DSM 5 Criteria for Delirium
Discover the DSM 5 Criteria for Delirium with our free template. Ideal for mental health professionals seeking a quick reference guide for patient care.


What is delirium?
Delirium is a severe disturbance in mental abilities that results in confused thinking and reduced awareness of the environment. It starts quickly, usually within hours or a few days, and can fluctuate throughout the day. People experiencing delirium can have trouble with attention, memory, orientation, and perception.
This condition can affect anyone but is more common in older adults, particularly those in hospital or long-term care settings.
What causes people to become delirious?
The causes of delirium are numerous, ranging from acute medical or surgical conditions, infections, and medication side effects to substance intoxication or withdrawal. It's often a sign of the body's stress response to an underlying issue rather than a standalone disease. For example, urinary tract infections, which are common in elderly populations, can trigger delirium.
Similarly, medications that affect the brain and nervous system, such as sedatives, can also lead to delirium.
What complications can delirium lead to?
The consequences and adverse effects of delirium are significant. It can lead to a more extended hospital stay, increase the risk of complications, and delay recovery from the underlying cause. Delirium is associated with an increased risk of mortality, particularly in older people.
Complications can include a decline in long-term cognitive function, resembling dementia, increased vulnerability to developing dementia later on, and a higher likelihood of needing long-term care or institutionalization.
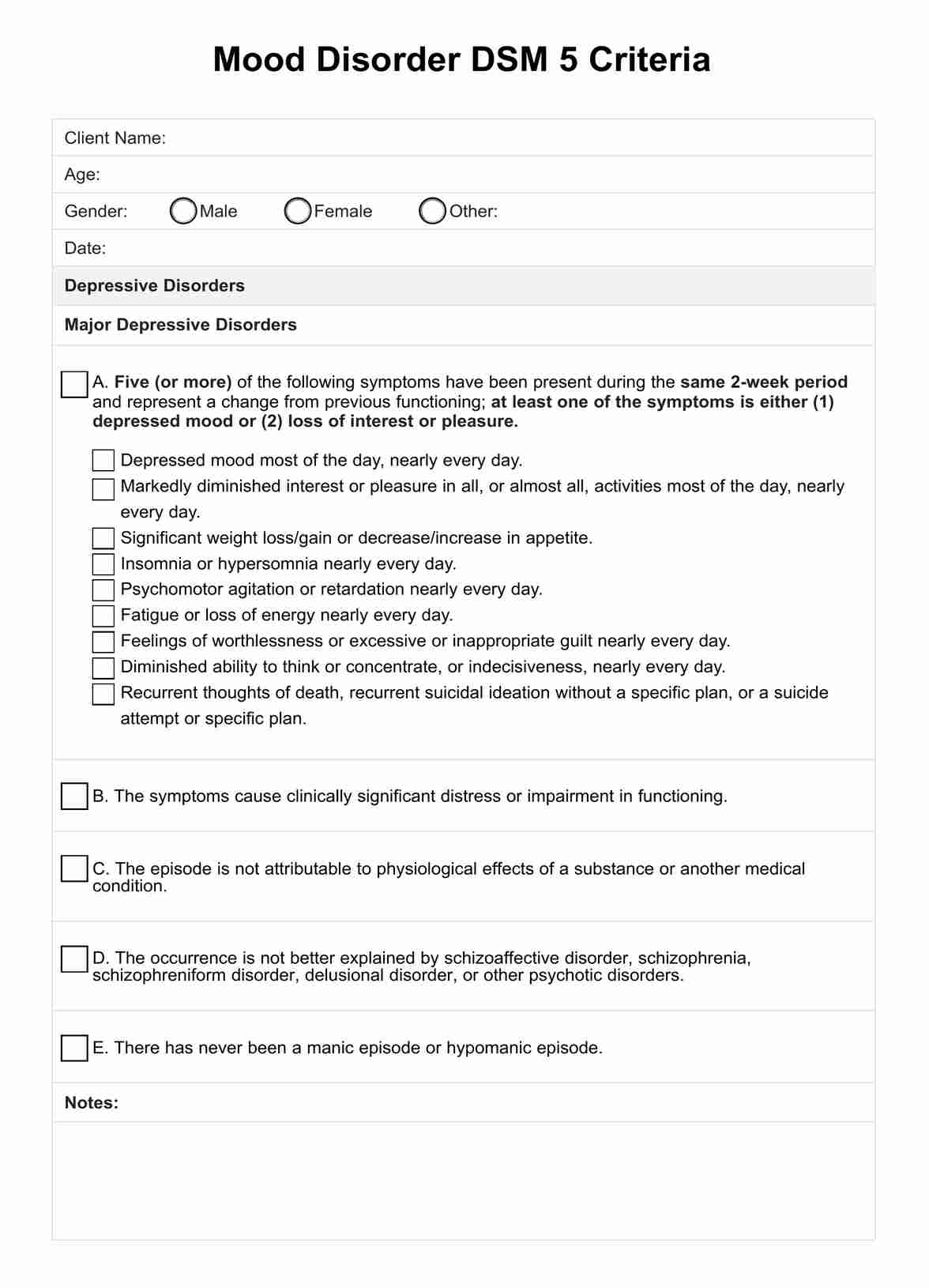
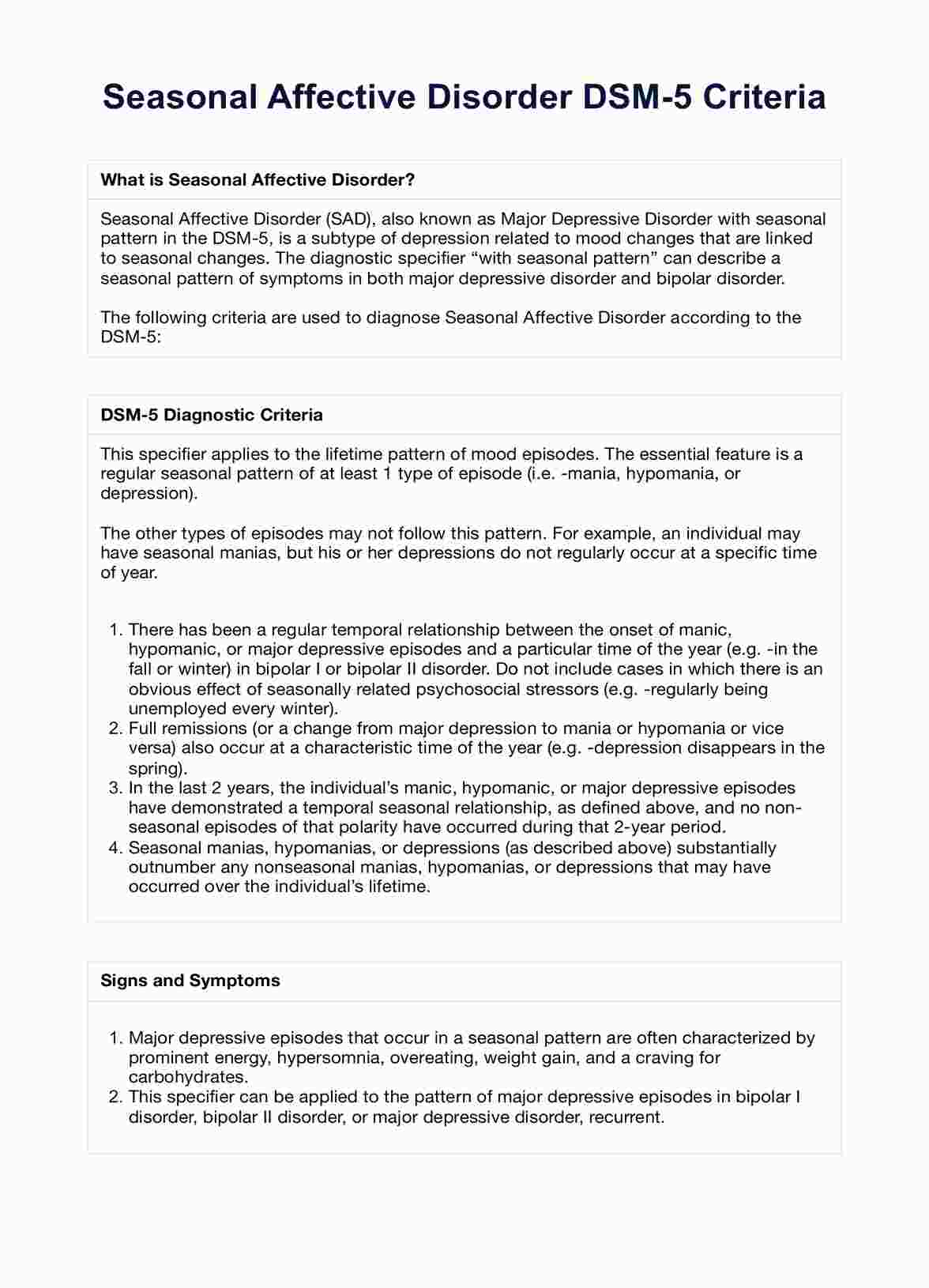
DSM 5 Criteria for Delirium Template
DSM 5 Criteria for Delirium Example
How is delirium diagnosed?
To diagnose delirium, healthcare professionals conduct a thorough evaluation that includes:
- Clinical interview: A detailed interview with the patient, family members, or caregivers to gather information about the onset and progression of symptoms, medical history, and any potential contributing factors such as recent surgeries, infections, or medication changes.
- Physical examination: A comprehensive physical exam to identify any underlying medical conditions causing delirium, including checking for signs of infection, dehydration, or other physical abnormalities.
- Neurological assessment: An evaluation of the patient's neurological status, including tests of attention, memory, orientation, and other cognitive functions.
- Laboratory tests: Blood tests, urine tests, and other laboratory studies to check for infections, electrolyte imbalances, liver and kidney function, and other potential contributors to delirium.
- Imaging studies: In some cases, imaging studies such as a CT scan or MRI of the brain may be performed to rule out other conditions that could cause similar symptoms, such as a stroke or brain tumor.
- Psychiatric evaluation: A psychiatric assessment to differentiate delirium from other mental health conditions like depression, dementia, or psychosis.
By combining information from these assessments, healthcare professionals can determine whether the patient meets the DSM-5 criteria for delirium and develop an appropriate treatment plan.
What is the DSM 5?
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), is a classification system for mental disorders published by the American Psychiatric Association (APA). It is the primary reference for mental health professionals in diagnosing and treating mental health conditions.
The DSM-5 provides standardized criteria and definitions for mental disorders, ensuring consistency and accuracy in diagnosis across different healthcare settings. It covers a wide range of mental health conditions, including mood disorders, anxiety disorders, psychotic disorders, personality disorders, and more.
The manual is regularly updated to reflect the latest research and advancements in mental health. The DSM-5, released in 2013, introduced several significant changes from its predecessor, the DSM-IV, including reclassifying some disorders and adding new ones.
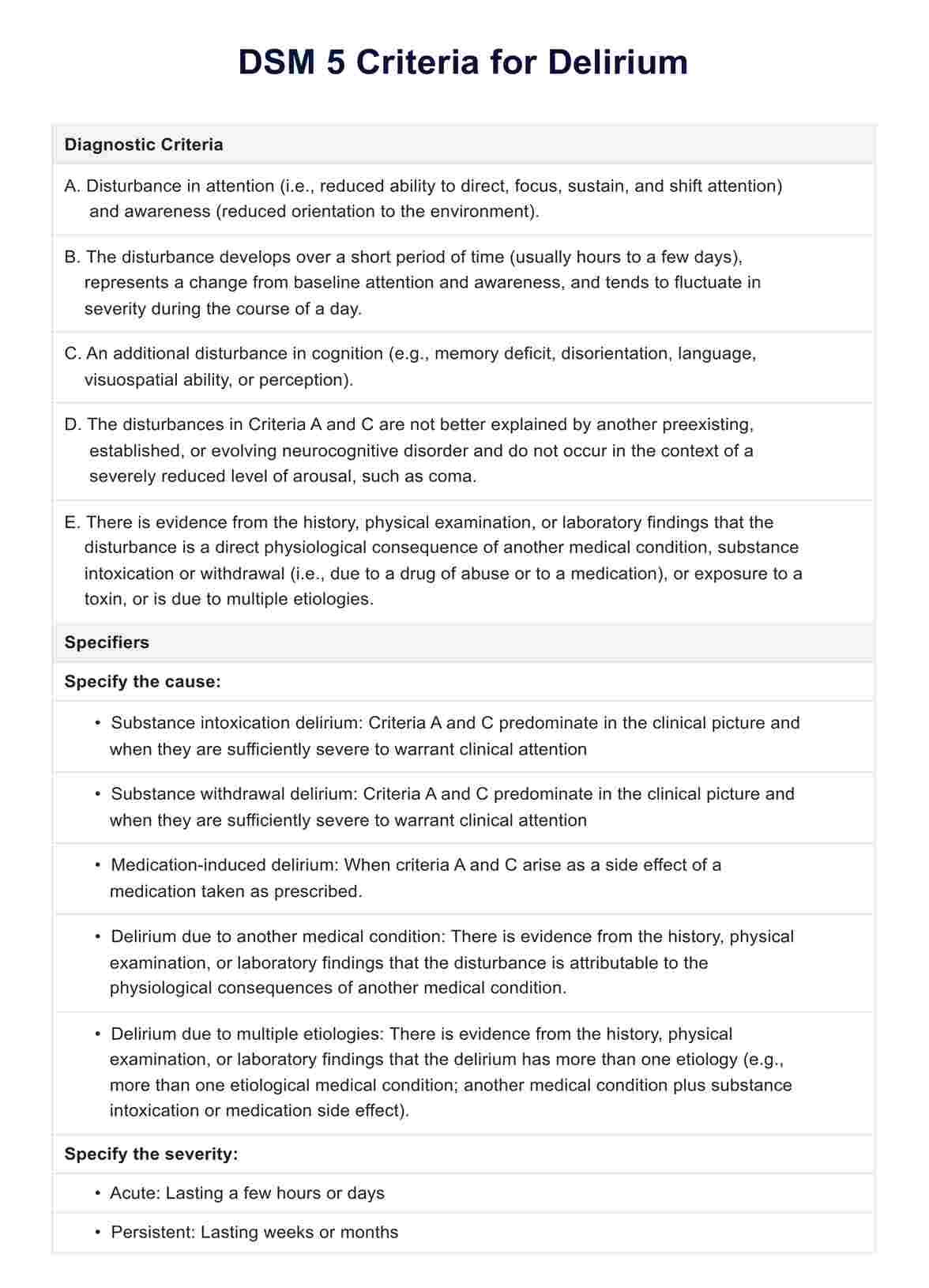
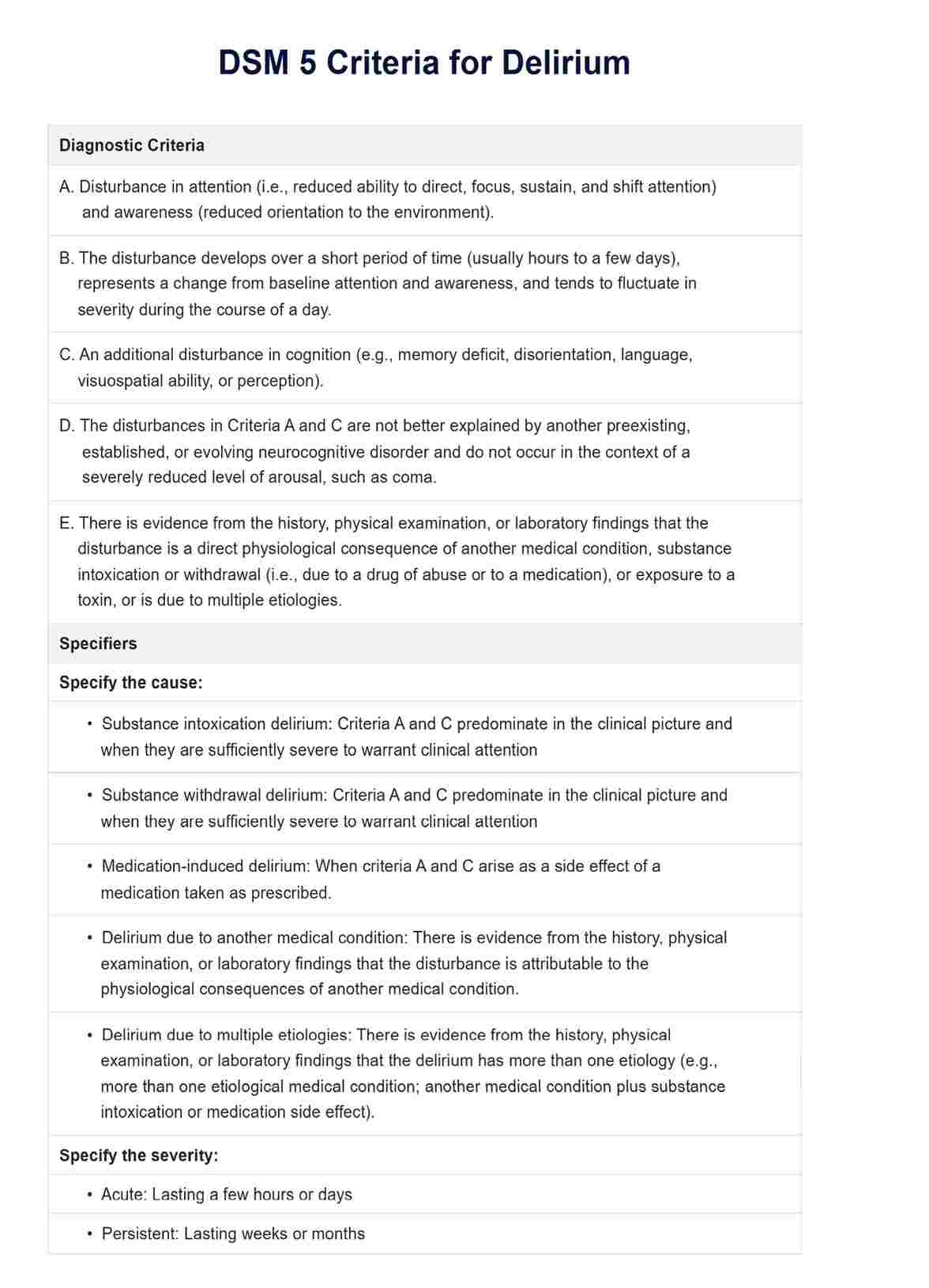
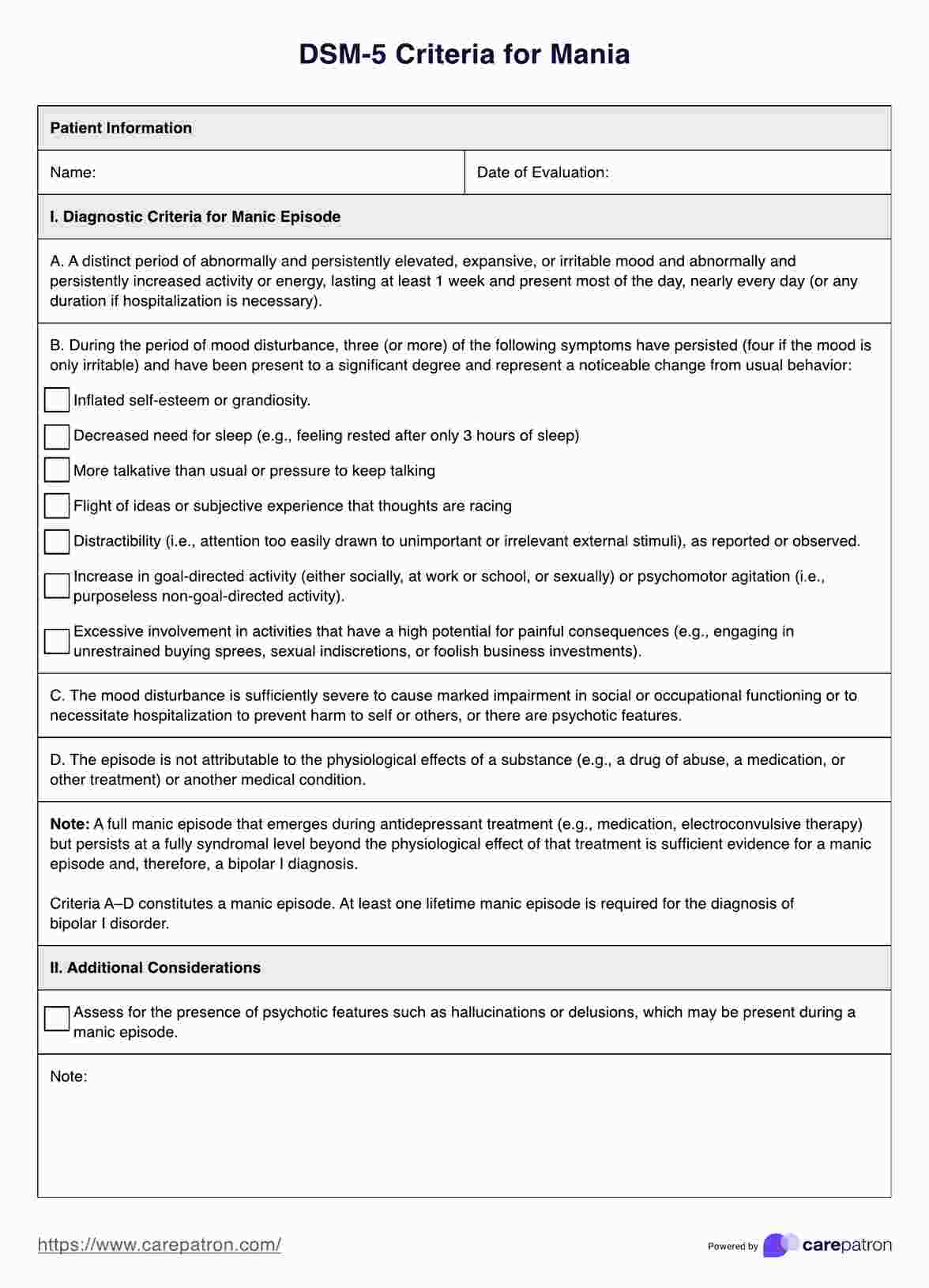
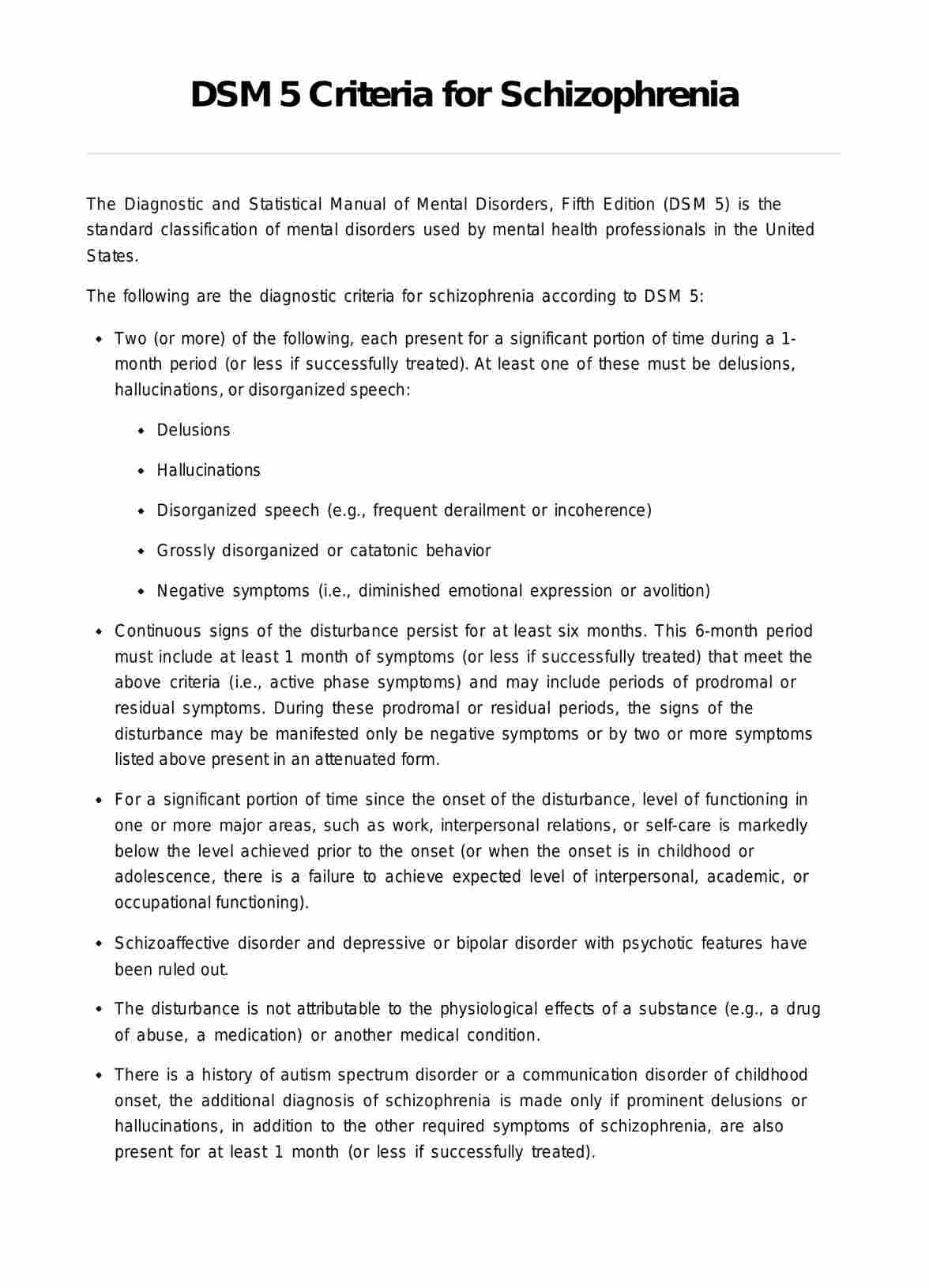
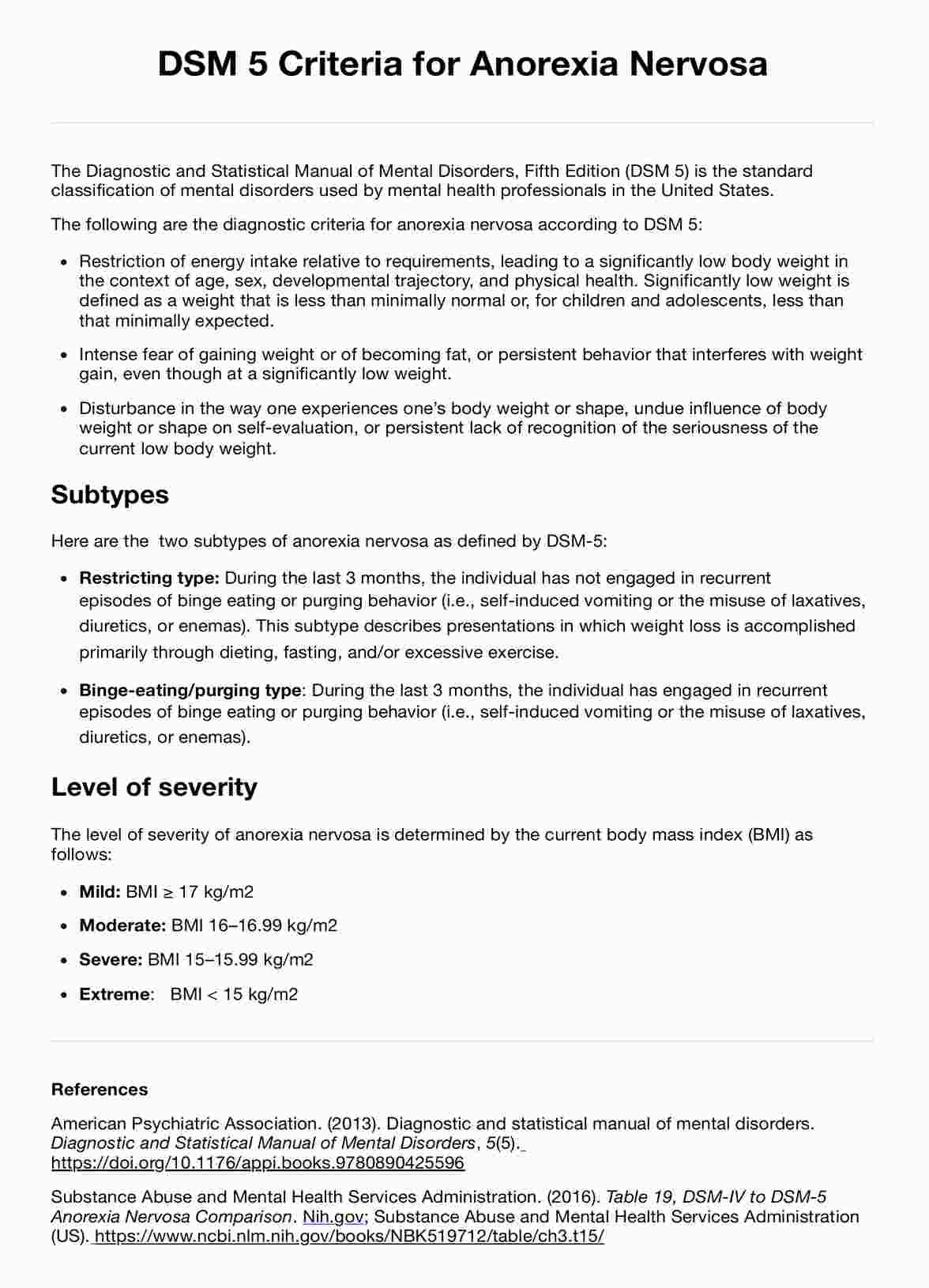
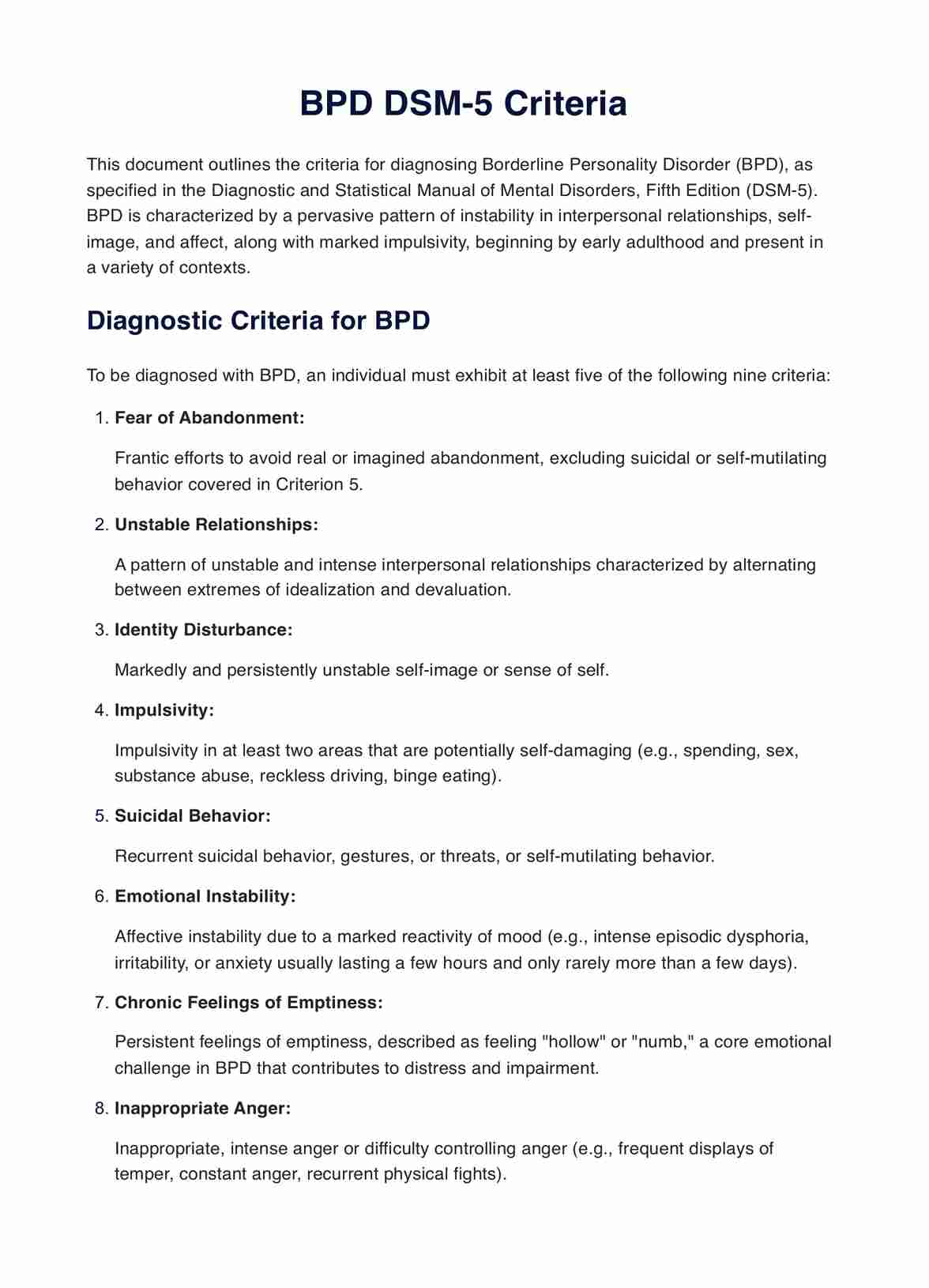
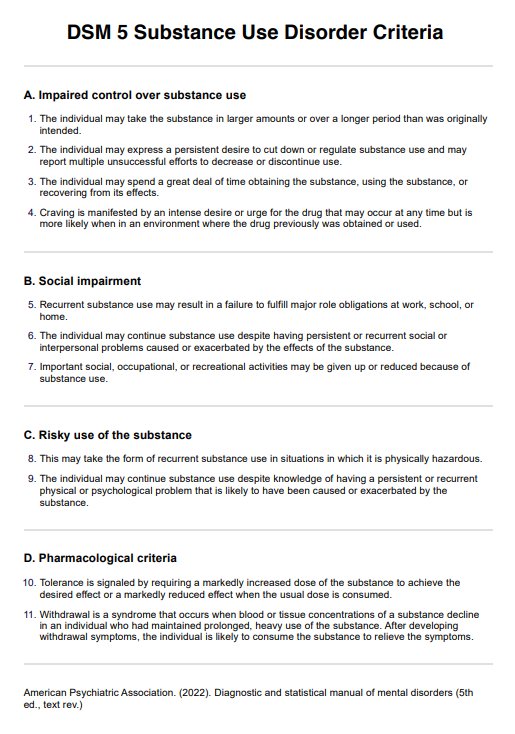
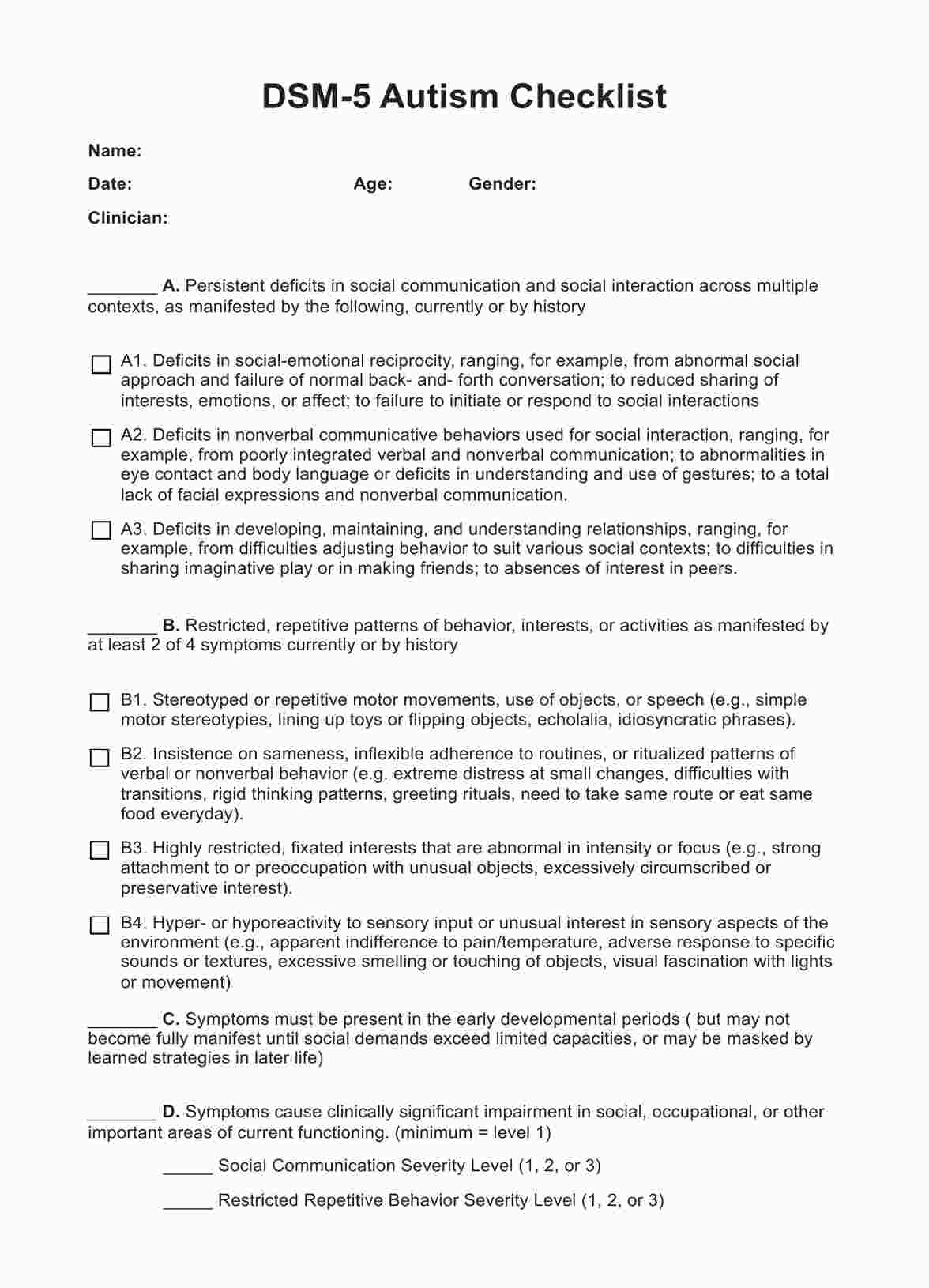
What are the DSM 5 diagnostic criteria for delirium?
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) provides specific criteria for diagnosing delirium. According to the DSM-5, the diagnosis of delirium requires the presence of the following features:
- Disturbance in attention and awareness: There is a reduced ability to direct, focus, sustain, and shift attention. The individual may have difficulty concentrating or become easily distracted.
- Change in cognition: There is a change in another aspect of cognition, such as memory deficit, disorientation, language disturbance, or perceptual disturbance. This change is not better explained by a preexisting, established, or evolving dementia.
- Acute onset and fluctuating course: The disturbance develops over a short period (usually hours to days) and tends to fluctuate in severity during the course of the day.
- Evidence of a causative medical condition: There is evidence from the history, physical examination, or laboratory findings that the disturbance is a direct physiological consequence of another medical condition, substance intoxication or withdrawal (due to medication use or toxin exposure) or multiple etiologies.
Differences between the DSM 4 and DSM 5 delirium criteria
The transition from the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) to the Fifth Edition (DSM-5) brought about some changes in the diagnostic criteria for delirium. Here are the key differences:
- Both DSM-5 and DSM-IV require a disturbance in attention, but DSM-5 also requires reduced awareness of the environment.
- Both versions note the acute onset and fluctuating severity of delirium, but DSM-5 specifically mentions a change from baseline in attention and awareness.
- DSM-5 specifies additional cognitive disturbances, such as memory or language deficits, while DSM-IV focuses on changes in cognition or perceptual disturbances not explained by dementia.
- DSM-5 excludes coma and requires that a pre-existing neurocognitive disorder does not better explain the disturbances, while DSM-IV does not specifically mention coma.
- DSM-5 includes a broader range of potential causes for delirium, including substance intoxication or withdrawal and exposure to toxins, while DSM-IV primarily attributes it to general medical conditions.
These changes were made to improve the accuracy and consistency of diagnosing delirium, ensuring it is clearly distinguished from other conditions with similar presentations, such as dementia or psychiatric disorders.
Research on delirium
Delirium has been the subject of extensive research, with recent studies focusing on improving its identification and management in critical care settings. The insights gained from these investigations hold promise for transforming patient care and reducing the occurrence of delirium in intensive care units (ICUs).
Kotfis et al. (2022) emphasized the need for a future in intensive care where delirium is no longer prevalent. Their study advocates for early identification and management of triggers and drivers of delirium, employing preventive measures and multidimensional interventions. Integrating decision trees and educating healthcare teams aims to heighten awareness and recognition of delirium, ultimately enhancing patient outcomes and creating a delirium-free environment in ICUs.
In another study, Dodsworth et al. (2023) developed and validated an international preoperative risk assessment model for postoperative delirium. This model aids in identifying patients at risk for delirium before surgery, allowing for implementing preventive strategies.
A pioneering AI innovation from Belgium has introduced a novel approach to delirium prevention by combining advanced AI technology with a comprehensive clinical database. This tool automatically calculates an individual's risk of developing delirium, enabling proactive identification and prevention. The utilization of AI technology in this context aims to improve early detection and intervention, potentially enhancing patient outcomes and decreasing the incidence of delirium.
These studies represent significant strides in the ongoing effort to understand and combat delirium. Focusing on prevention, early detection, and effective management, the research paves the way for a future where delirium is no longer a major concern in intensive care settings.
Treatments for delirium
Managing delirium involves a multifaceted approach that addresses the underlying causes, provides supportive care, and employs specific interventions to alleviate symptoms. Here are some key components of delirium treatment:
Identifying and treating the underlying cause
The first step in treating delirium is to identify and address the underlying medical condition, substance intoxication or withdrawal, or exposure to a toxin that may be contributing to the delirium. This may involve adjusting medications, treating infections, managing metabolic imbalances, or addressing other medical issues.
Environmental and supportive measures
Creating a calm, comfortable, and safe environment can help reduce agitation and confusion in patients with delirium. This may include ensuring adequate lighting, minimizing noise, providing orientation cues (such as clocks and calendars), and having familiar objects or people present.
Medications
While there are no specific medications approved for the treatment of delirium, certain medications may be used to manage symptoms such as agitation, hallucinations, or sleep disturbances. These may include antipsychotics, benzodiazepines (for delirium due to alcohol withdrawal), or other sedatives. It's essential to use these medications judiciously, as they can have side effects and may worsen delirium in some cases.
Non-pharmacological interventions
Strategies such as reorientation techniques, cognitive stimulation, and reality orientation can help manage delirium. Engaging patients in simple, structured activities and providing reassurance and support can also be beneficial.
Prevention
Implementing preventive measures, especially in high-risk settings like hospitals and ICUs, is crucial. This may involve regular monitoring for early signs of delirium, avoiding unnecessary medications, ensuring proper hydration and nutrition, and promoting good sleep hygiene.
Early detection and appropriate management of delirium are essential to prevent complications and improve outcomes. A multidisciplinary approach involving physicians, nurses, therapists, and family members is often required to effectively address the complex needs of patients with delirium.
References
BMC Medicine. (n.d.). Table 1 A comparison of DSM-IV and DSM-5 criteria for delirium. BMC Medicine. Retrieved March 13, 2024, from https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-014-0164-8/tables/1
Dodsworth, B. T., Reeve, K., Falco, L., Hueting, T., Sadeghirad, B., Mbuagbaw, L., Goettel, N., & Gelsomino, N. S. (2023). Development and validation of an international preoperative risk assessment model for postoperative delirium. Age and Ageing, 52(6). https://doi.org/10.1093/ageing/afad086
European Delirium Association and American Delirium Society. (2014). The DSM-5 criteria, level of arousal and delirium diagnosis: Inclusiveness is safer. BMC Medicine, 12(1). https://doi.org/10.1186/s12916-014-0141-2
Kotfis, K., van Diem-Zaal, I., Roberson, S. W., Sietnicki, M., van den Boogaard, M., Shehabi, Y., & Ely, E. W. (2022). The future of intensive care: delirium should no longer be an issue. Critical Care, 26(1). https://doi.org/10.1186/s13054-022-04077-y
MacLullich, A. M., Shenkin, S. D., Goodacre, S., Godfrey, M., Hanley, J., Stíobhairt, A., Lavender, E., Boyd, J., Stephen, J., Weir, C., MacRaild, A., Steven, J., Black, P., Diernberger, K., Hall, P., Tieges, Z., Fox, C., Anand, A., Young, J., & Siddiqi, N. (2019). The 4 ‘A’s test for detecting delirium in acute medical patients: A diagnostic accuracy study. In PubMed. NIHR Journals Library. https://www.ncbi.nlm.nih.gov/books/NBK544926/
Commonly asked questions
Delirium can often be cured by treating the underlying cause and managing symptoms, but early detection and intervention are crucial for successful outcomes.
The DSM-5 criteria for delirium include a disturbance in attention and awareness, a change from baseline cognitive function, and evidence that the disturbance is a direct physiological consequence of another medical condition or substance use.
The DSM-5 delirium criteria emphasize the importance of inattention and reduced awareness of the environment, and they provide a broader list of etiological types compared to DSM-4.





















-template.jpg)





















































































