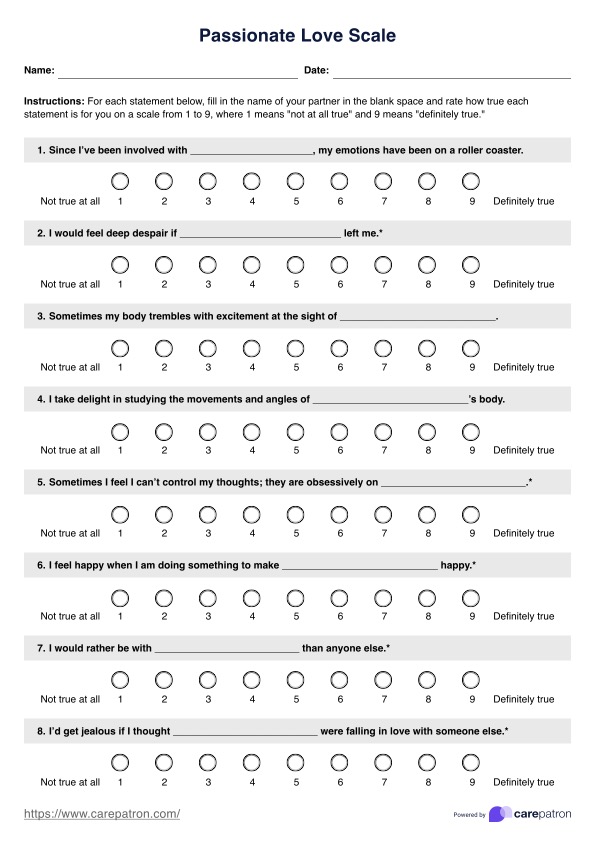
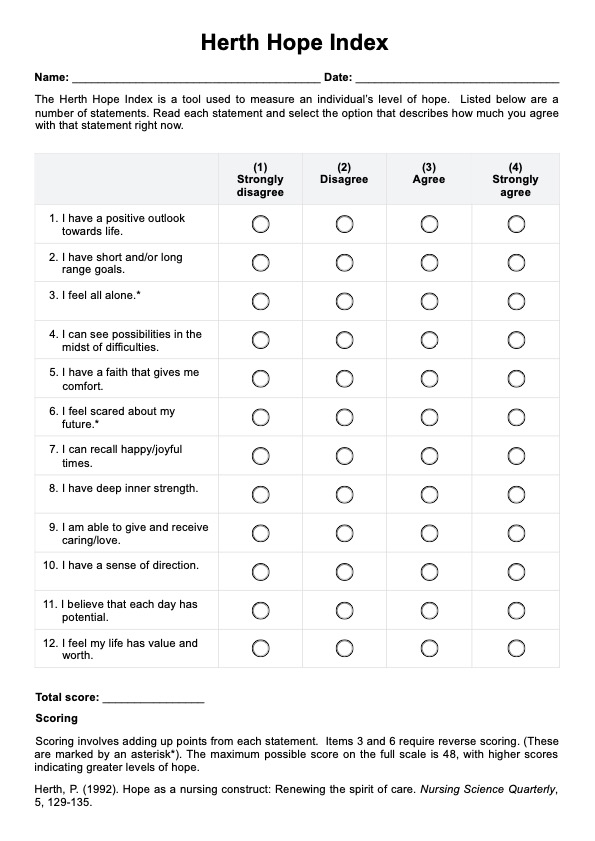
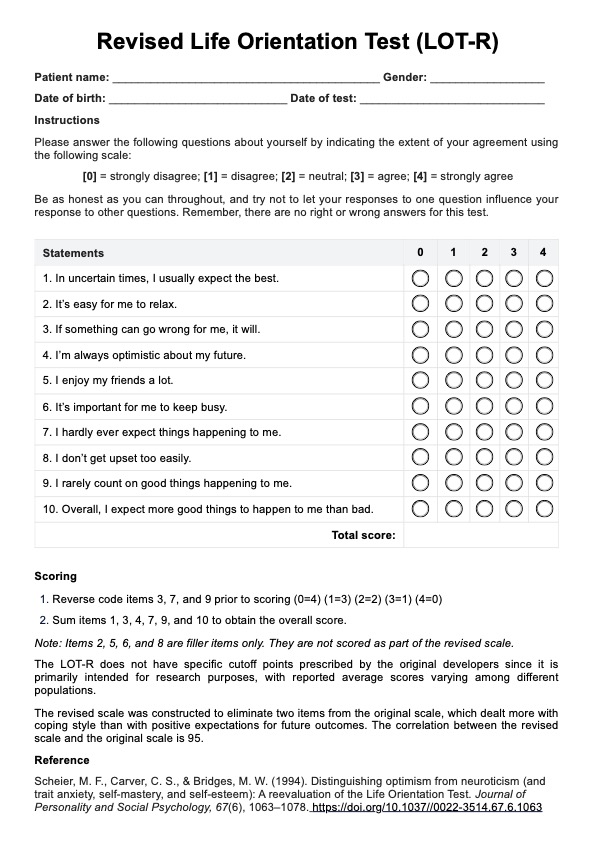
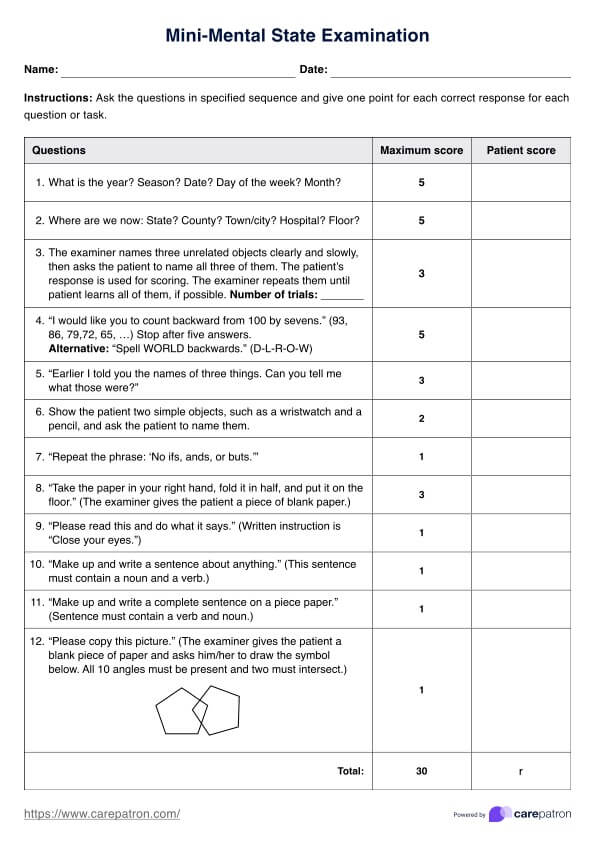
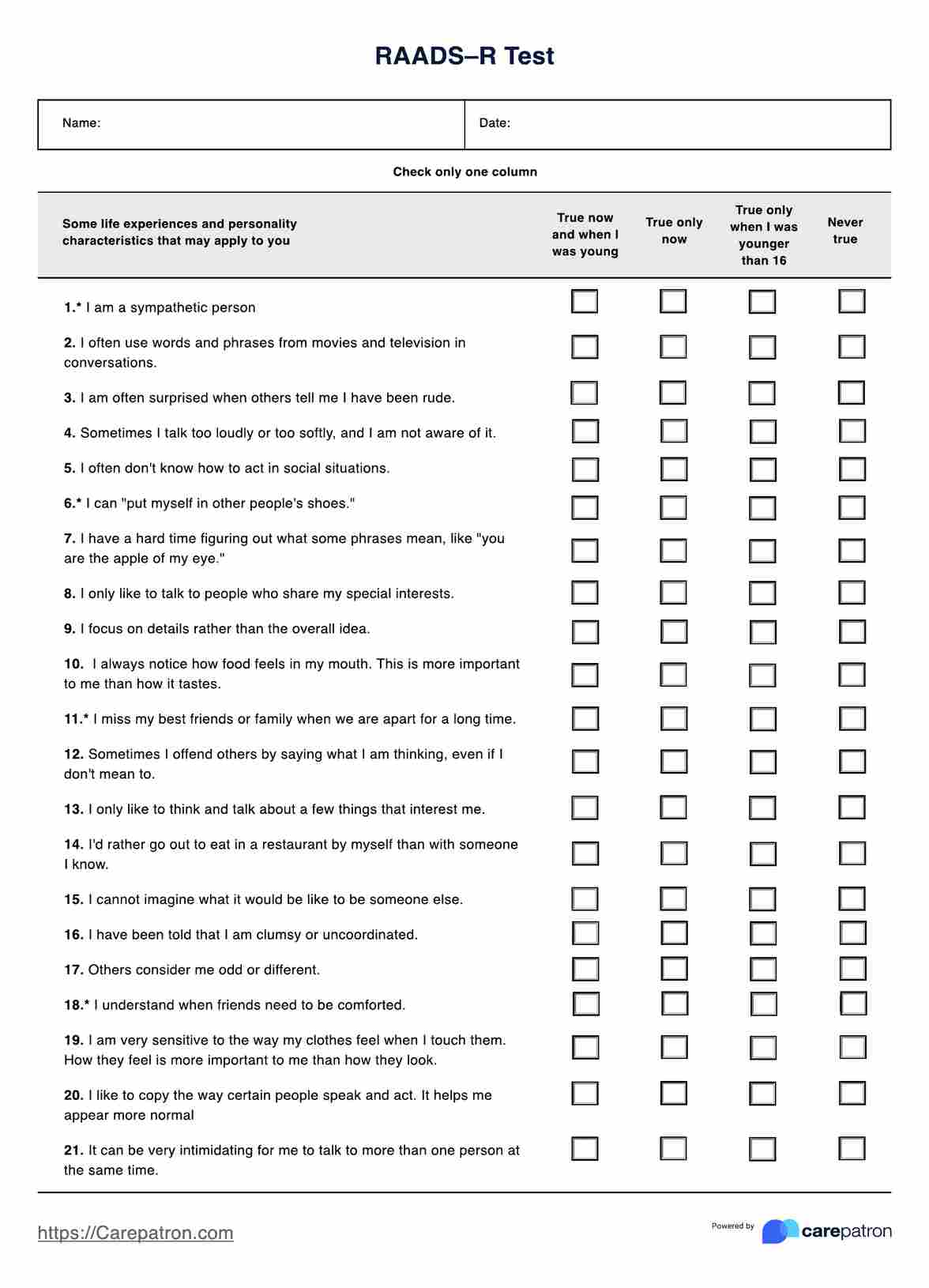
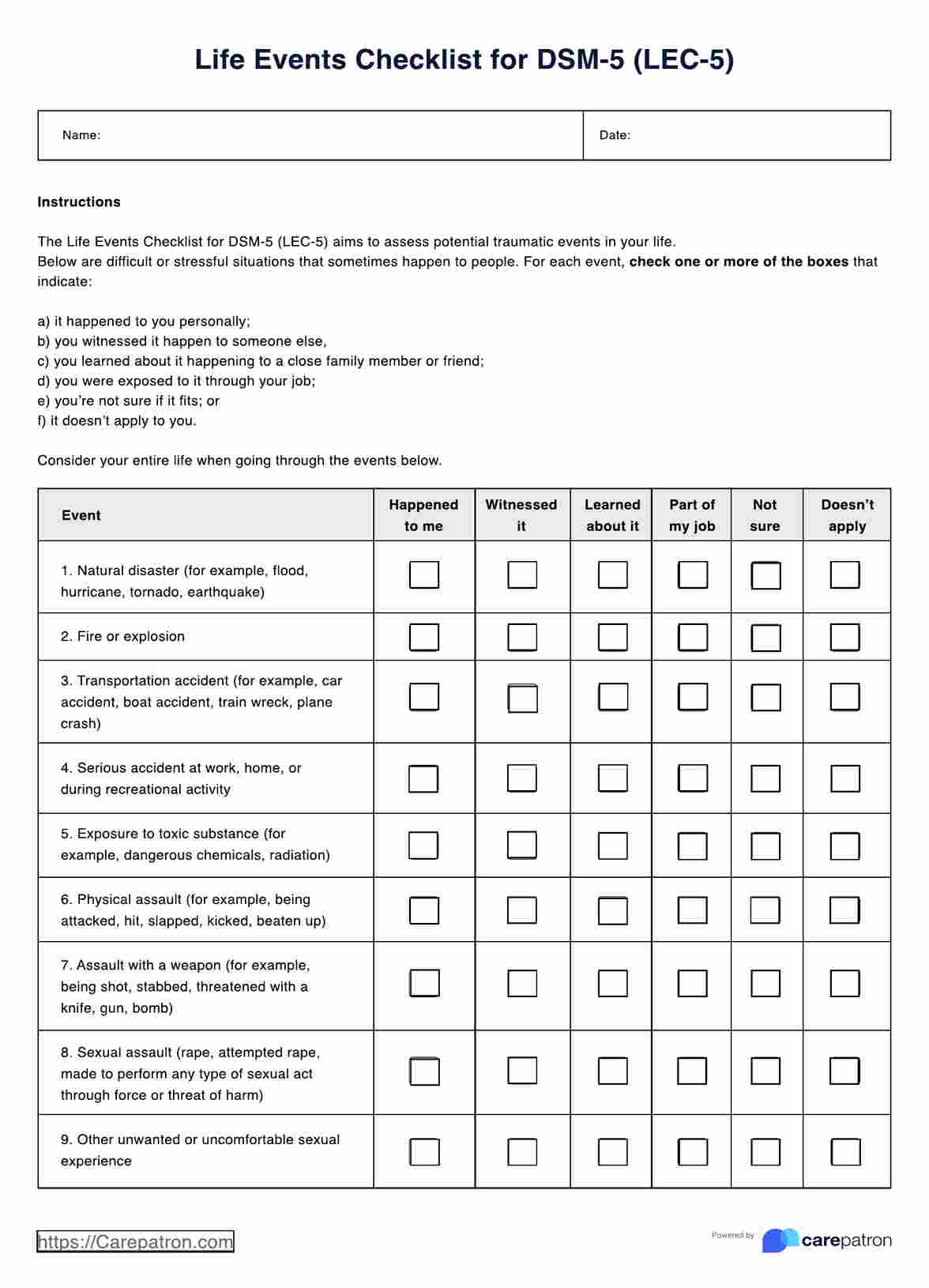
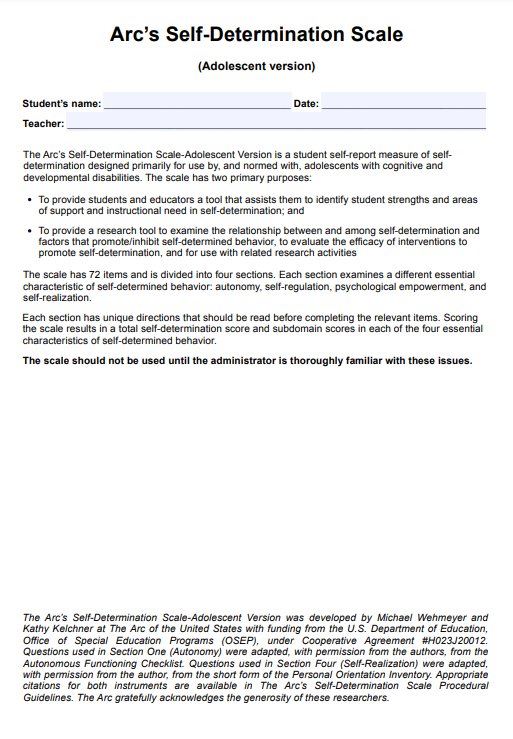
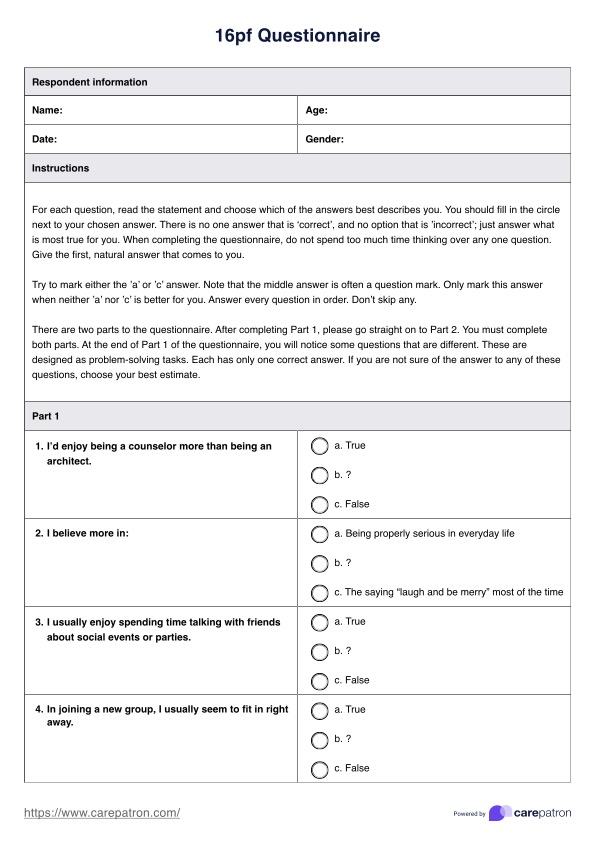
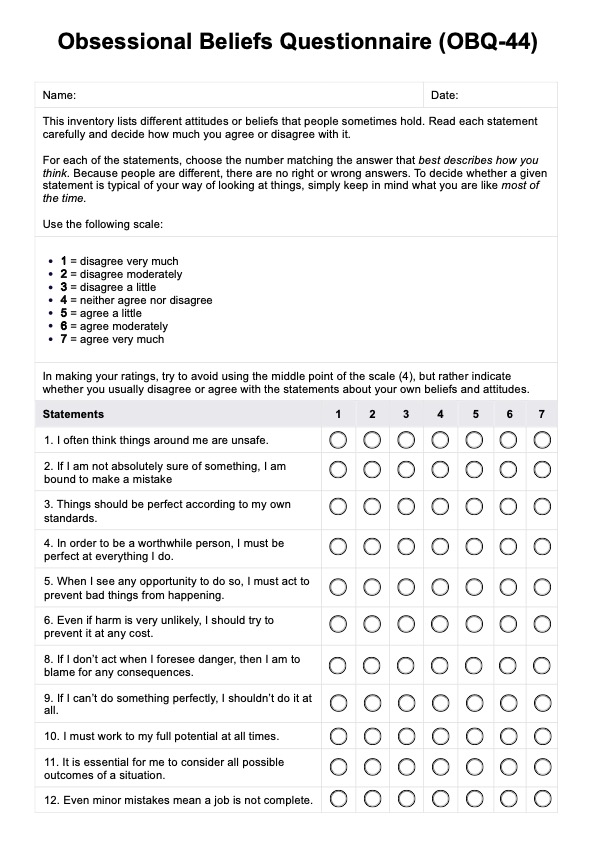
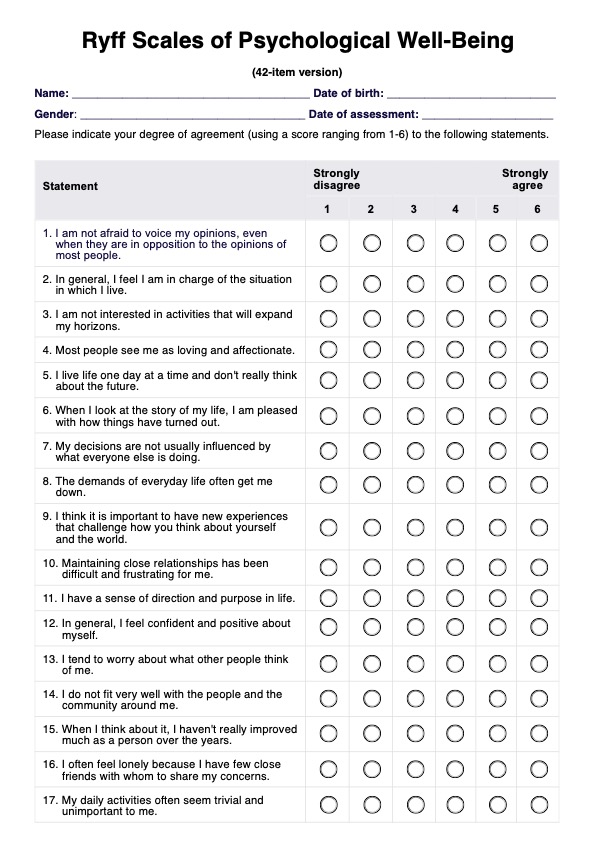
Step 4: Screening tools
Healthcare professionals may use standardized screening tools or questionnaires to assess the severity of the patient's symptoms and monitor their progress over time. Examples include the Patient Health Questionnaire (PHQ-9) for depression and the Mood Disorder Questionnaire (MDQ) for bipolar disorder.
Step 5: Functional assessment
The healthcare professional will evaluate the impact of the mood disorder on the patient's daily functioning, including their ability to work, study, maintain relationships, and engage in self-care activities.
Use the Patient Health Questionnaire Template which provides a comprehensive tool for evaluating general mental health. Complement it with the Clinical Interview Template to gather detailed patient history and insights for a well-rounded assessment.
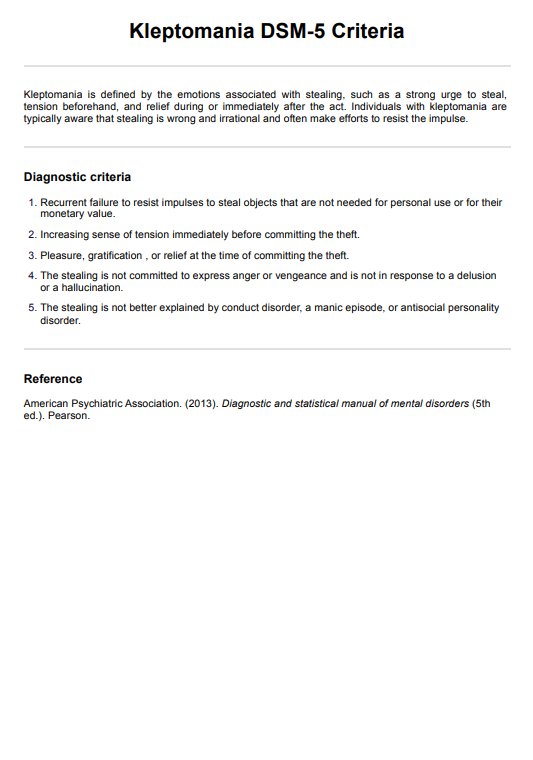
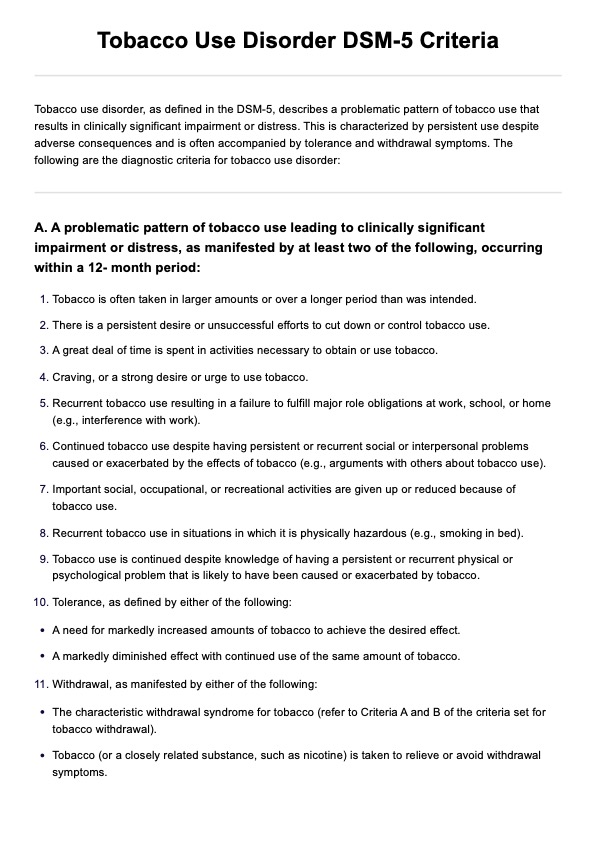
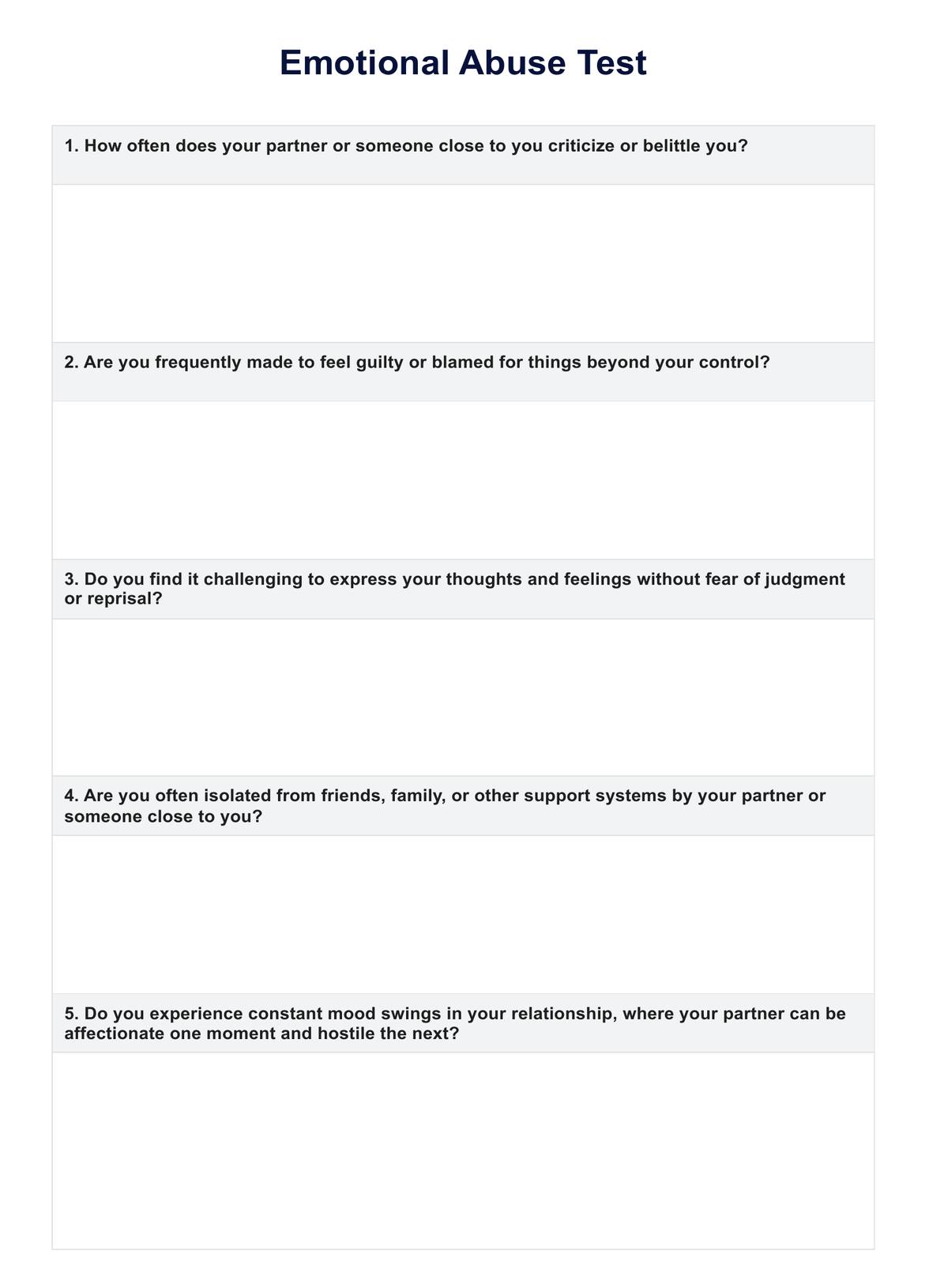
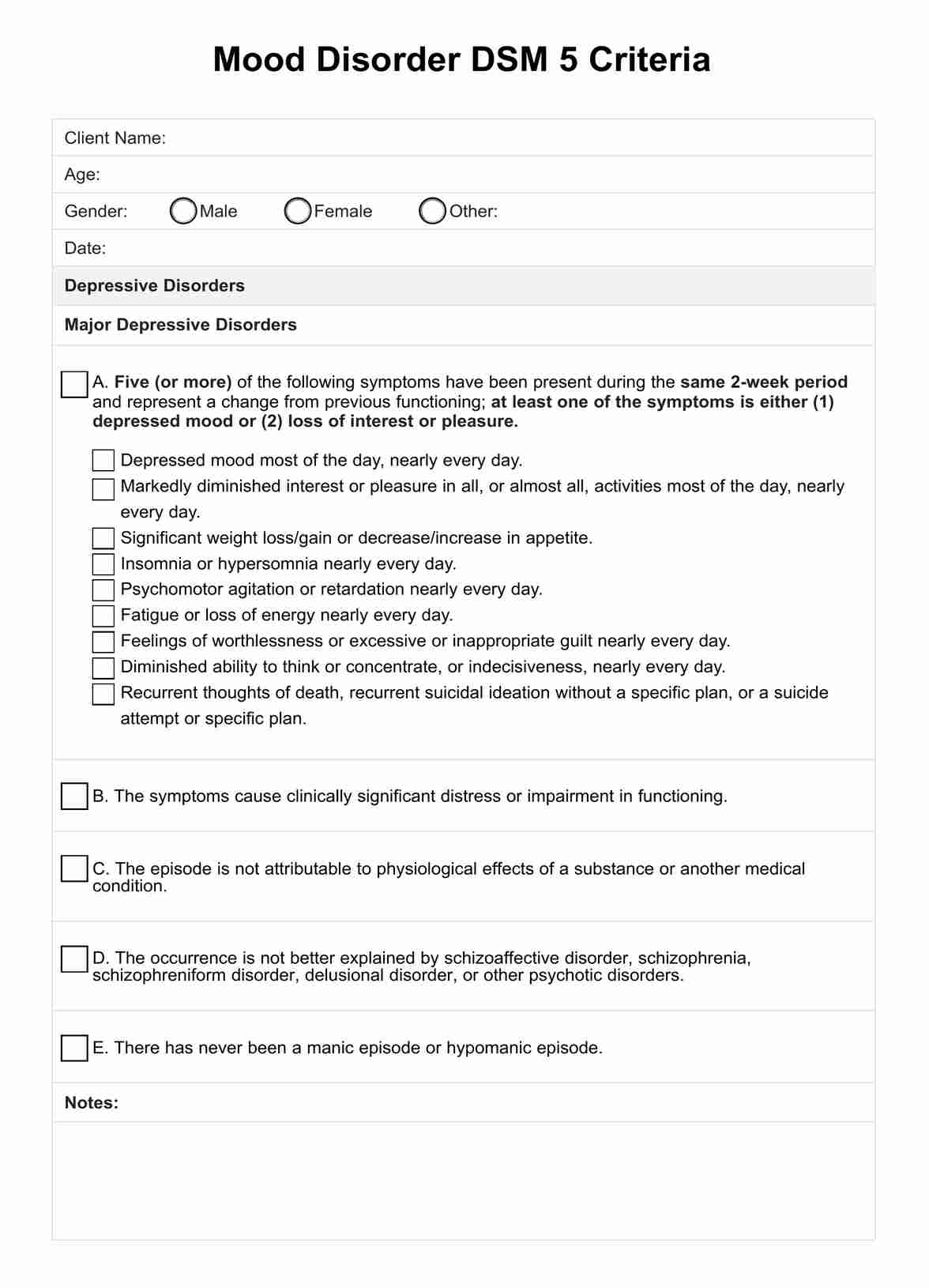
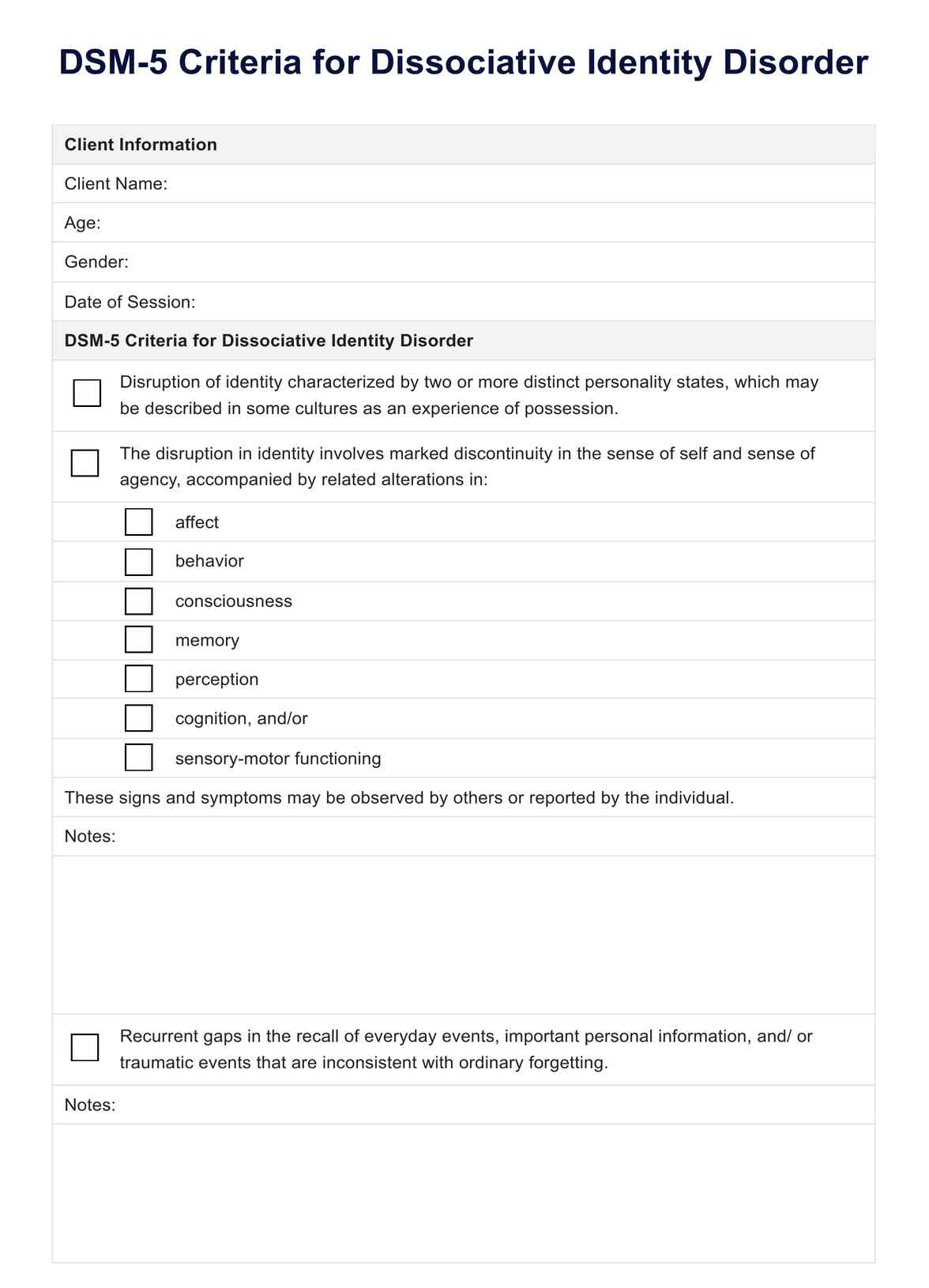
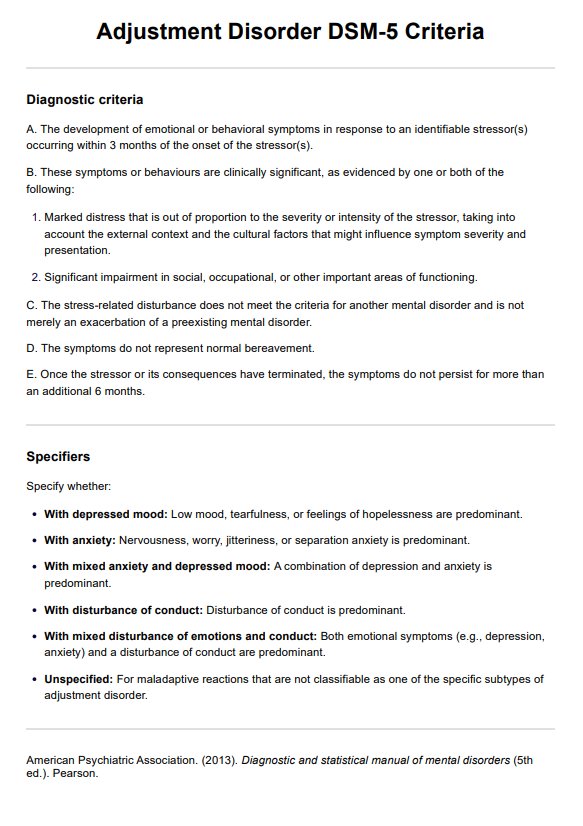
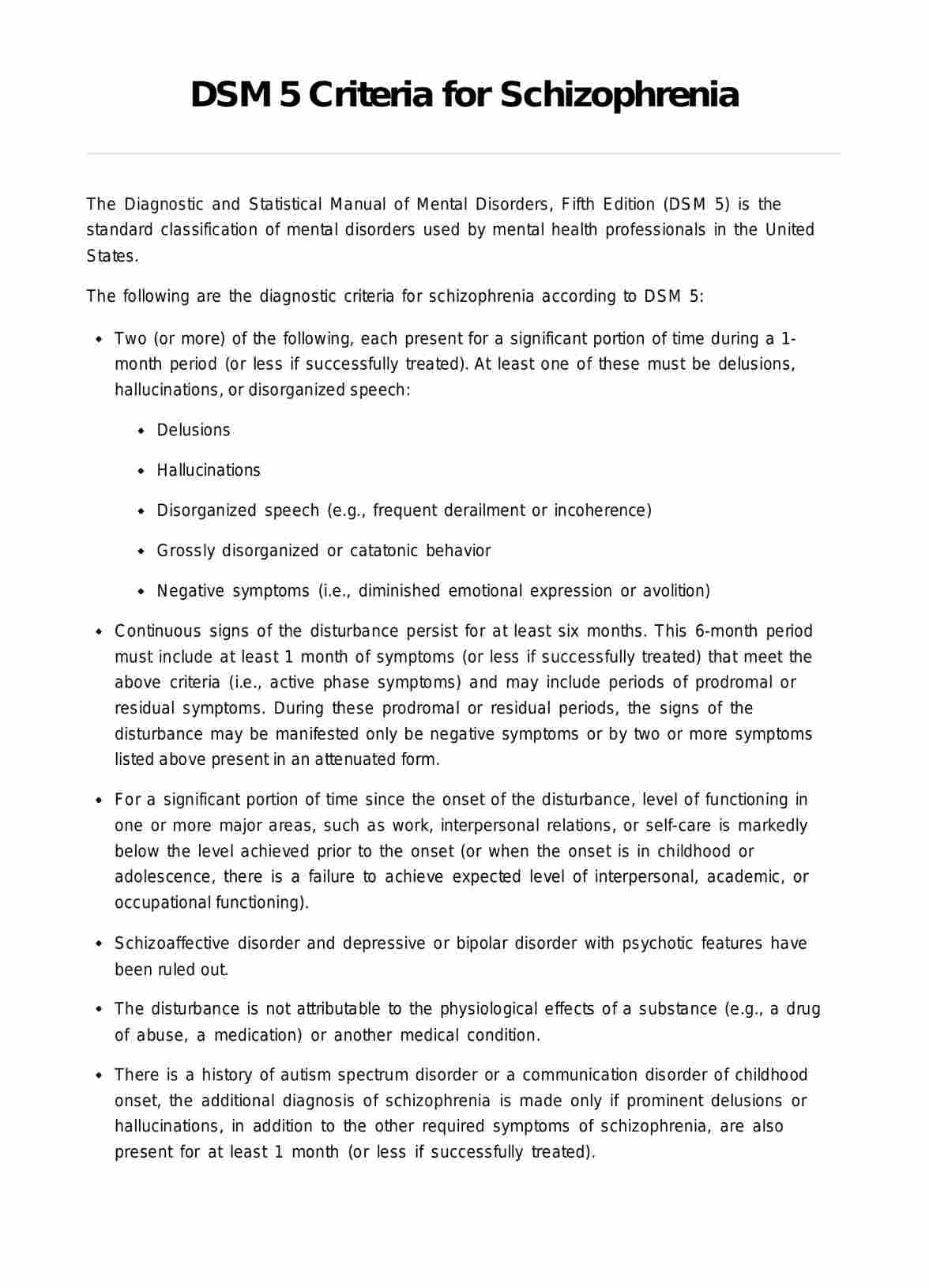
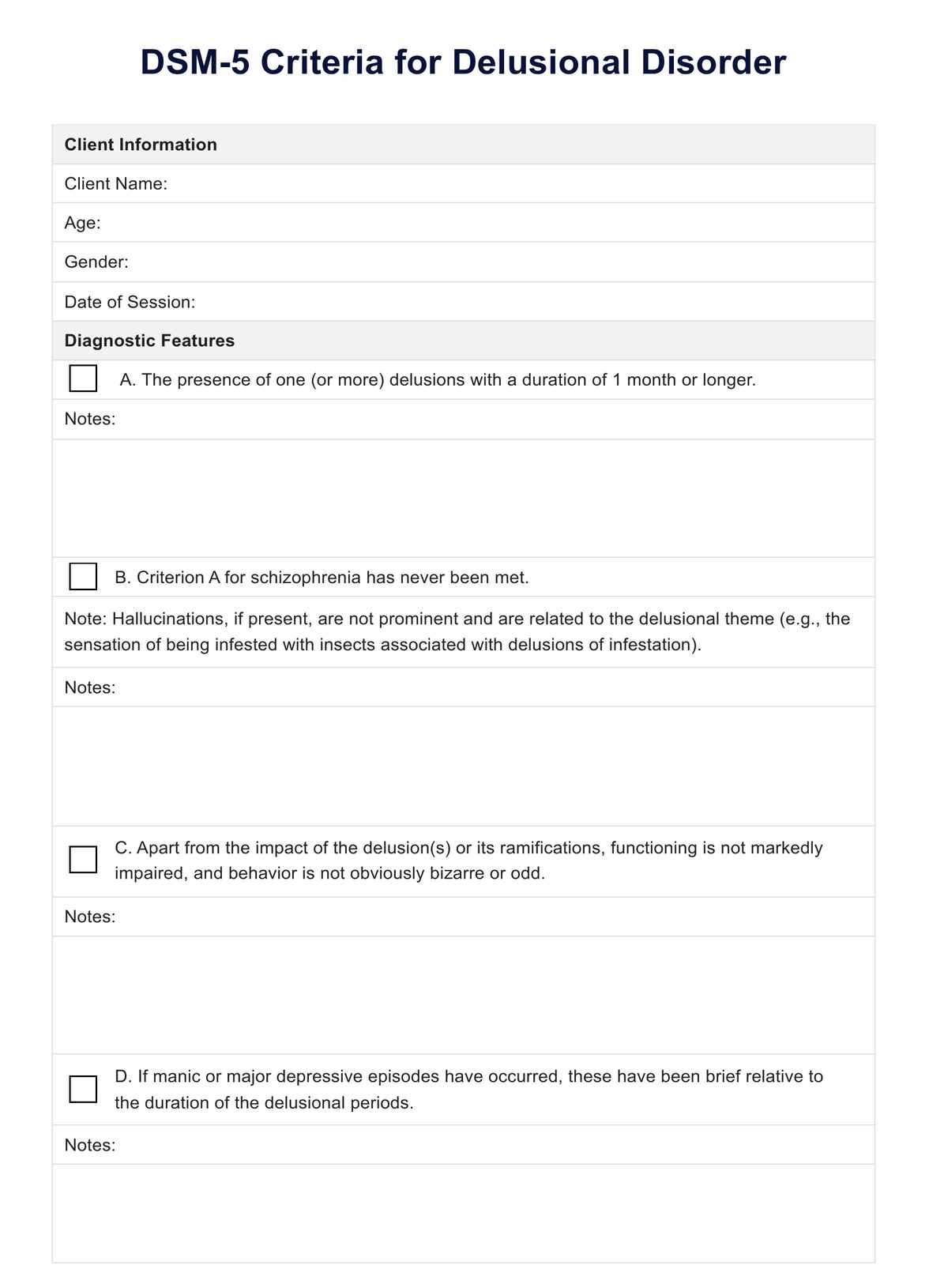
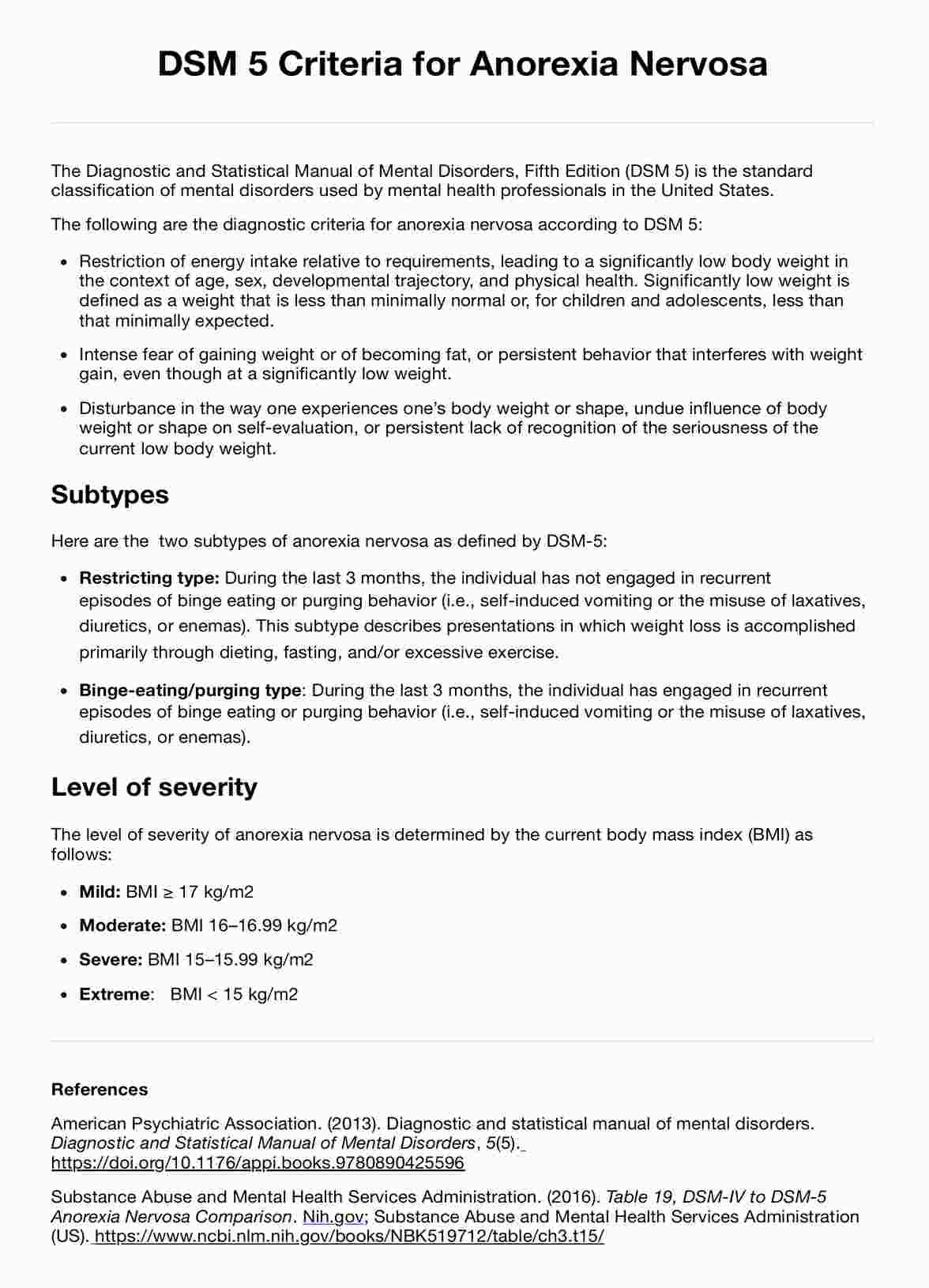
What are the DSM 5 criteria for mood disorders?
The DSM-5 criteria for mood disorders are comprehensive and designed to guide healthcare professionals through diagnostic protocols. Here is a summary of the criteria for some of the key mood disorders, as established by the DSM-5:
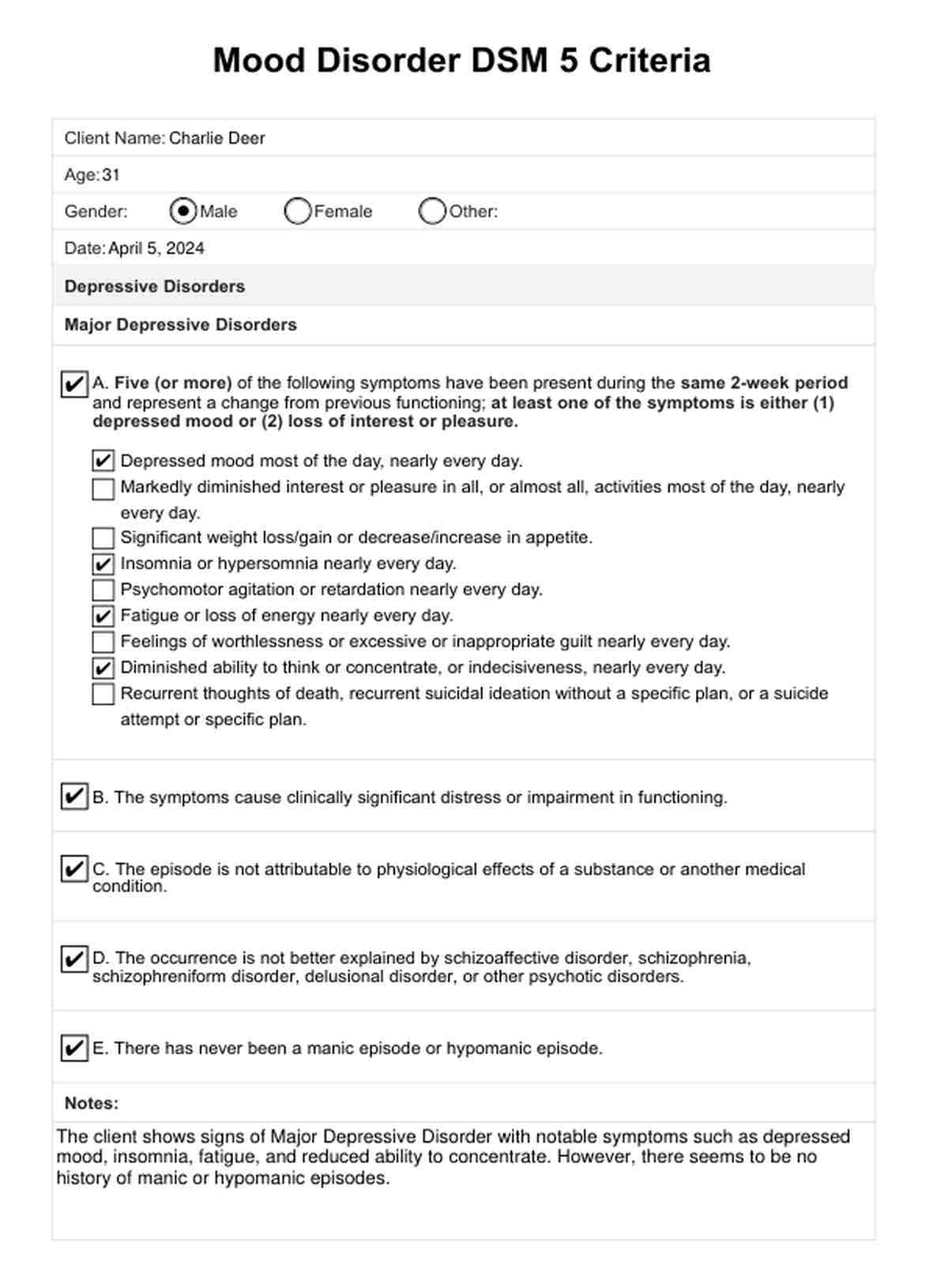
Major depressive disorder
A defining feature of Major Depressive Disorder is the occurrence of one or more major depressive episodes, characterized by at least two weeks of a depressed mood or a loss of interest or pleasure in almost all activities, accompanied by other symptoms including significant weight change, sleep disturbances, or suicidal ideation.
Persistent depressive disorder (dysthymia)
For a diagnosis of Persistent Depressive Disorder, a patient must demonstrate a consistently depressed mood for at least two years (one year for children and adolescents), along with at least two additional depressive symptoms.
Bipolar I disorder
A Bipolar I Disorder diagnosis requires the presentation of one or more manic episodes, which may be preceded by or followed by hypomanic or major depressive episodes. A manic episode entails a distinct episode of abnormally elevated, expansive, or irritable mood and abnormally increased activity or energy, lasting at least one week and present most of the day, nearly every day.
Bipolar II disorder
A diagnosis of Bipolar II disorder necessitates a history of at least one major depressive episode and at least one hypomanic episode without the occurrence of a full manic episode.
How is mood disorder treated?
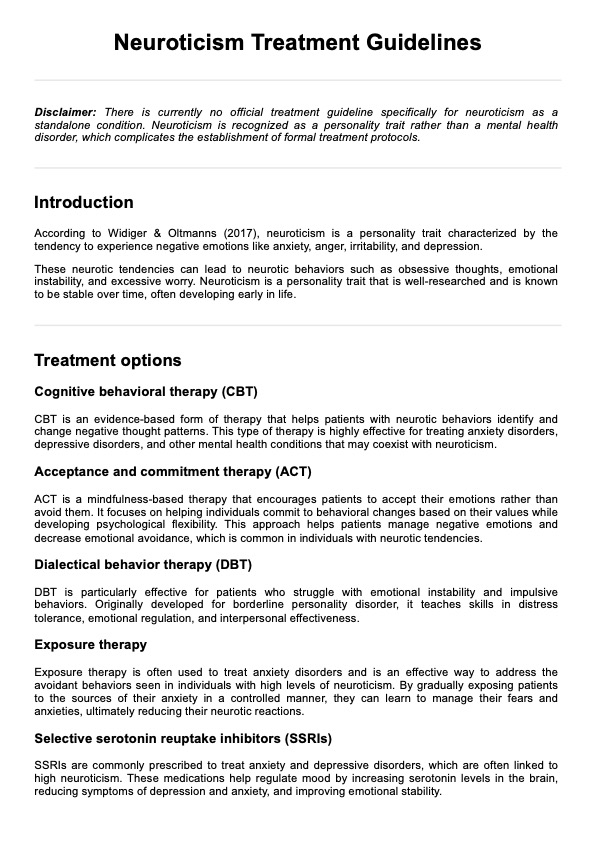
Mood disorders, such as depression and bipolar disorder, can be effectively treated through a combination of various approaches. Here are some common treatment methods:
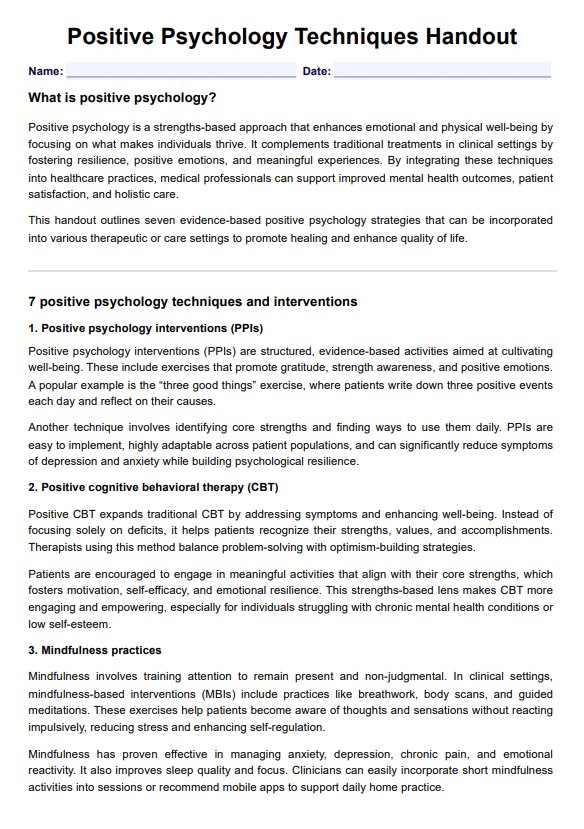
Psychotherapy
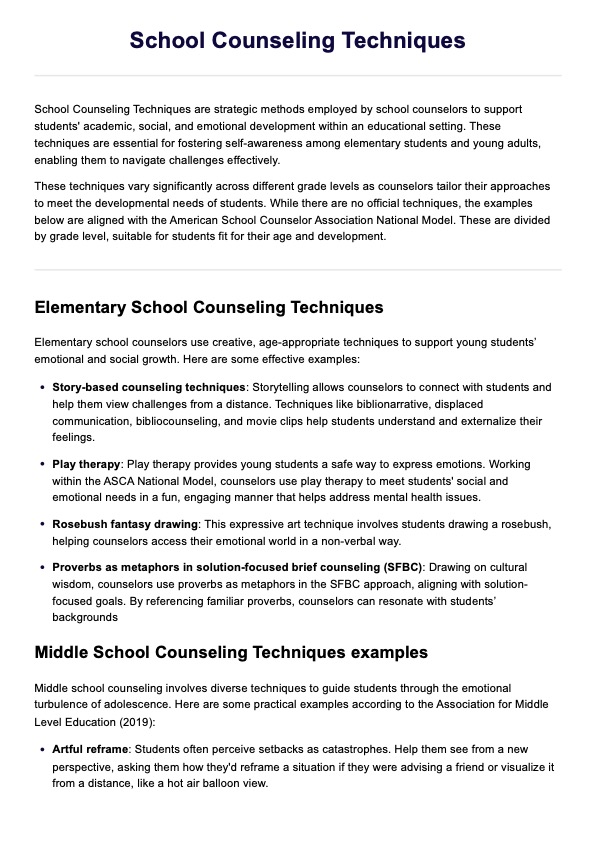
Psychotherapy, also known as talk therapy, is a crucial component in the treatment of mood disorders. It can help individuals understand and manage their thoughts, emotions, and behaviors more effectively. Common types of psychotherapy include:
- Cognitive-behavioral therapy (CBT)
- Interpersonal therapy (IPT)
- Psychodynamic therapy
- Family-focused therapy (FFT)
Pharmacotherapy
Medication can be an effective treatment option for mood disorders, mainly when used in combination with psychotherapy. Several classes of medications are commonly prescribed, including:
- Antidepressants (e.g., selective serotonin reuptake inhibitors [SSRIs], serotonin-norepinephrine reuptake inhibitors [SNRIs])
- Mood stabilizers (e.g., lithium, anticonvulsants)
- Antipsychotics (for bipolar disorder or treatment-resistant depression)
Brain stimulation therapies
In some cases, brain stimulation therapies may be recommended for individuals who do not respond to other treatments. These include:
- Electroconvulsive therapy (ECT)
- Transcranial magnetic stimulation (TMS)
- Deep brain stimulation (DBS)
Lifestyle changes
Incorporating healthy lifestyle changes can also play a crucial role in managing mood disorders. These may include:
- Regular exercise
- Stress management techniques (e.g., mindfulness, meditation)
- Maintaining a balanced diet
- Establishing a consistent sleep routine
Support groups
Participating in support groups can provide individuals with mood disorders a sense of community, support, and shared understanding. These groups can offer valuable coping strategies and a safe space to share experiences.
Reference
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC.
Beck, J. S. (2011). Cognitive behavior therapy: Basics and beyond (2nd ed.). Guilford Press.
Shadrina, M., Bondarenko, E. A., & Slominsky, P. A. (2018). Genetics Factors in Major Depression Disease. Frontiers in psychiatry, 9, 334. https://doi.org/10.3389/fpsyt.2018.00334
Teo, A. R., Choi, H., & Valenstein, M. (2013). Social relationships and depression: ten-year follow-up from a nationally representative study. PloS one, 8(4), e62396. https://doi.org/10.1371/journal.pone.0062396
Commonly asked questions
The causes of mood disorders are believed to be a combination of genetic, biological, environmental, and psychological factors. This can include a family history of mood disorders, brain chemistry imbalances, stressful life events, and chronic health conditions.
While some mood disorders can be managed more effectively than others, most can be substantially improved with proper treatment. This might include medication, psychotherapy, or a combination of both, allowing many individuals to lead normal, productive lives.
Yes, lifestyle changes such as regular physical activity, maintaining a healthy diet, getting enough sleep, and reducing stress can positively impact managing mood disorders. However, lifestyle changes should complement, not replace, professional treatment plans.






-template.jpg)