DSM 5 Criteria for Schizophrenia
Explore the DSM 5 Criteria for Schizophrenia and learn more about the symptoms, diagnosis, and treatment options. Download a free PDF for your reference.


What is schizophrenia?
Schizophrenia is a chronic mental disorder that affects the way a person thinks, feels, and behaves. It is a serious condition that can cause significant impairment in daily functioning and can impact relationships with others.
People with schizophrenia may experience hallucinations, delusions, disorganized thinking and speech, lack of motivation or interest in activities, and difficulty with concentration and memory (Hany et al., 2023). These symptoms can be distressing and can make it challenging to carry out daily tasks. Active and residual periods of the disorder can occur, with varying levels of severity and duration.
Moreover, people with schizophrenia have grossly disorganized or catatonic behavior, which includes extreme excitement or stupor, no responsiveness to surroundings, and disorganized speech and thoughts. This can lead to difficulty in communication with others.
Schizophrenia is a complex disorder that has no single known cause. It is believed that a combination of genetic, environmental, and brain chemistry factors may contribute to the development of schizophrenia.
There is currently no cure for schizophrenia, but it can be managed with a combination of medication, therapy, and support from loved ones. With proper treatment and support, many people with schizophrenia can lead fulfilling lives.
DSM 5 Criteria for Schizophrenia Template
DSM 5 Criteria for Schizophrenia Example
Types of schizophrenia
There are five recognized types of schizophrenia spectrum: paranoid, disorganized, catatonic, undifferentiated, and residual. Specific symptoms and patterns of behavior characterize each type:
Paranoid schizophrenia
Paranoid schizophrenia is the most common type of schizophrenia. People with this type of schizophrenia often experience delusions and hallucinations, but their thoughts and behaviors remain relatively organized.
Disorganized schizophrenia
Disorganized schizophrenia is characterized by disorganized thinking and speech, as well as difficulty with daily tasks. People with this type of schizophrenia may have trouble organizing their thoughts and communicating coherently.
Catatonic schizophrenia
Unusual movements and behaviors characterize catatonic schizophrenia. People with this type of schizophrenia may hold their bodies in strange positions or display repetitive, purposeless movements.
Undifferentiated schizophrenia
Undifferentiated schizophrenia is diagnosed when an individual displays a combination of symptoms from multiple types of schizophrenia. This type of schizophrenia is often used as a placeholder diagnosis until more specific symptoms and patterns emerge.
Residual schizophrenia
Residual schizophrenia refers to individuals who have experienced at least one episode of schizophrenia but currently only have mild symptoms. These symptoms may include disordered thinking, difficulty with concentration, and mild hallucinations.
Causes and symptoms
The exact cause of schizophrenia is unknown, but it's believed to be a combination of genetic, environmental, and neurological factors. Some risk factors for developing schizophrenia include a family history of the disorder, exposure to certain viruses during prenatal development, and drug use during adolescence.
Schizophrenia can have various types of symptoms:
- Psychotic symptoms: These symptoms can manifest as hallucinations, where individuals perceive things that are not real, or delusions, which involve holding onto false beliefs even when presented with contradictory evidence.
- Active phase symptoms: During this phase, individuals may encounter heightened symptoms, including vivid hallucinations where they see, hear, or feel things that are not present, and delusions, which are strong beliefs not based on reality.
- Catatonic behavior negative symptoms: These include lack of motivation and difficulty with daily tasks. It also includes having disorganized or catatonic behavior like lack of response to the environment, repetitive movements, or utterances.
- Negative symptoms: These include a lack of motivation and difficulty with daily tasks. It can also refer to decreased emotions and expressions, making it difficult for individuals to connect with others. Only negative symptoms may be present in some cases, leading to a milder form of schizophrenia.
- Prodromal or residual symptoms: These are milder symptoms that may occur during the disorder's early stages or between acute episodes. They can include difficulty concentrating, changes in sleep patterns, and reduced emotional expression.
Treatment options
Treatment for schizophrenia typically involves a combination of medication, therapy, and support from loved ones. Antipsychotic medications can help alleviate some of the symptoms of schizophrenia, but they may also have side effects such as weight gain and drowsiness.
Therapy, including cognitive-behavioral therapy (CBT), can help individuals with schizophrenia learn coping skills and manage their symptoms. It can also be beneficial for family members to participate in therapy sessions to understand the disorder and learn how to provide support.
Support from loved ones, including a strong social network and stable living environment, can greatly improve the overall well-being of individuals with residual schizophrenia. It's important for loved ones to educate themselves about the disorder and be patient and understanding when supporting their loved ones.
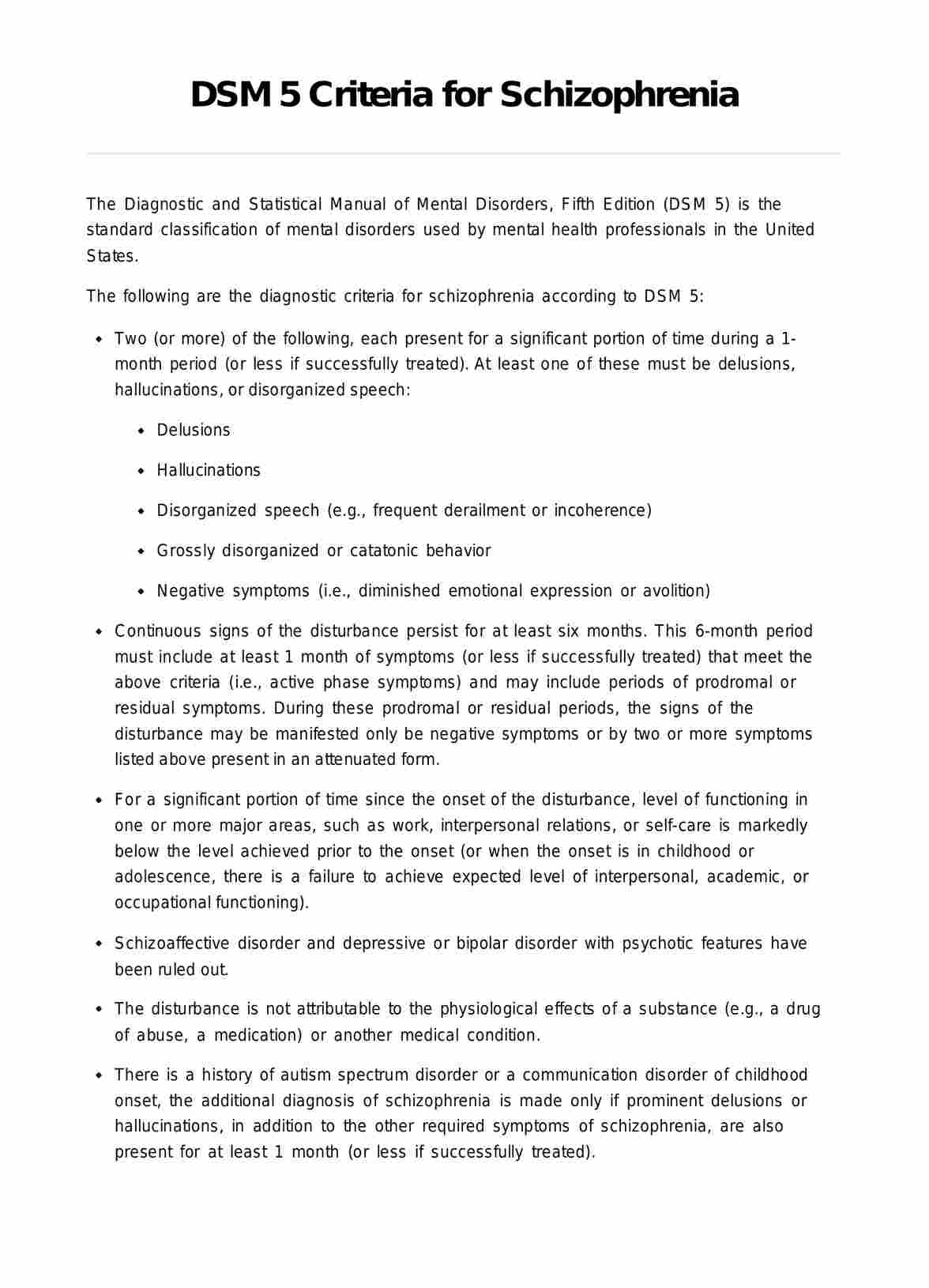
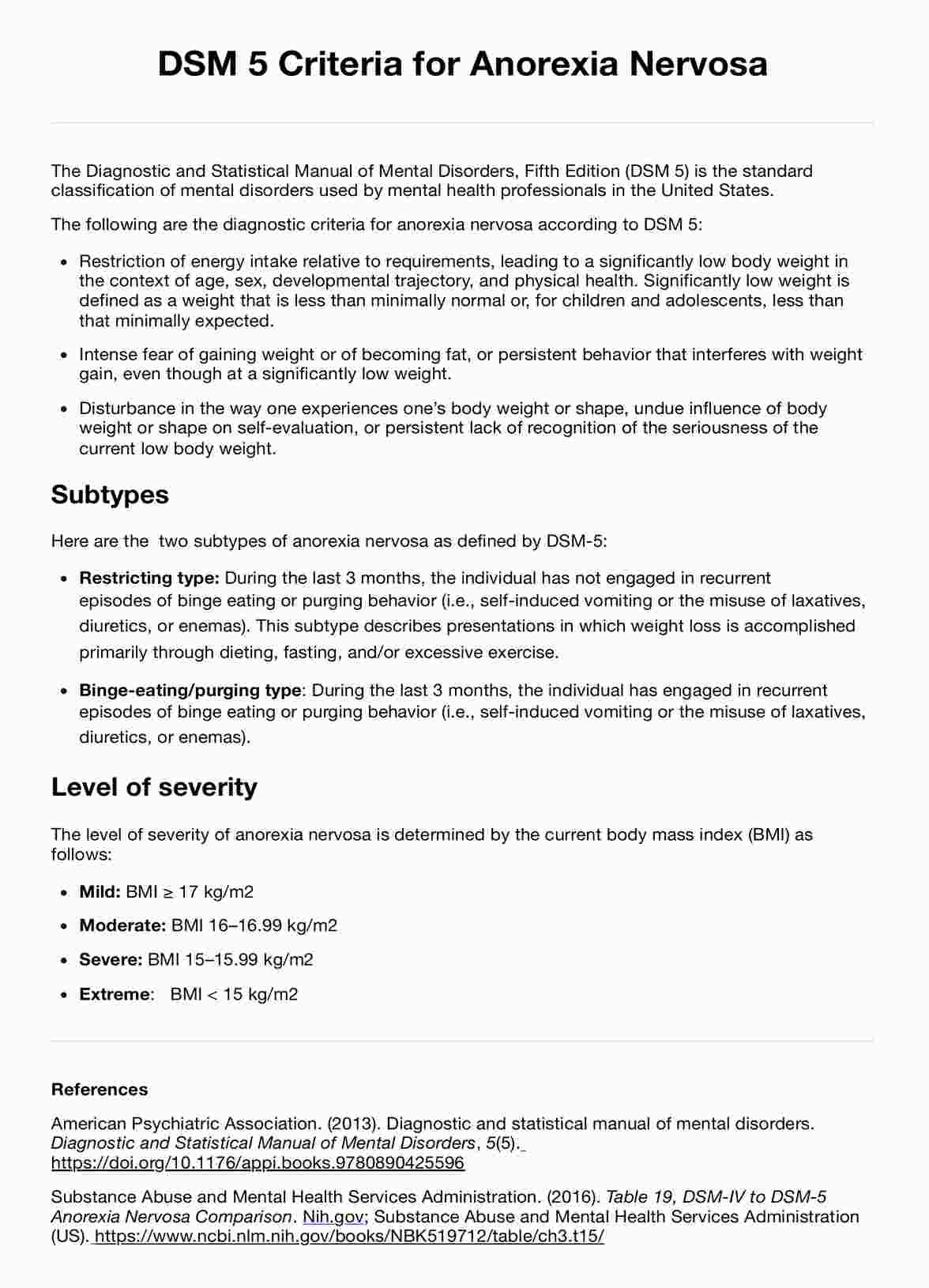
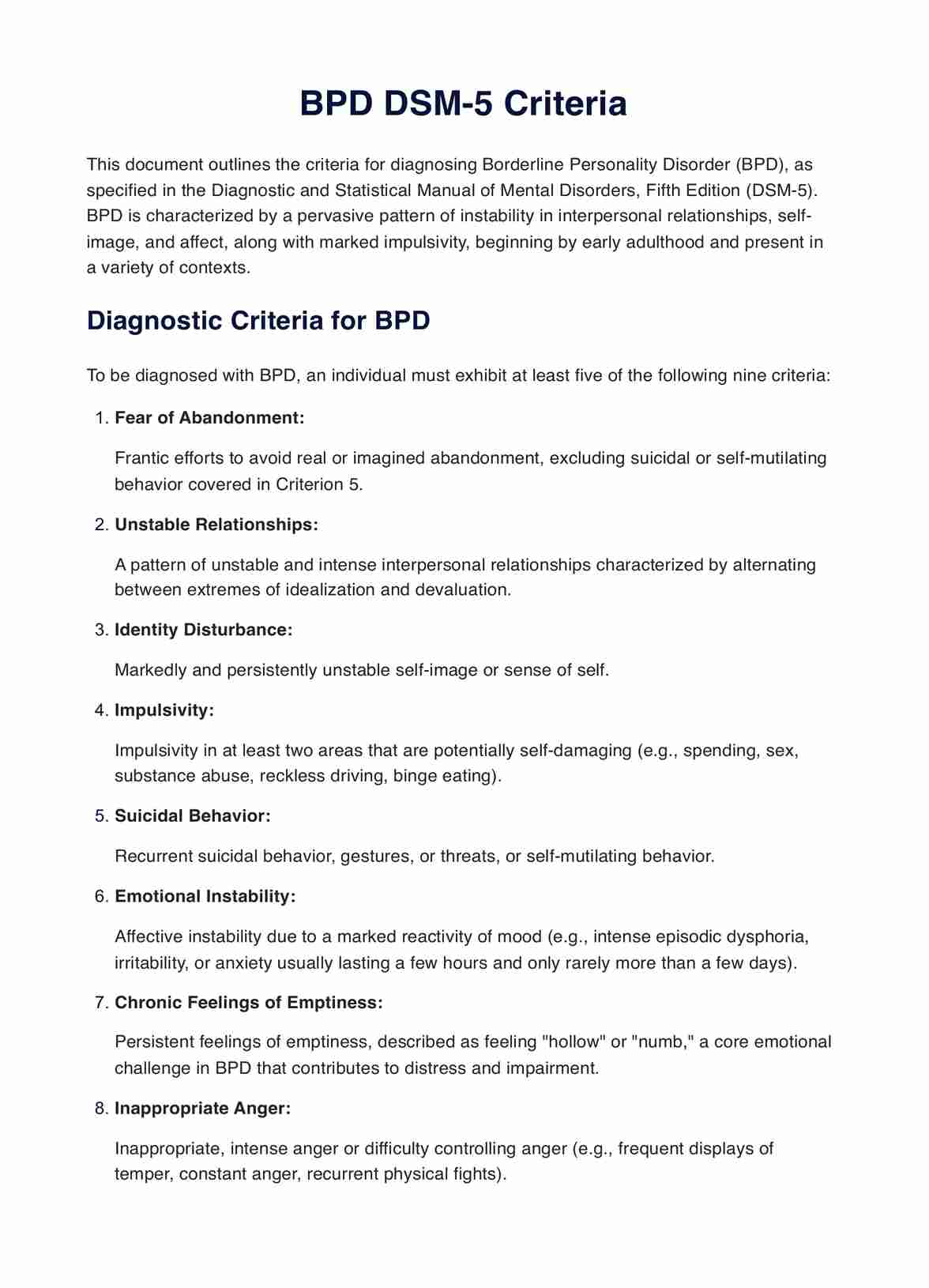
DSM 5 Criteria for Schizophrenia
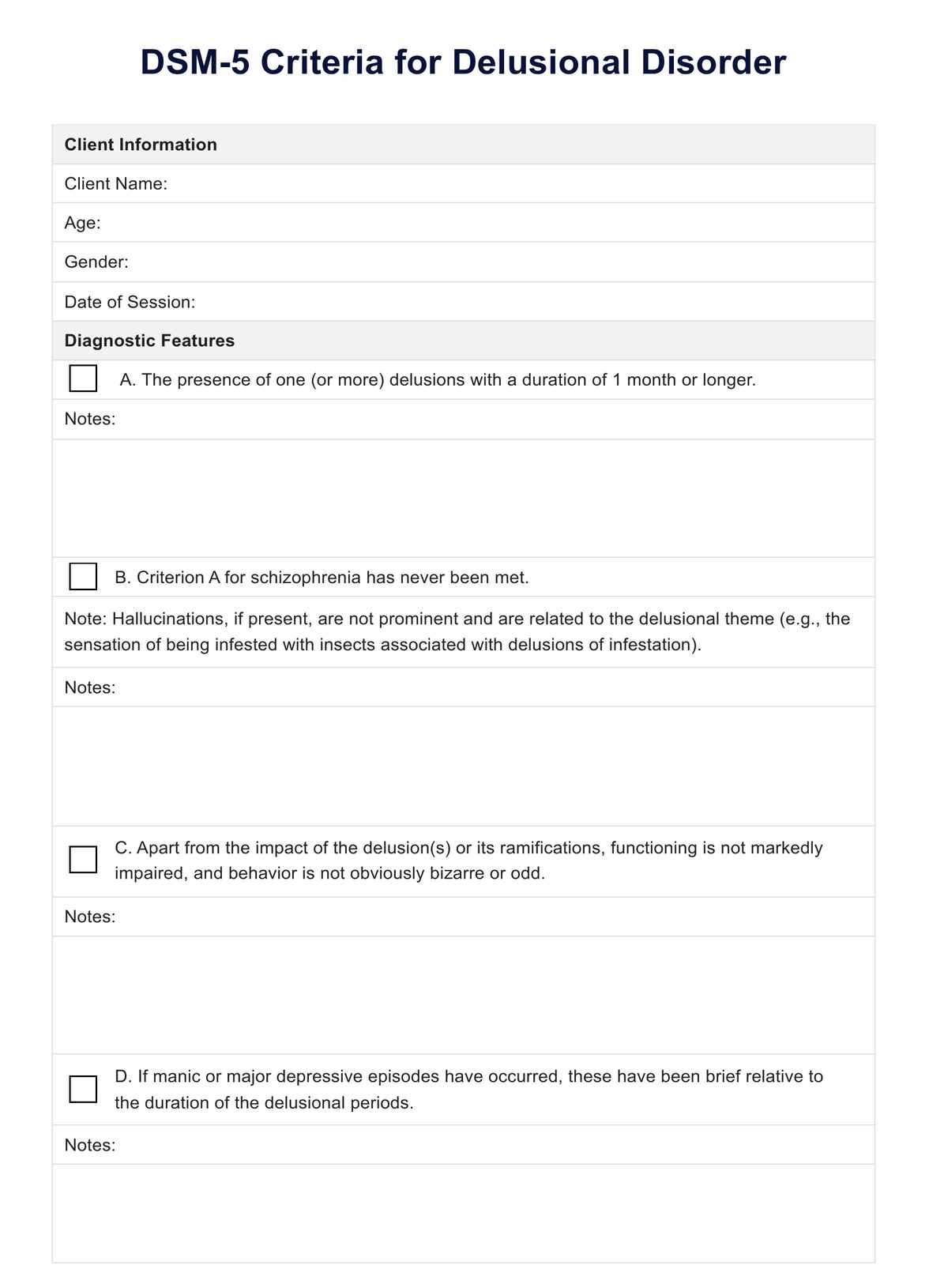
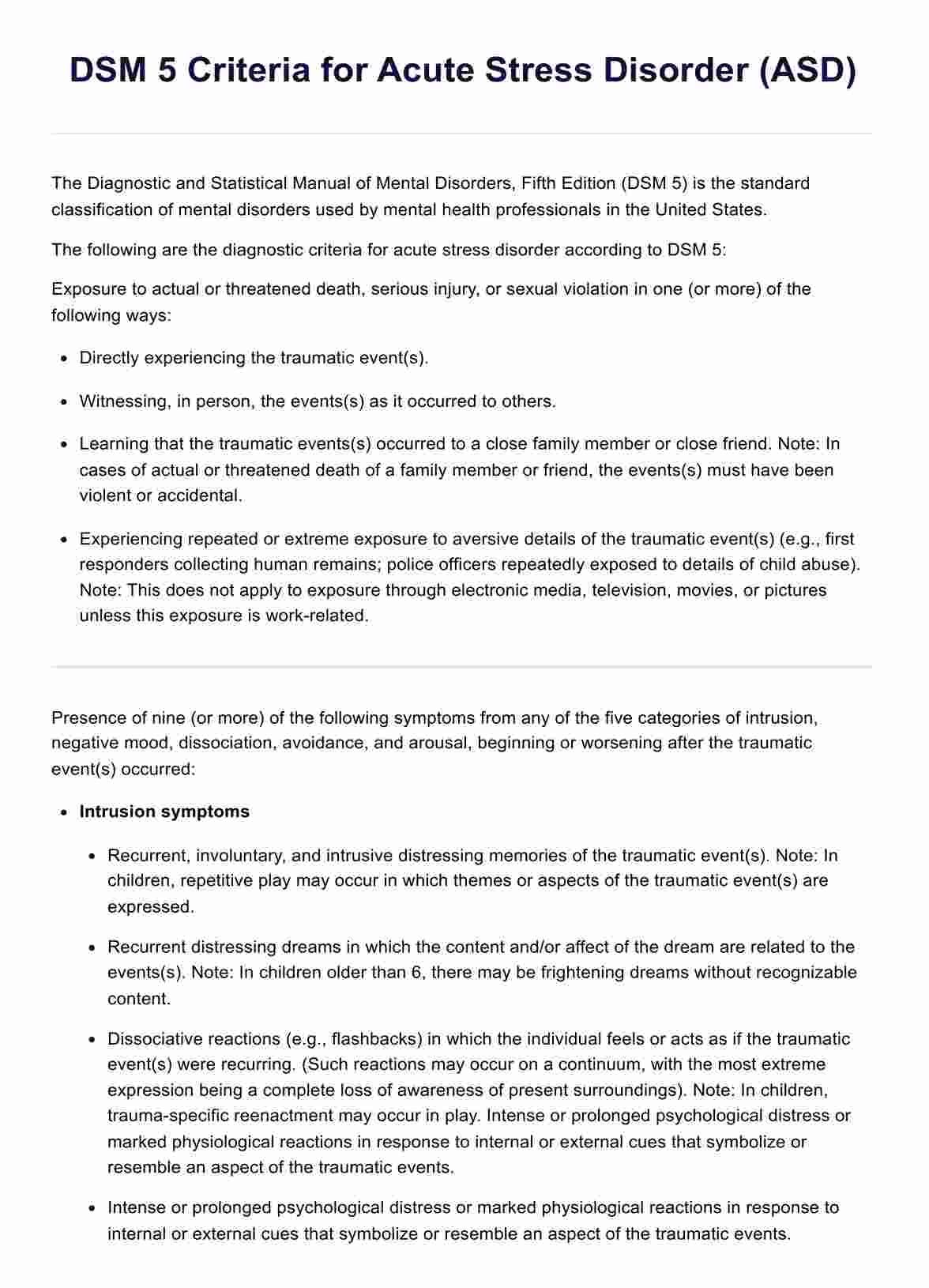
The Diagnostic and Statistical Manual of Mental Disorders (DSM 5) is a crucial publication that serves as a cornerstone for diagnosing various mental health conditions. It offers standardized criteria to assist skilled clinicians in identifying mental disorders during a thorough case formulation assessment.
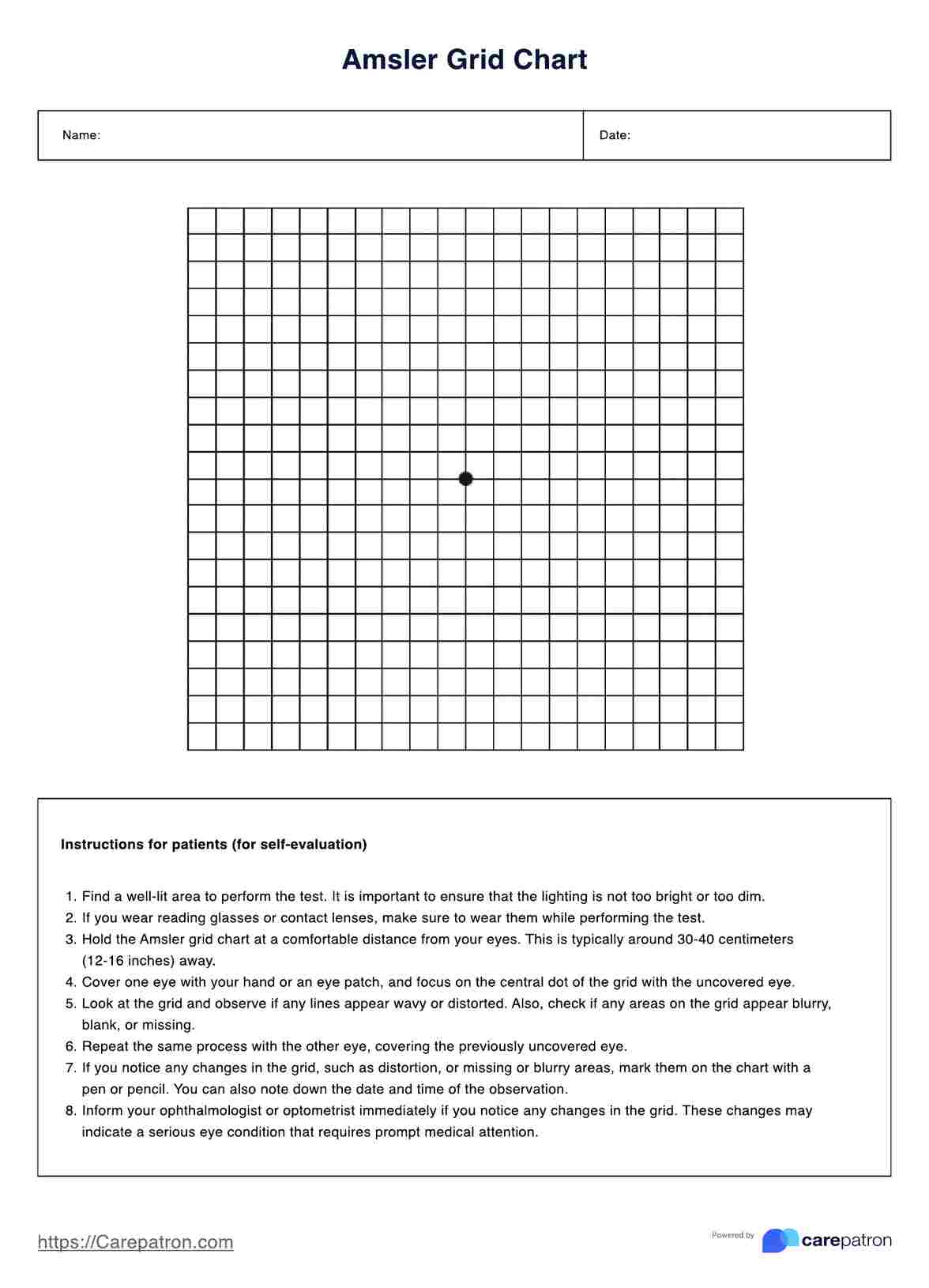
According to the DSM 5, the diagnosis of schizophrenia requires the presence of Two (or more) of the following, each present for a significant portion of time during a 1-month period (or less if successfully treated). At least one of these must be delusions, hallucinations, or disorganized speech:
- Delusions
- Hallucinations
- Disorganized speech (e.g., frequent derailment or incoherence)
- Grossly disorganized or catatonic behavior
- Negative symptoms (i.e., diminished emotional expression or avolition)
Continuous signs of the disturbance persist for at least 6 months. This 6-month period must include at least 1 month of symptoms (or less if successfully treated) that meet the above criteria (i.e., active phase symptoms) and may include periods of prodromal or residual symptoms.
Download our comprehensive template for the full criteria.
Co-occurring disorders
Individuals with schizophrenia may also experience co-occurring mental disorders, such as the following:
Schizoaffective disorder
This disorder, known as schizoaffective disorder, is characterized by a combination of symptoms seen in schizophrenia, like hallucinations and delusions, along with mood disorder symptoms such as depression or bipolar disorder. People with schizoaffective disorder may experience disruptions in their thoughts, emotions, and behavior, impacting their daily lives and relationships.
Post-traumatic stress disorder (PTSD)
Traumatic events, such as accidents, abuse, or natural disasters, have the potential to act as triggers for the onset of schizophrenia in susceptible individuals. This can result in the individual being diagnosed not only with schizophrenia but also PTSD, further complicating their mental health condition.
Psychotic disorder due to another medical condition
In some cases, schizophrenia-like symptoms may be caused by an underlying medical condition, such as a brain tumor or thyroid disorder. This is known as a psychotic disorder due to another medical condition and requires proper medical treatment in addition to therapy for the management of both physical and mental health concerns.
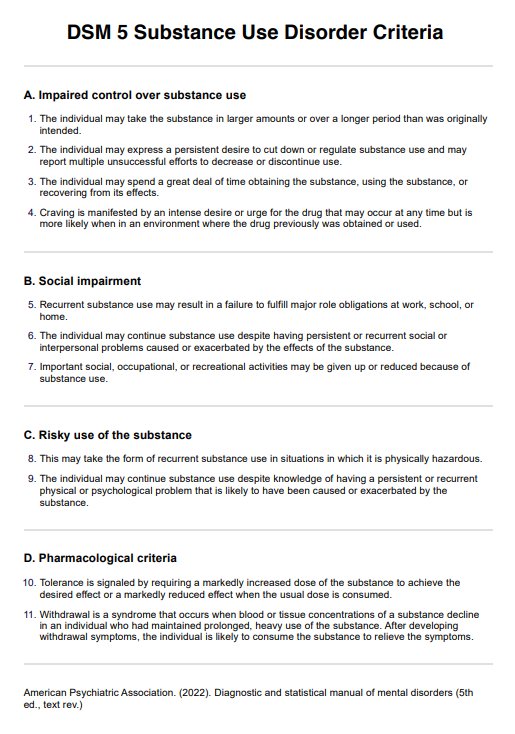
Substance-induced psychotic disorder
Substance use, particularly long-term use of drugs like marijuana and alcohol, can lead to symptoms similar to those seen in schizophrenia. This is known as substance-induced psychotic disorder and requires a comprehensive treatment approach that addresses both the substance use itself and any potential underlying mental health conditions.
Depressive or bipolar disorder with psychotic features
Similar to schizoaffective disorder, some individuals may experience a combination of mood disorder symptoms and schizophrenia-like symptoms. In these cases, the individual may be diagnosed with either depressive or bipolar disorder with psychotic features, depending on the predominant mood disturbance.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders. Diagnostic and Statistical Manual of Mental Disorders, 5(5). https://doi.org/10.1176/appi.books.9780890425596
Hany, M., Rehman, B., Azhar, Y., et al. (2023, March 20). Schizophrenia. In StatPearls. Treasure Island, FL: StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK539864/
Substance Abuse and Mental Health Services Administration. (2016, June). Table 3.22DSM-IV to DSM-5 Schizophrenia Comparison. Nih.gov; Substance Abuse and Mental Health Services Administration (US). https://www.ncbi.nlm.nih.gov/books/NBK519704/table/ch3.t22/
Commonly asked questions
While schizophrenia itself is not a communication disorder, it can significantly affect verbal and non-verbal communication. Some individuals may experience disorganized thinking and speech, which are symptoms of schizophrenia that influence their ability to communicate effectively.
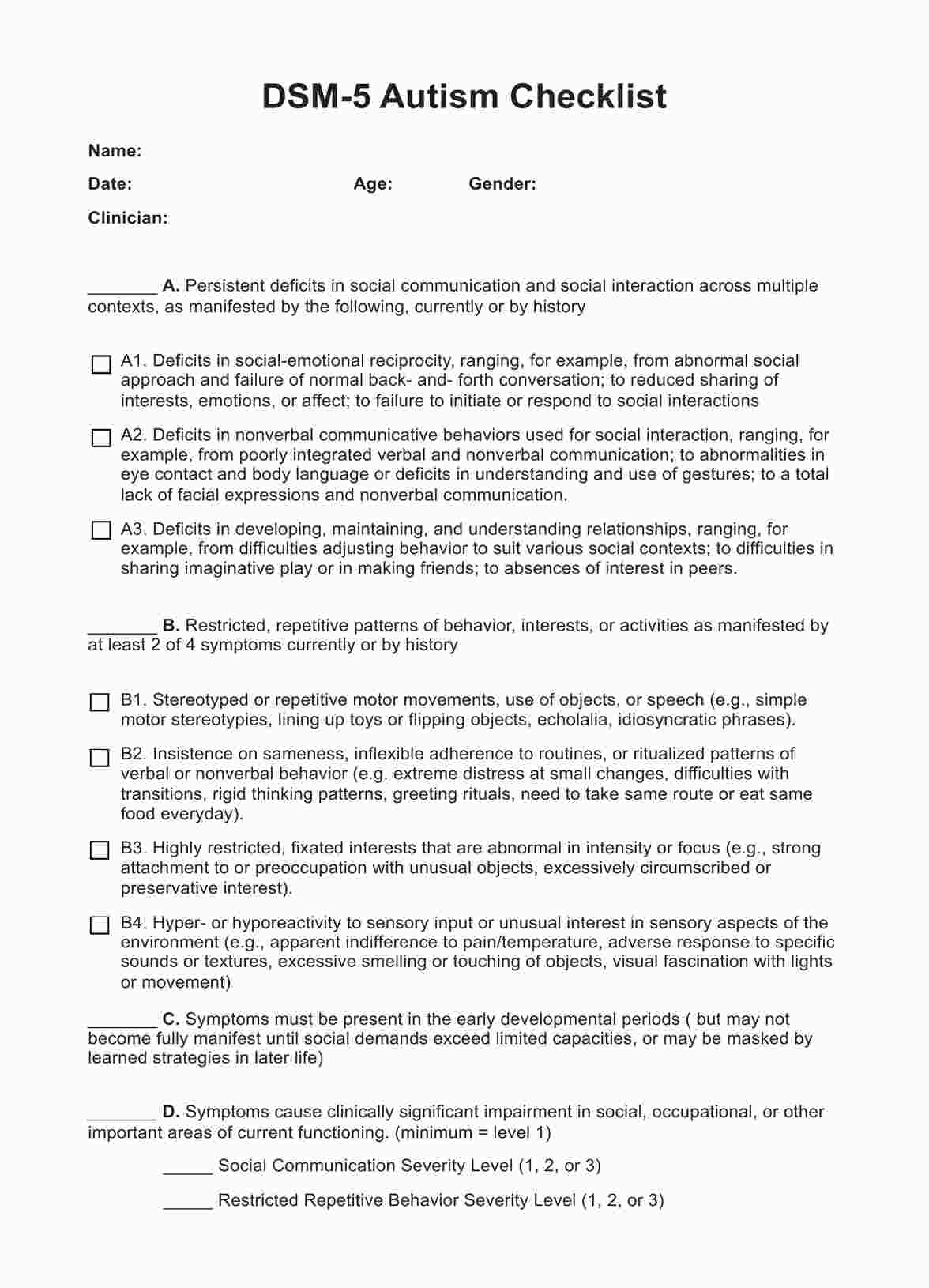
There may be overlaps in the genetic and environmental factors contributing to schizophrenia and autism spectrum disorder (ASD), but they are distinct conditions. However, individuals with ASD may have an increased risk of developing schizophrenia or related psychotic disorders later in life.
Prodromal periods refer to the initial phase before the full onset of schizophrenia, characterized by mild symptoms or changes in behavior. Residual periods occur after acute phases of the illness, where symptoms lessen in intensity but may not disappear entirely, often requiring ongoing management.




















-template.jpg)