Agoraphobia DSM 5 Criteria
Explore a helpful documentation tool to help screen for the symptoms of agoraphobia among clients. Download a free PDF resource here.


What is agoraphobia?
Agoraphobia is a complex anxiety disorder that significantly impacts individuals and their ability to navigate various spaces. At its core, it is characterized by marked distress as shown in intense fear, anxiety, or avoidance of being in situations where escape might be intricate, or help wouldn't be available if things go wrong. These symptoms occur in places or situations that might induce panic and feel trapped, helpless, or embarrassed.
People with agoraphobia might feel unsafe in an open space, in a crowd, or when outside of their home alone. This fear or anxiety is disproportionate to the actual danger these situations pose. It's not just about preferring the comfort of home; it's an overwhelming, persistent dread that can confine them, limiting their life experiences and interactions. The disorder can vary in severity, from mild, where individuals avoid certain situations, to severe, where they may feel unable to leave their homes (Barlow et al., 2018).
Studies have found that agoraphobia is a common consequence of panic disorder but can also develop independently, affecting about 2% of the population annually and being more prevalent in women. Agoraphobia also often emerges in adolescence or young adulthood, with fears related to safety and physical limitations being common triggers (Roest et al., 2019).
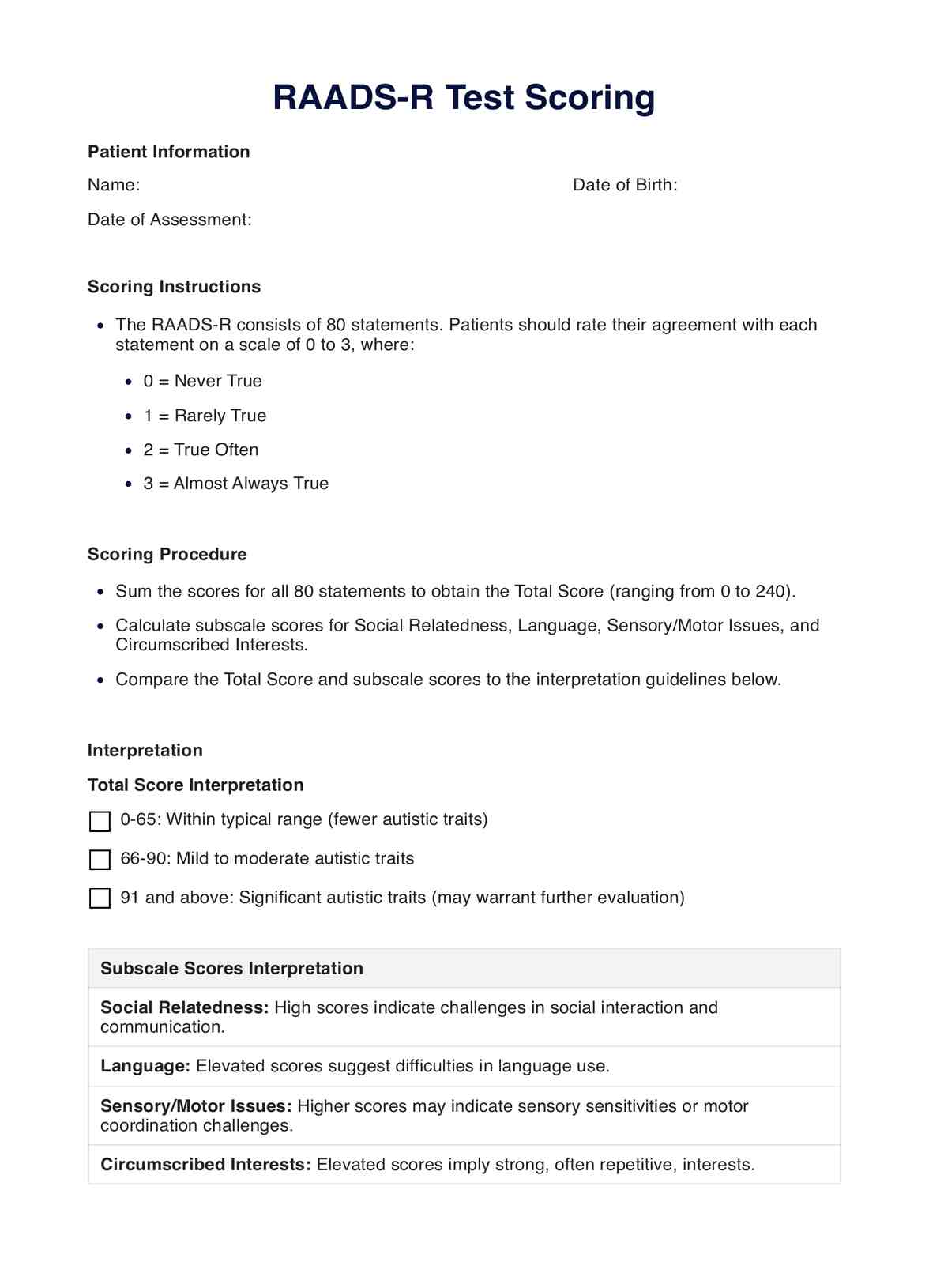
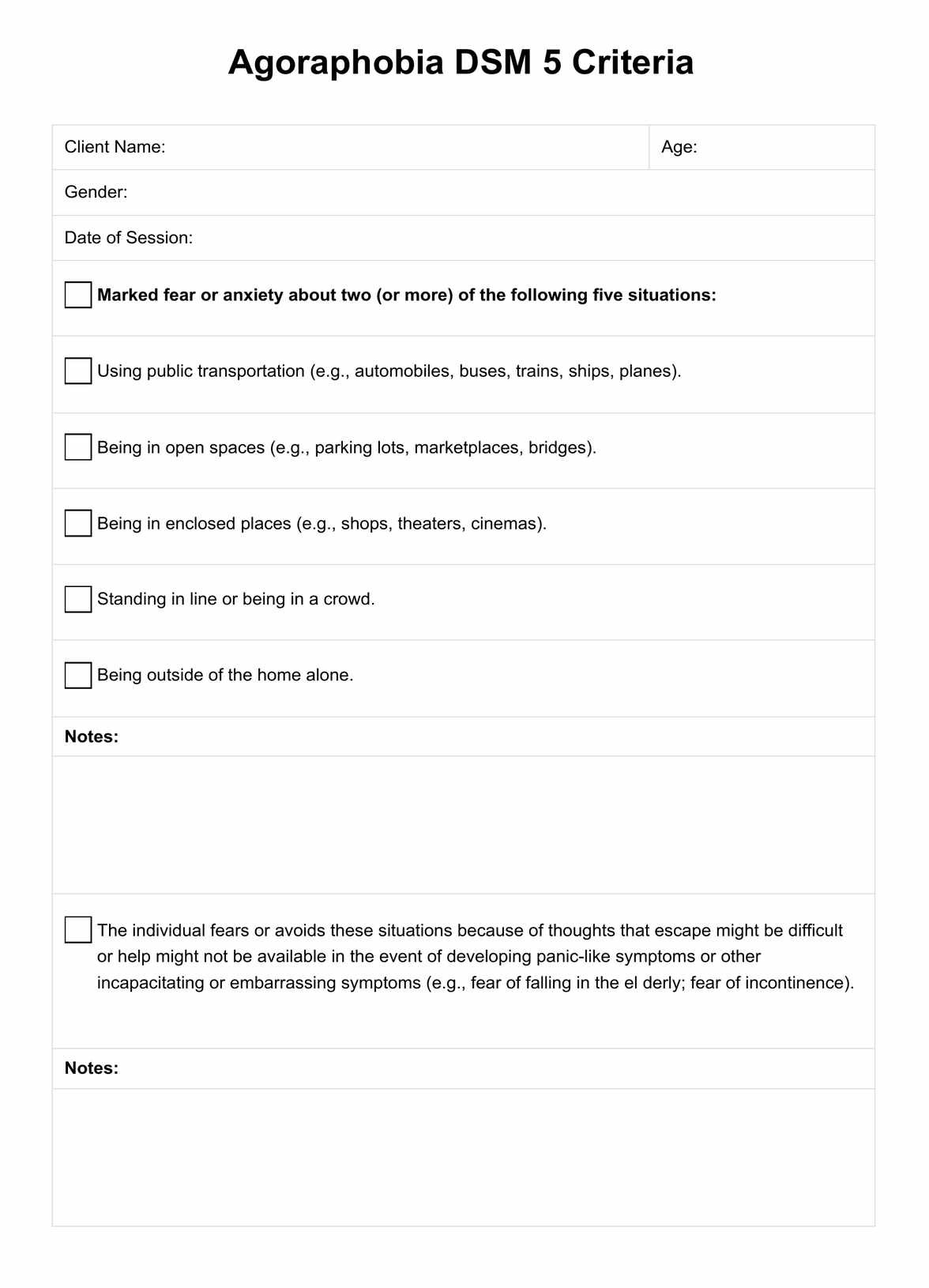
Agoraphobia DSM 5 Criteria Template
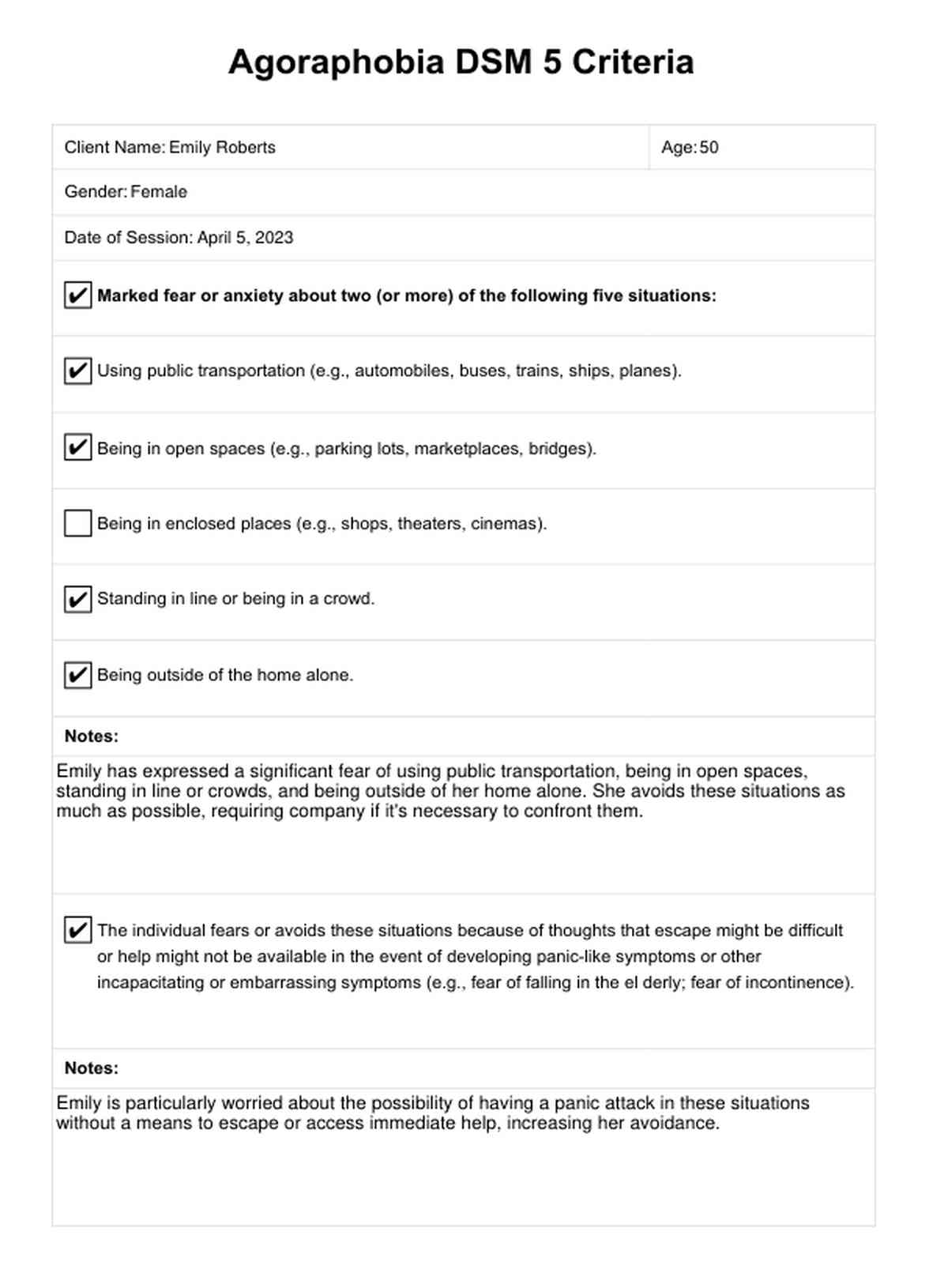
Agoraphobia DSM 5 Criteria Example
Symptoms and causes of agoraphobia
Agoraphobia manifests through a variety of symptoms that go beyond simple fears, resonating deeply in the individual's everyday functioning. The presentation of the following symptoms could need further exploration:
- Intense fear: Individuals experience disproportionate fear when facing specific situations, especially where escape may be challenging.
- Avoidance: There is often a conscious effort to avoid anxiety-inducing places, such as crowded markets, public transportation, or open spaces like parking lots.
- Dependence on others: Some individuals may only venture into feared situations with a trusted companion.
- Physical symptoms: Encountering or anticipating the anxiety-provoking situation can lead to panic attacks, with symptoms like heart palpitations, sweating, trembling, abdominal distress, feeling dizzy, and shortness of breath.
- Behavior change: The individual's routine might change significantly as they take measures to avoid triggering environments.
- Functional impairment: This severe avoidance and distress can impair one's ability to perform routine tasks, work, socialize, and maintain relationships.
Beyond recognizing these symptoms, it is also essential to understand the possible origins of agoraphobia. While the exact cause of agoraphobia is not yet fully confirmed and still requires extensive studies, the risk of developing this disorder is attributed to a combination of the following factors:
- Biological and genetic factors: There may be genetic components at play, and some people might have a predisposition to the disorder.
- Temperament: Traits such as nervousness or a tendency toward negative emotions can increase susceptibility.
- Experiences: Those who've suffered panic attacks or other intensely fearful situations may become worried about experiencing these feelings again, leading to agoraphobia.
- Learned responses: Observing others exhibit fearful behavior in response to specific situations may also contribute to the development of agoraphobia.
How do healthcare professionals diagnose agoraphobia?
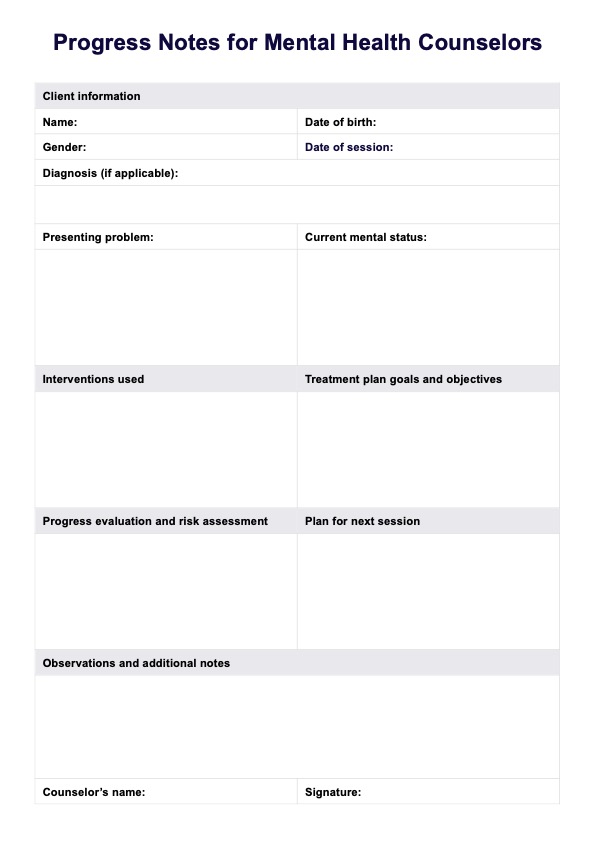
Healthcare professionals diagnose agoraphobia through a comprehensive process that involves assessing reported symptoms, conducting physical examinations, and ruling out other potential medical conditions. The diagnosis is primarily symptom-based, with mental health professionals relying on the individual's description of their experiences and behaviors related to anxiety and avoidance of specific situations (National Health Service, 2021).
Professionals usually take the following steps to diagnose agoraphobia:
Step 1: Initial consultation and history-taking
The assessment process starts with a comprehensive history taking, documenting the client's symptoms, duration and frequency, and any situations that trigger them. Particular attention should be given to the individual's emotional response to experiencing or thinking about such situations.
Step 2: Identifying fear patterns
Determine if the individual has developed patterns of avoidance behavior or reliance on others to manage feared situations. It's important to differentiate between fear of the situation and the response (for example, panic attacks) it might provoke.
Step 3: Mental health review
A detailed mental health assessment should be conducted to identify any past or current psychiatric conditions. This includes exploring potentially comorbid disorders such as other anxiety disorders, depression, or substance use disorders. It is also essential to use evidence-based assessments to gain more insights about an individual and possible presentations of agoraphobia, such as the Mobility Inventory for Agoraphobia.
Step 4: Physical examination and labs
While there are no specific physical findings or lab tests that can diagnose agoraphobia, they may help rule out medical conditions that can mimic its symptoms, such as thyroid disorders or certain heart conditions.
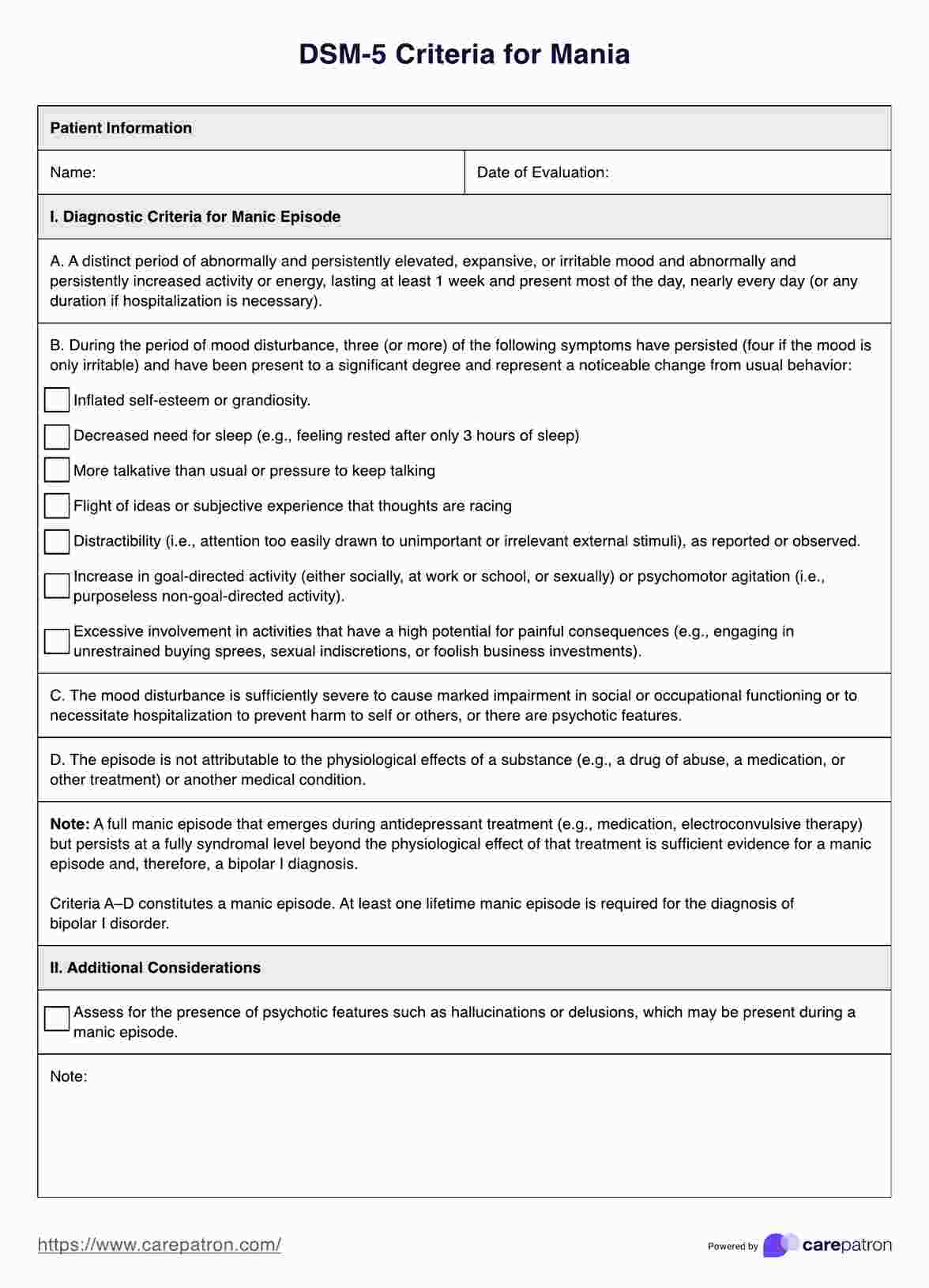
Step 5: Referring to DSM-5 diagnostic criteria
The DSM-5 outlines specific criteria for diagnosing agoraphobia. According to the DSM-5, an individual must demonstrate marked fear or anxiety about two or more scenarios, such as using public transportation, being in open or enclosed spaces, standing in line or being in a crowd, or being outside the home alone. This fear or anxiety must be out of proportion to the actual danger posed by these situations, causing significant distress and interfering with daily functioning.
Step 6: Follow-up consultations
Regularly reassess the individual's condition as per treatment response or changes in circumstances. In cases where a firm diagnosis was not initially possible, these follow-ups may help draw other definitive conclusions.
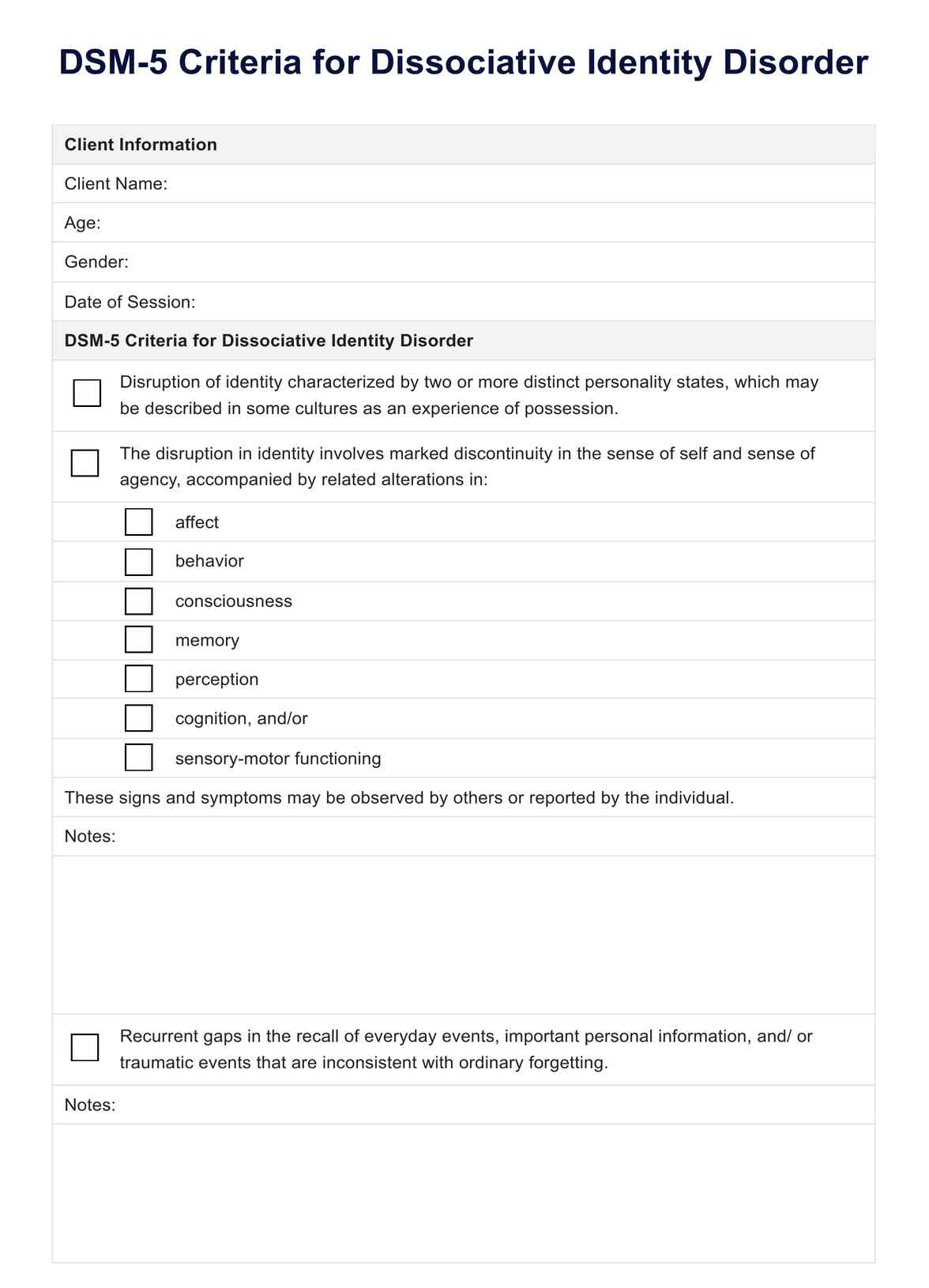
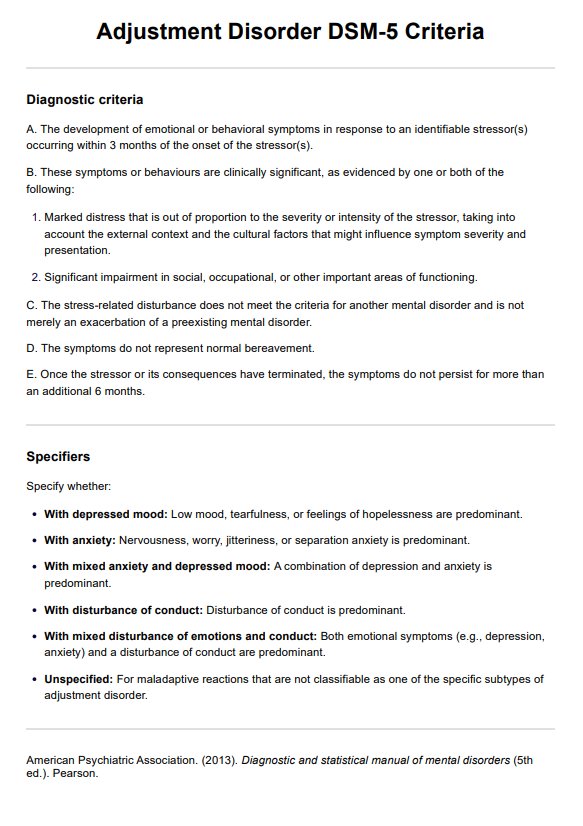
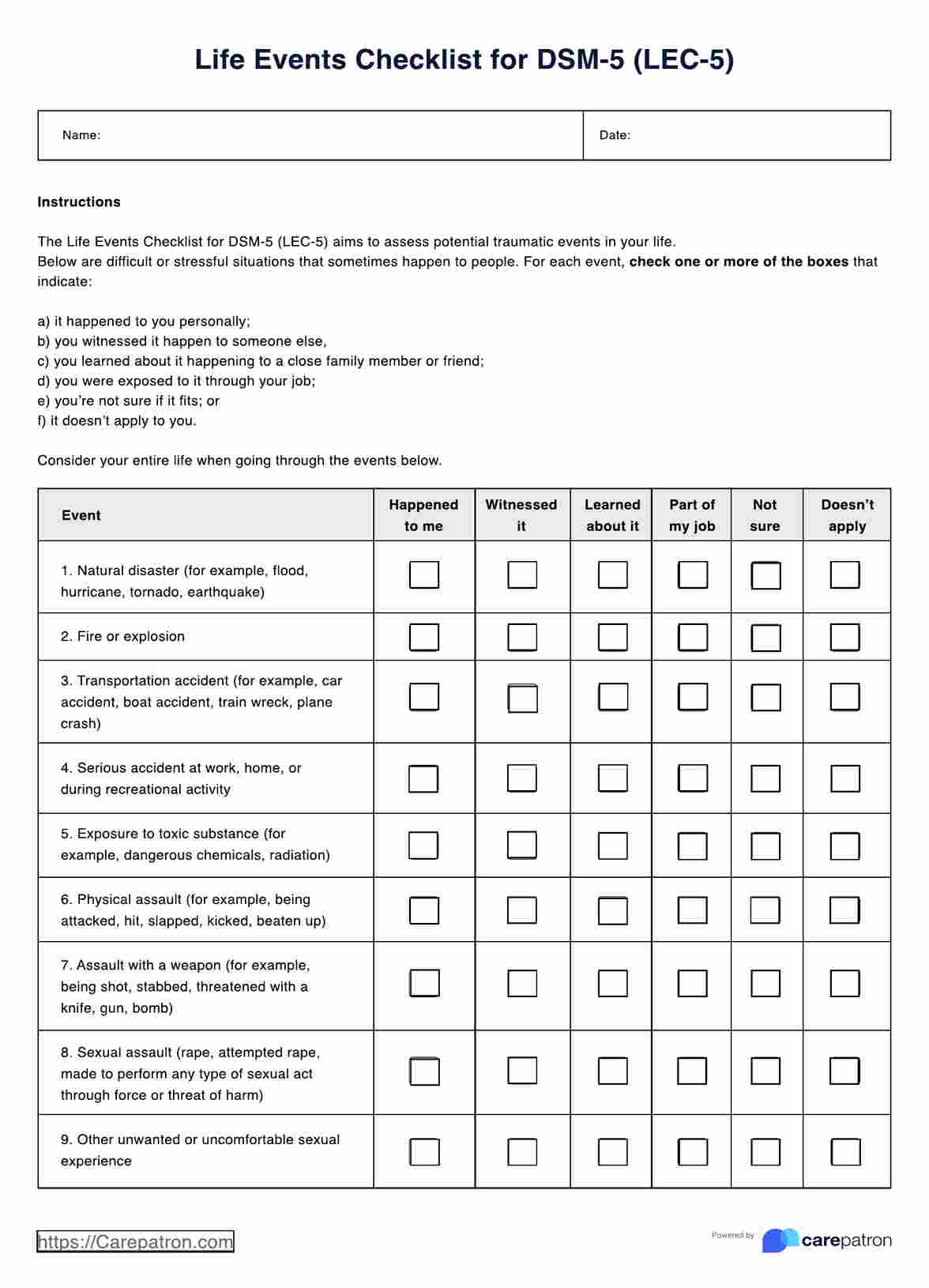
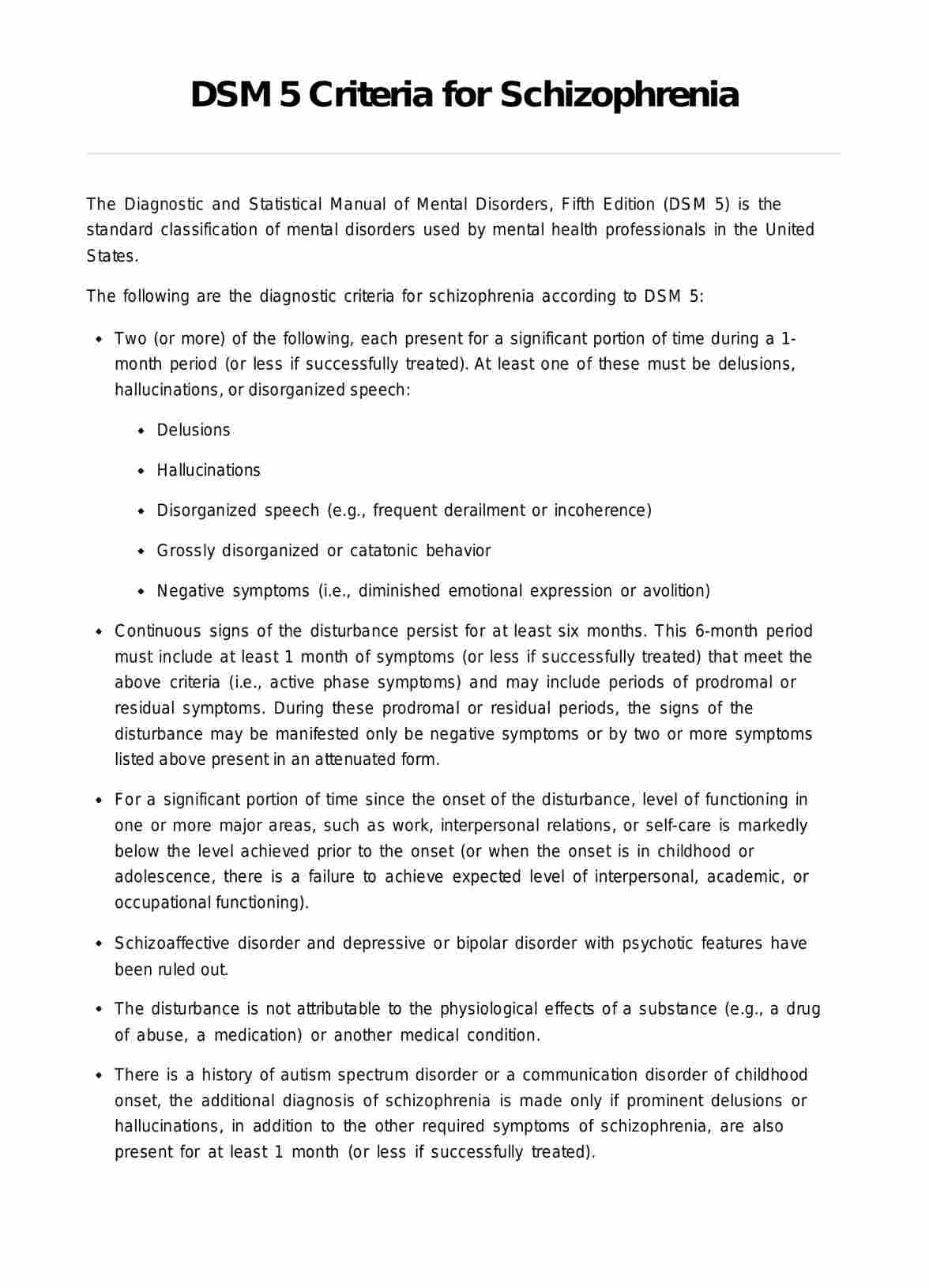
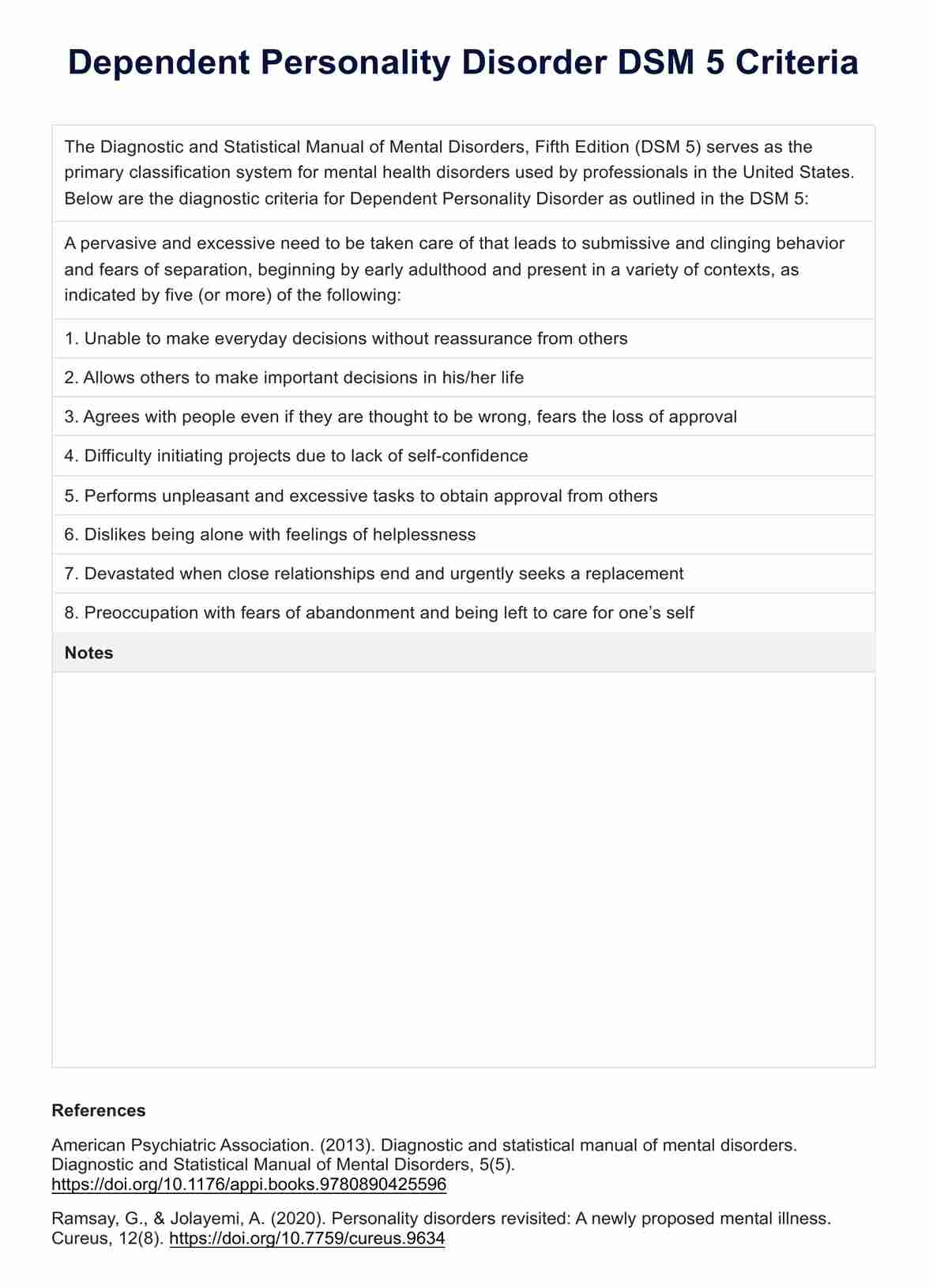
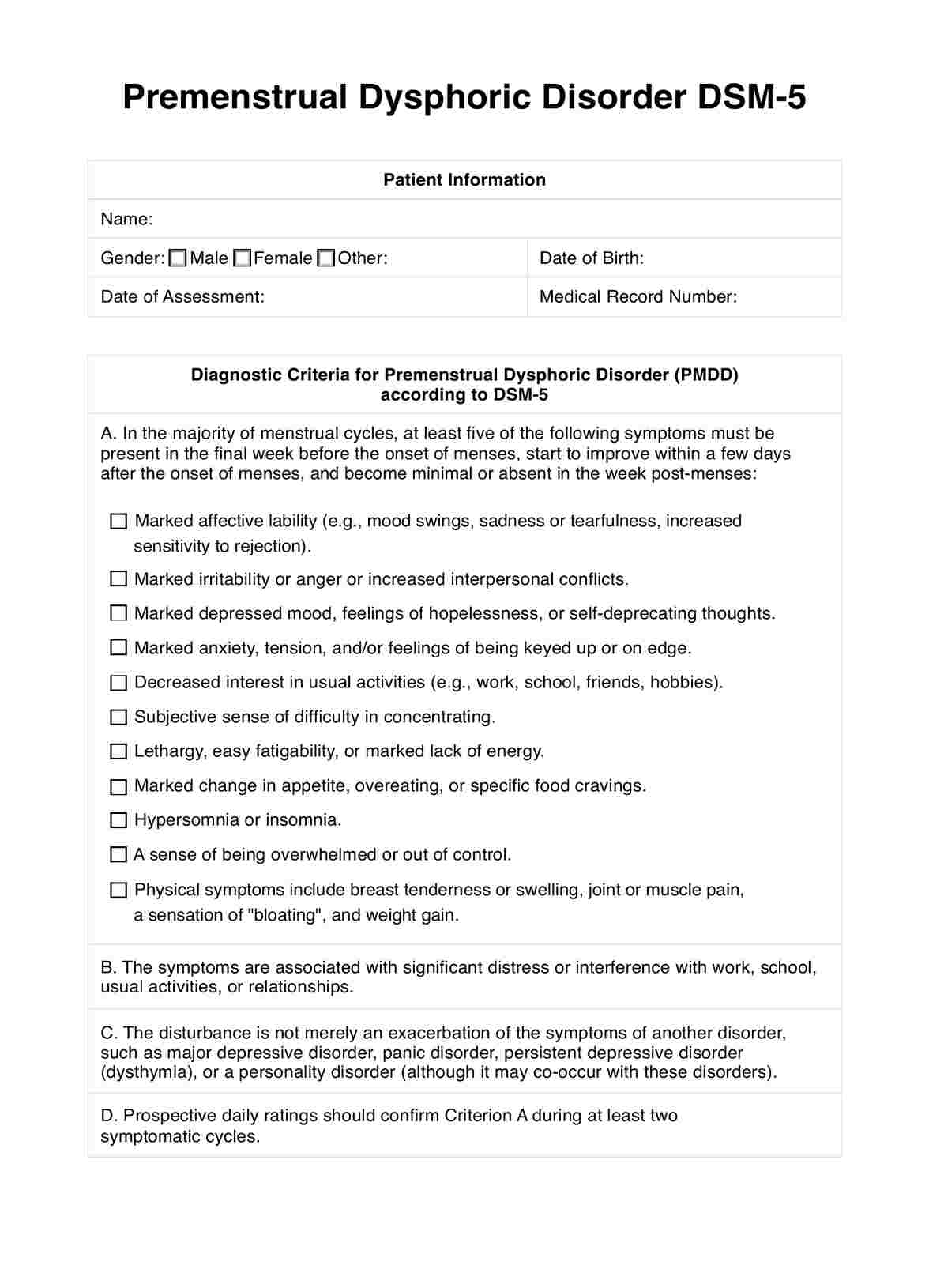
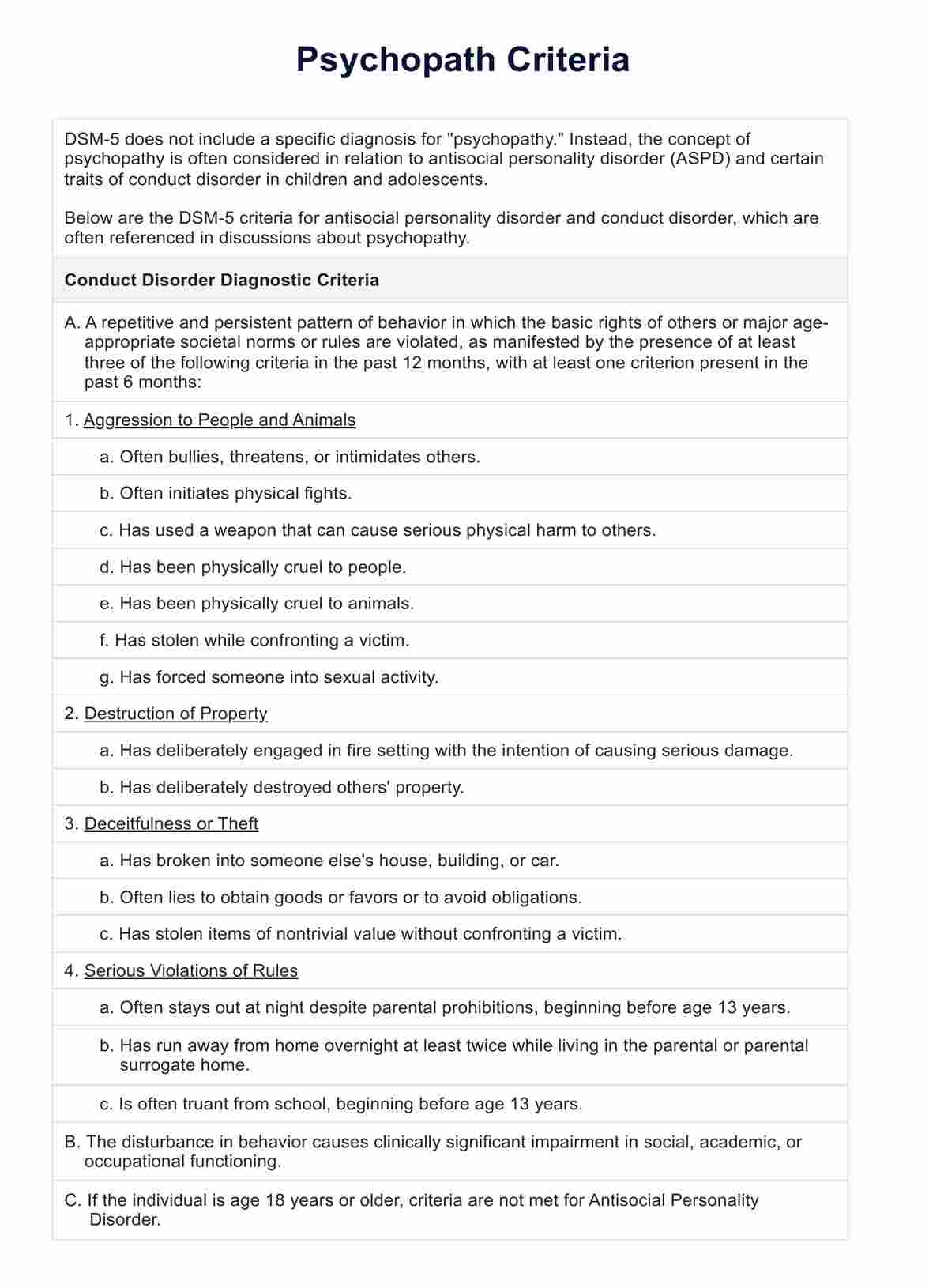
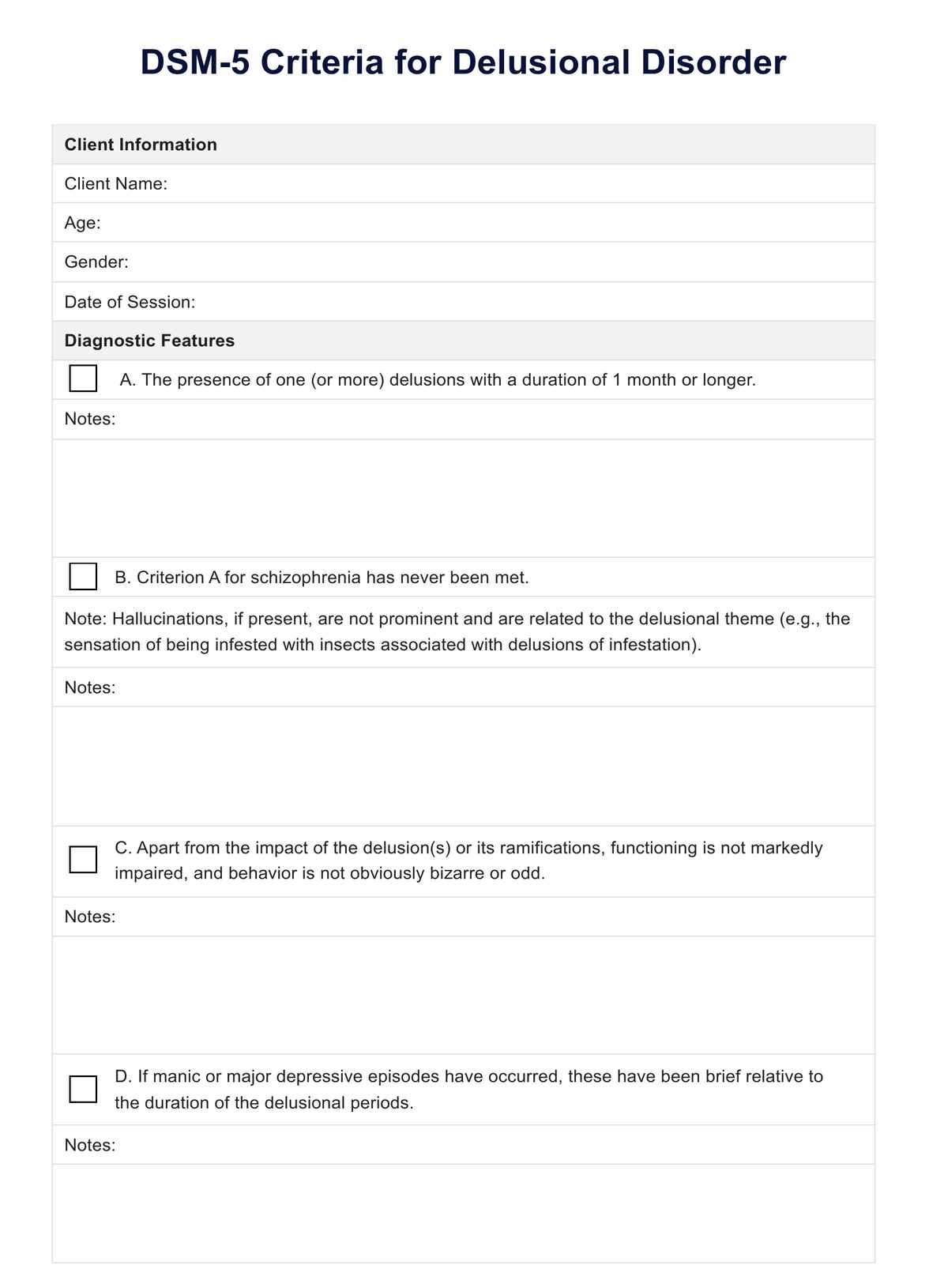
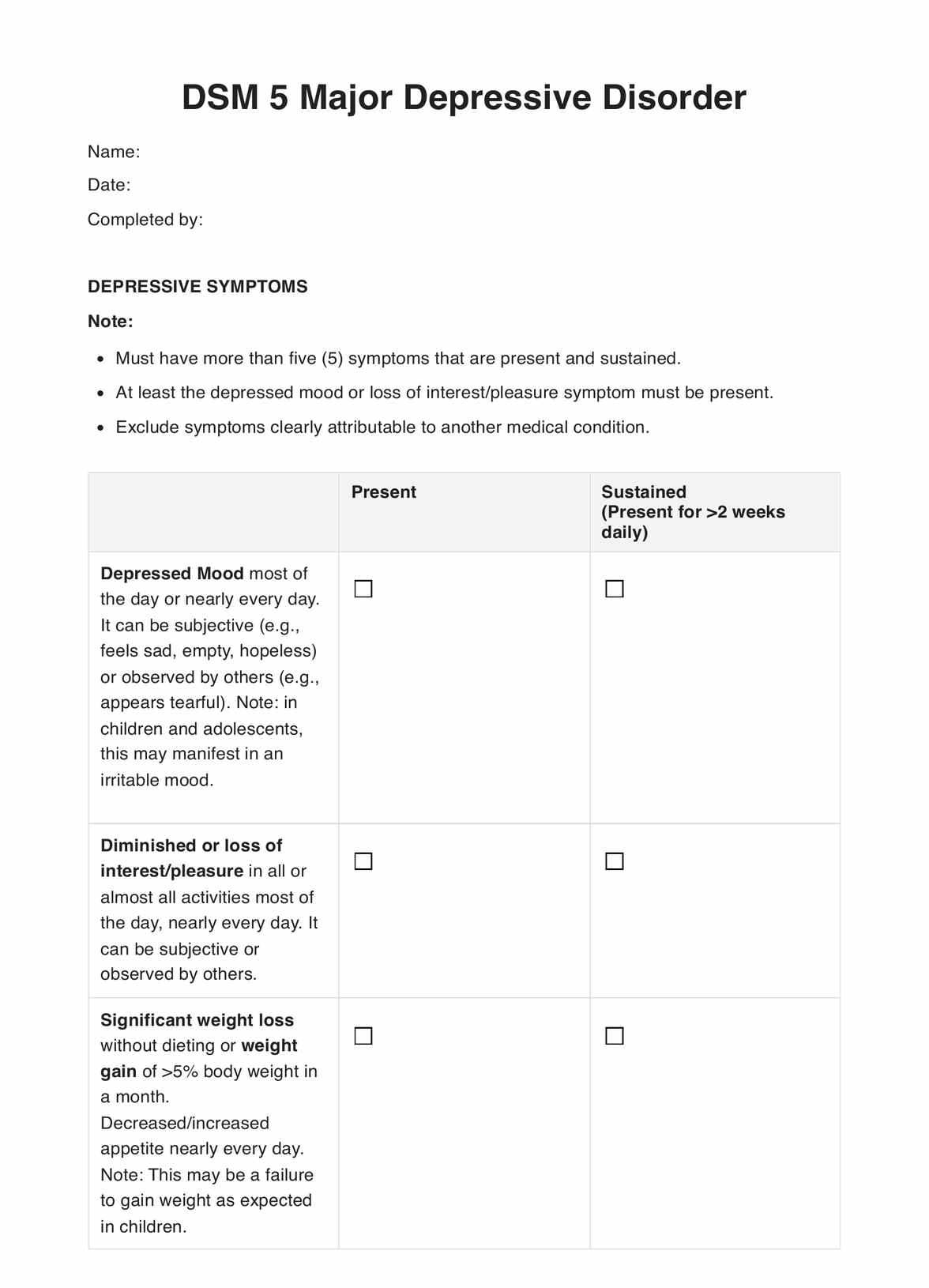
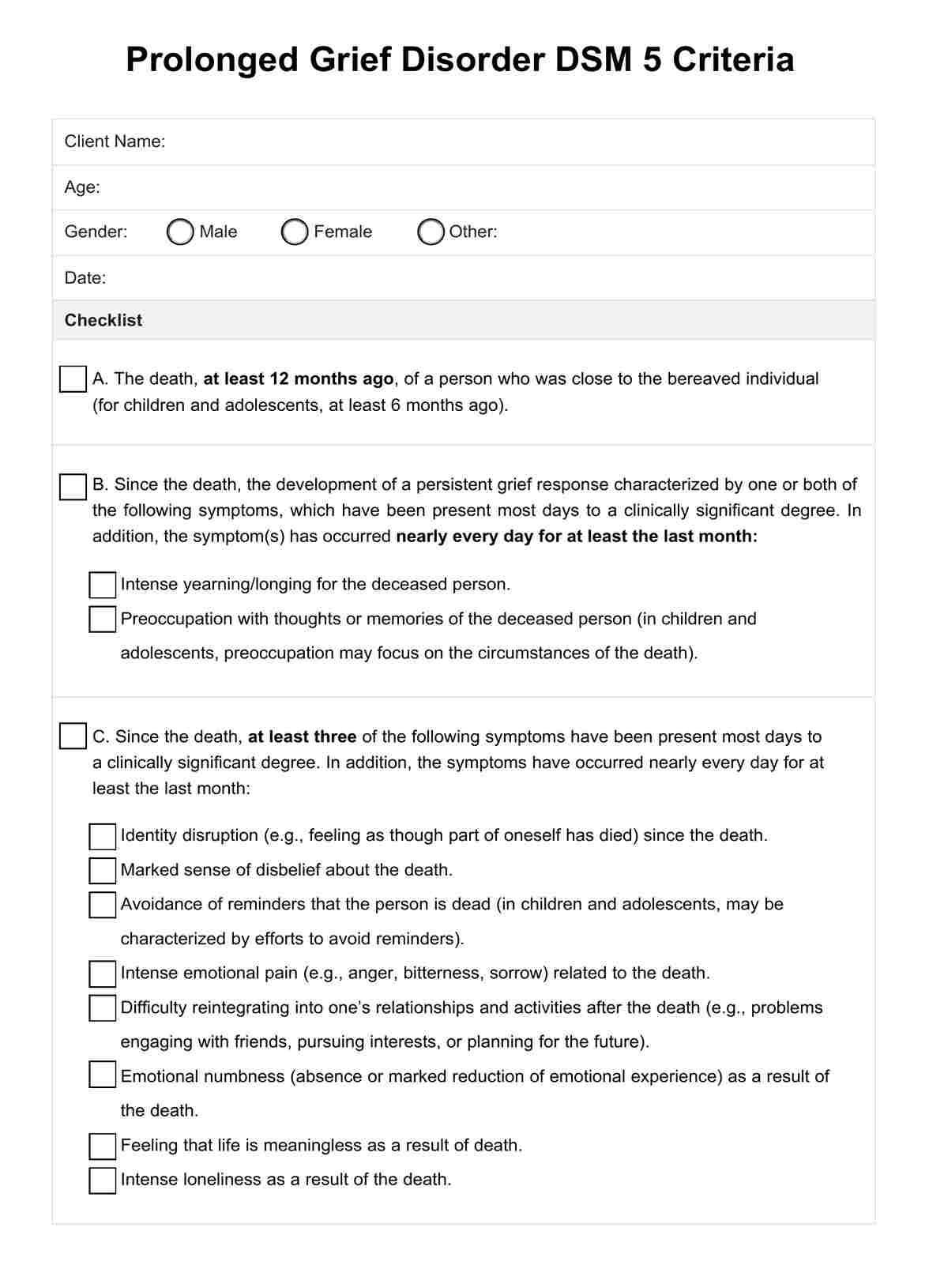
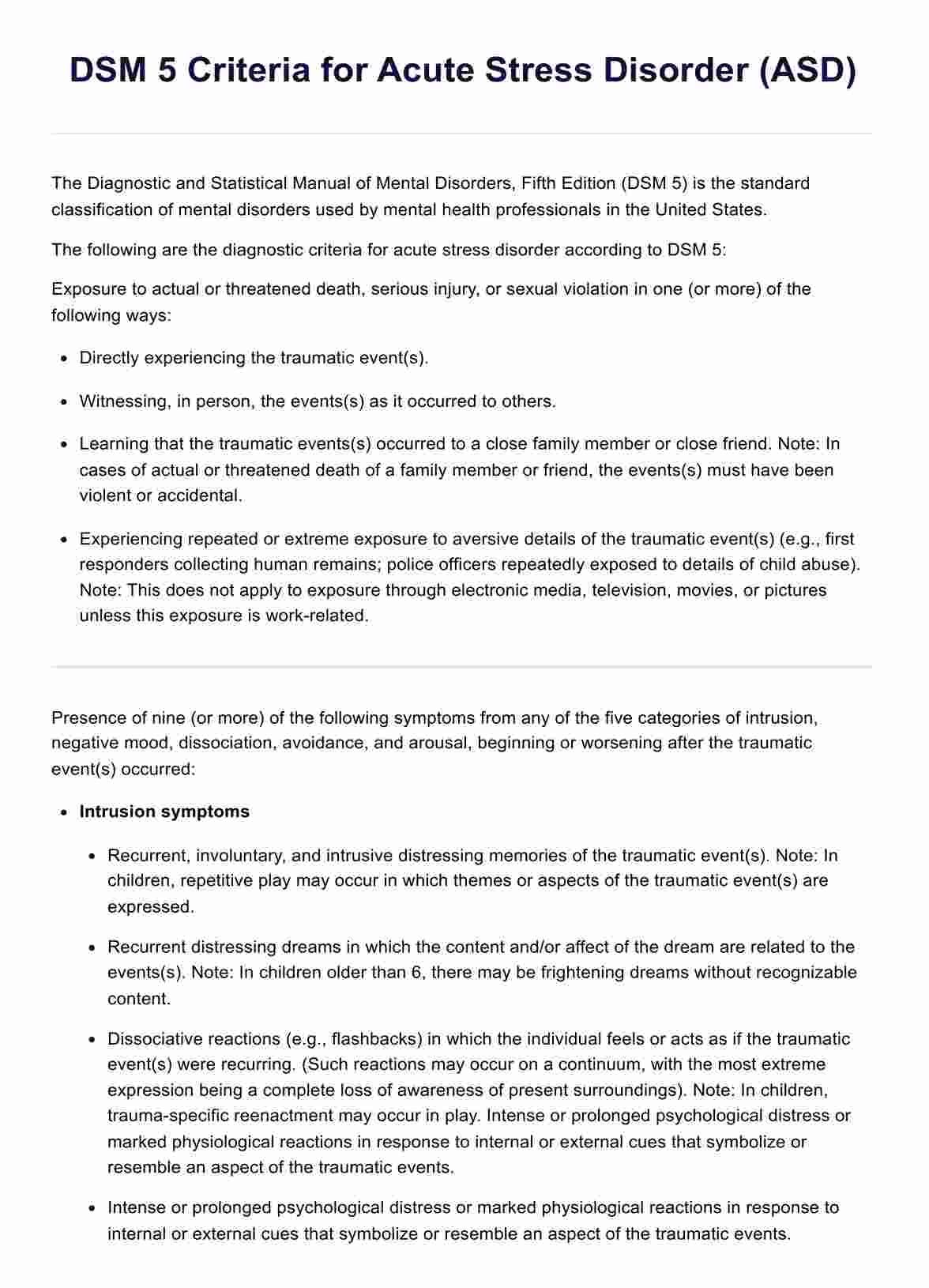
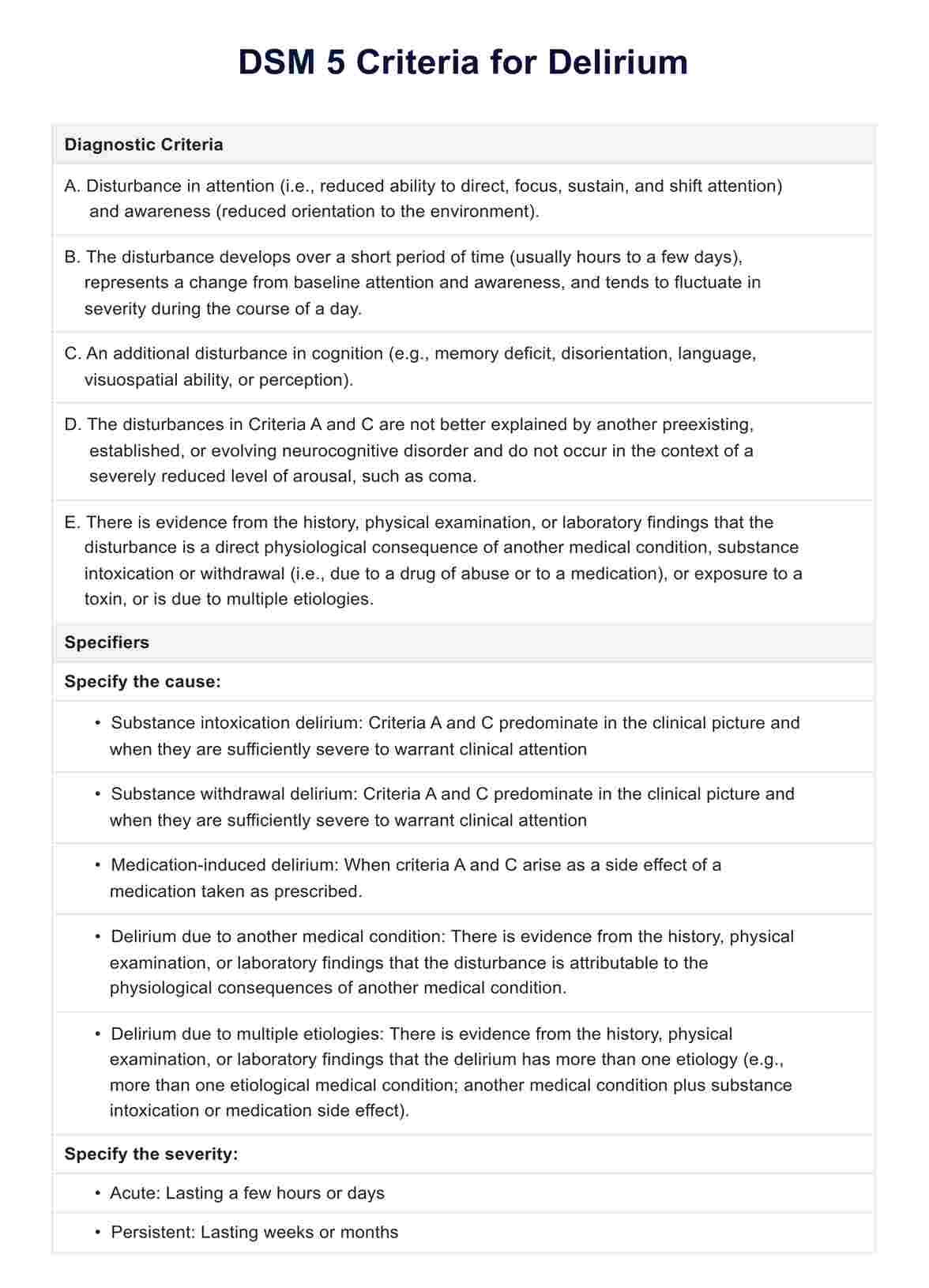
What are the DSM 5 criteria for diagnosing agoraphobia?
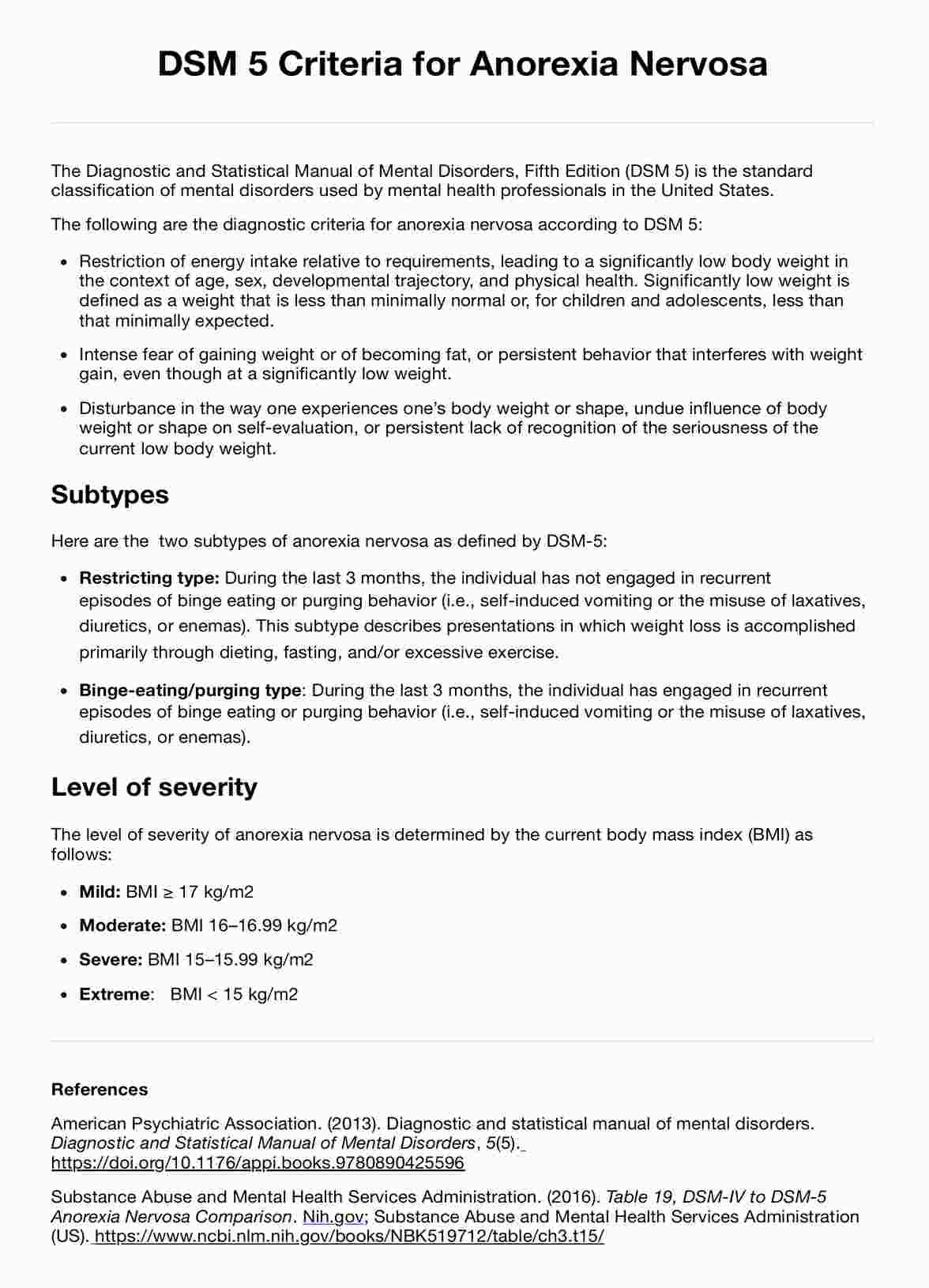
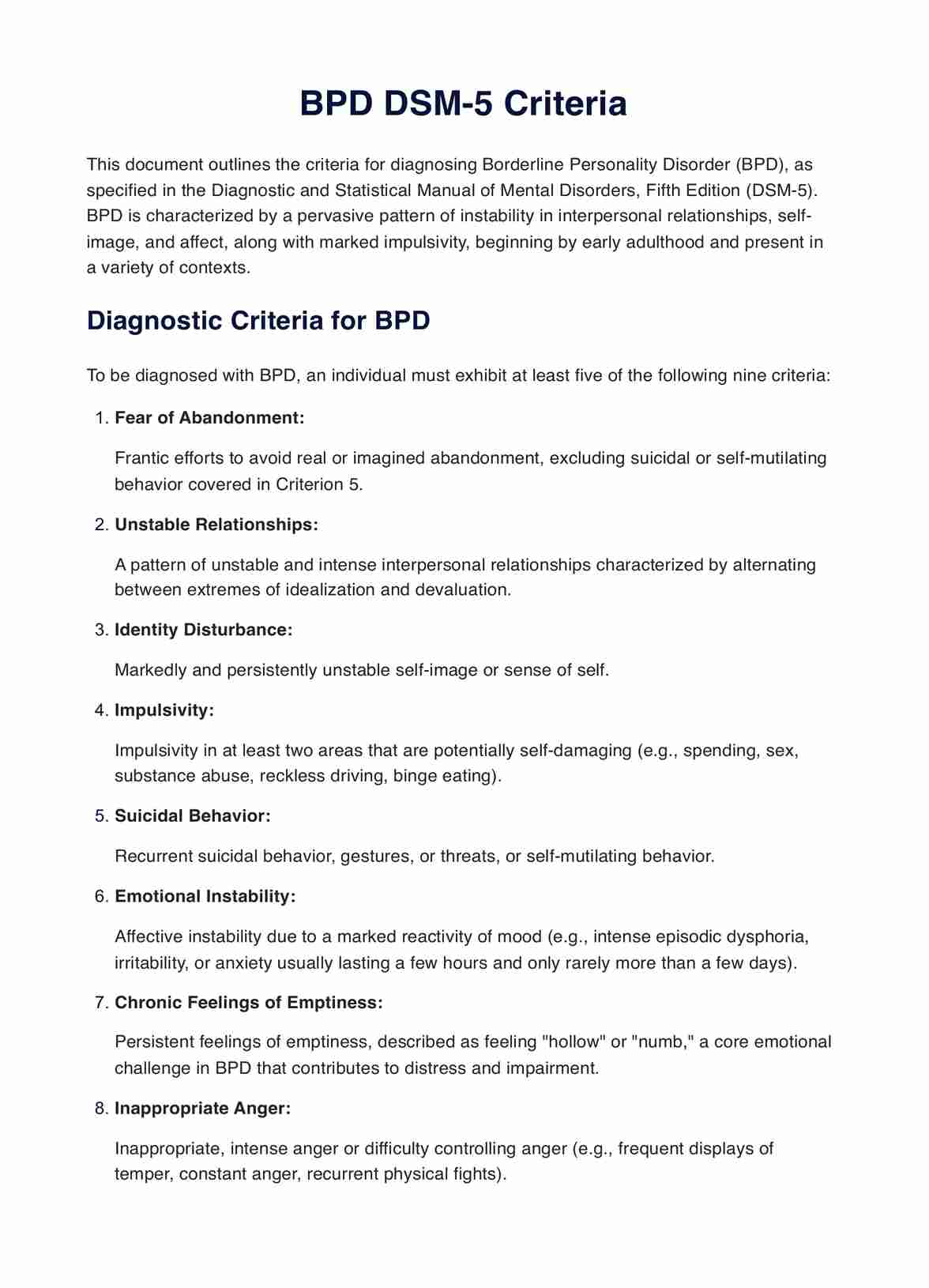
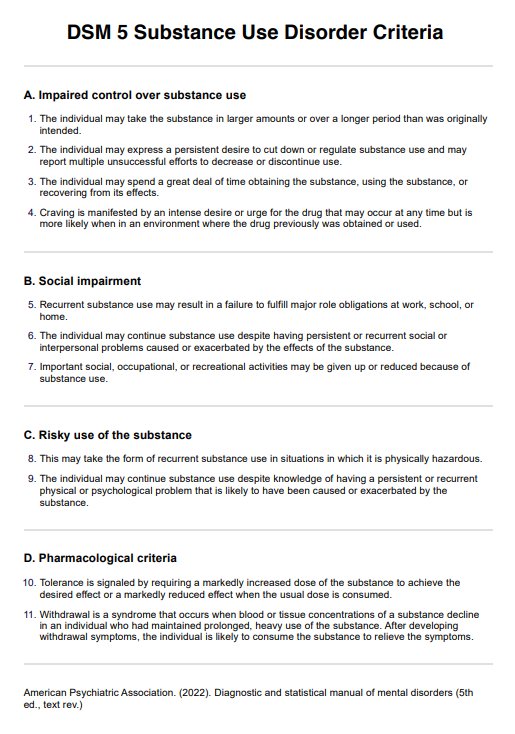
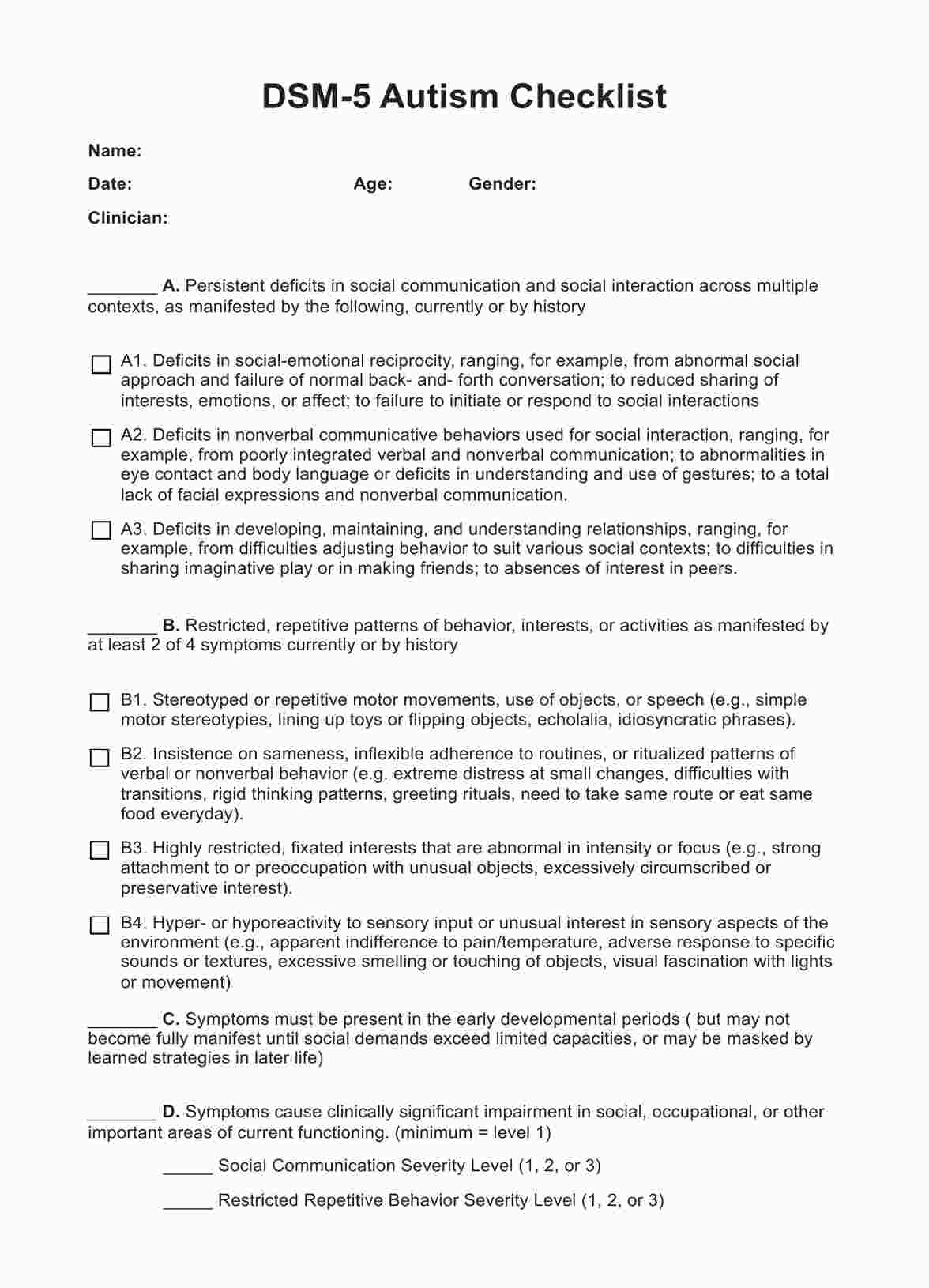
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), is a critical tool for mental health professionals. It provides standardized criteria to diagnose and classify mental disorders, ensuring consistency and reliability across various settings. For diagnosing agoraphobia, the American Psychological Association (2013) offers specific criteria in the DSM-5 that guide healthcare practitioners in identifying and differentiating this mental disorder from other anxiety-related conditions. The diagnostic criteria include the following:
- Marked fear or anxiety about two (or more) of the following five situations:
- Using public transportation (e.g., automobiles, buses, trains, ships, planes).
- Being in open spaces (e.g., parking lots, marketplaces, bridges).
- Being in enclosed places (e.g., shops, theaters, cinemas).
- Standing in line or being in a crowd.
- Being outside of the home alone. The individual fears or avoids these situations because of thoughts that escape might be difficult or help might not be available in the event of developing panic-like symptoms or other incapacitating or embarrassing symptoms (e.g., fear of falling in the elderly, fear of incontinence).
- The agoraphobic situations almost always provoke fear or anxiety.
- The agoraphobic situations are actively avoided, require the presence of a companion, or are endured with intense fear or anxiety.
- The fear or anxiety is out of proportion to the actual danger posed by the agoraphobic situations and to the sociocultural context.
- The fear, anxiety, or avoidance is persistent, typically lasting for 6 months or more.
- The fear, anxiety, or avoidance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.
- If another medical condition (e.g., inflammatory bowel disease, Parkinson's disease) is present, the fear, anxiety, or avoidance is clearly excessive.
- The symptoms of another mental disorder do not better explain the fear, anxiety, or avoidance—for example, the symptoms are not confined to specific phobia or situational type; they do not involve only social situations (as in social anxiety disorder), and are not related exclusively to obsessions (as in obsessive-compulsive disorder), perceived defects or flaws in physical appearance (as in body dysmorphic disorder), reminders of traumatic events (as in posttraumatic stress disorder), or fear of separation (as in separation anxiety disorder).
What is the relationship between panic disorder and agoraphobia?
The development of agoraphobia is commonly associated with the experience of panic attacks. Many individuals with agoraphobia report that the fear of enduring a panic attack, particularly in a situation where escape might be difficult or help unavailable, serves as a fundamental reason for their avoidance behaviors. The intensity of a panic attack may be so overwhelming that the fear of this happening again drives individuals to avoid places or situations where they predict it could happen again.
While panic attacks are a notable feature of panic disorder, they can also be a part of agoraphobia. However, a key distinction is that in a panic disorder diagnosis, the panic attacks are unexpected and not consistently triggered by specific situations. In contrast, agoraphobia is marked by avoidance of situations due to the fear evoked by the thoughts of being unable to escape or get help in the case of such an attack or other embarrassing symptoms.
How does our Agoraphobia DSM 5 Criteria template work?
The Agoraphobia DSM-5 Criteria Template can help us professionals accurately identify this anxiety disorder by evaluating specific symptoms experienced by a client. Here's a step-by-step guide on how to use this tool effectively in a clinical setting:
Step 1: Understand the DSM-5 criteria for agoraphobia
Familiarize yourself with the criteria for agoraphobia as per DSM-5 before using the template and the common representation of these symptoms.
Step 2: Use the template during the assessment
During the client interview, use the template as a structured checklist to explore the individual's symptoms, checking off each criterion.
Step 3: Analyze symptoms and impact
Probe into the scenarios that cause the anxiety symptoms and fear experienced by the individual. Assess the level of distress and how these fears impact their daily functioning. If panic experiences are prevalent, consider related disorders like panic disorder.
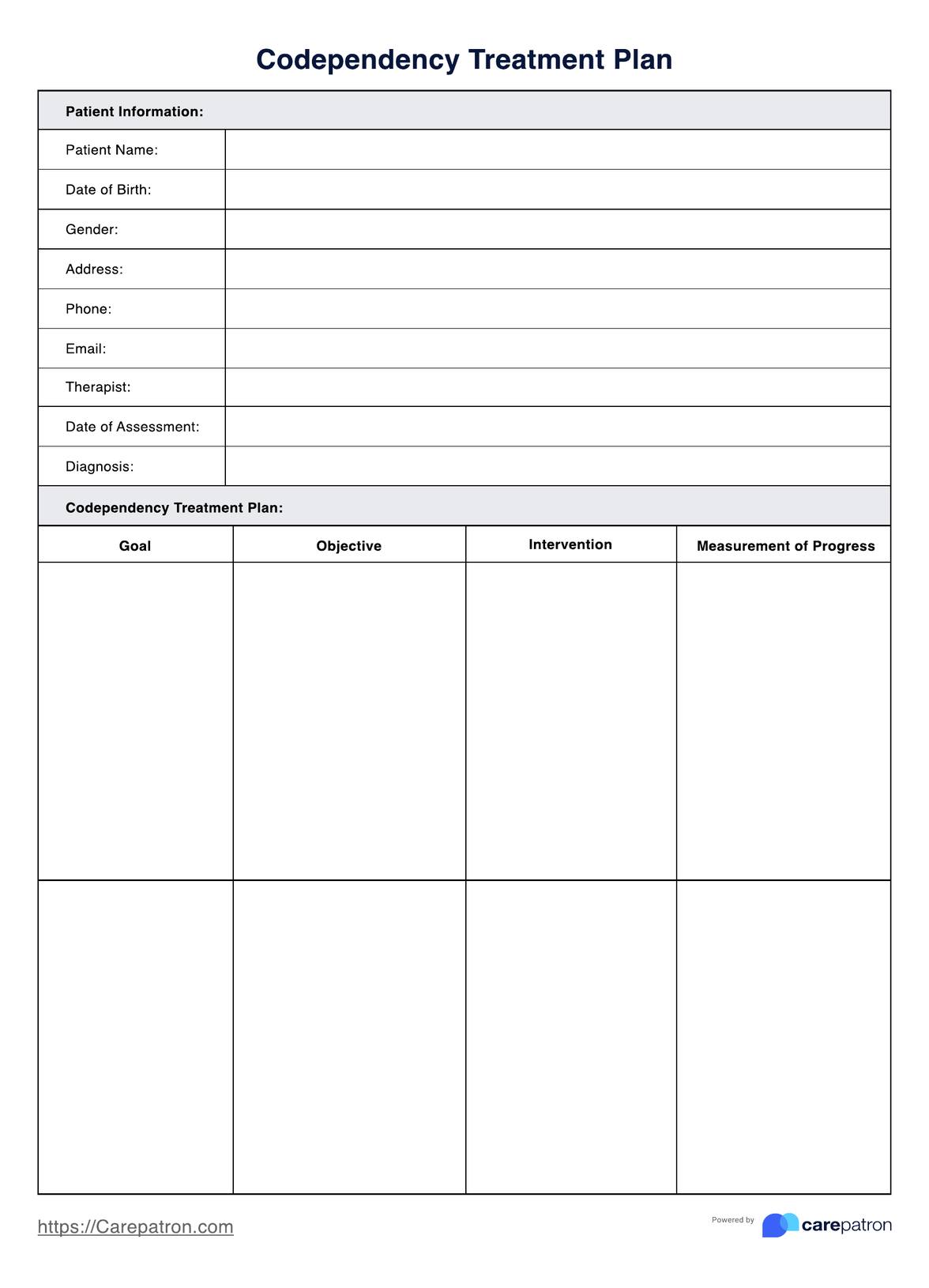
Step 4: Make a diagnosis and treatment plan
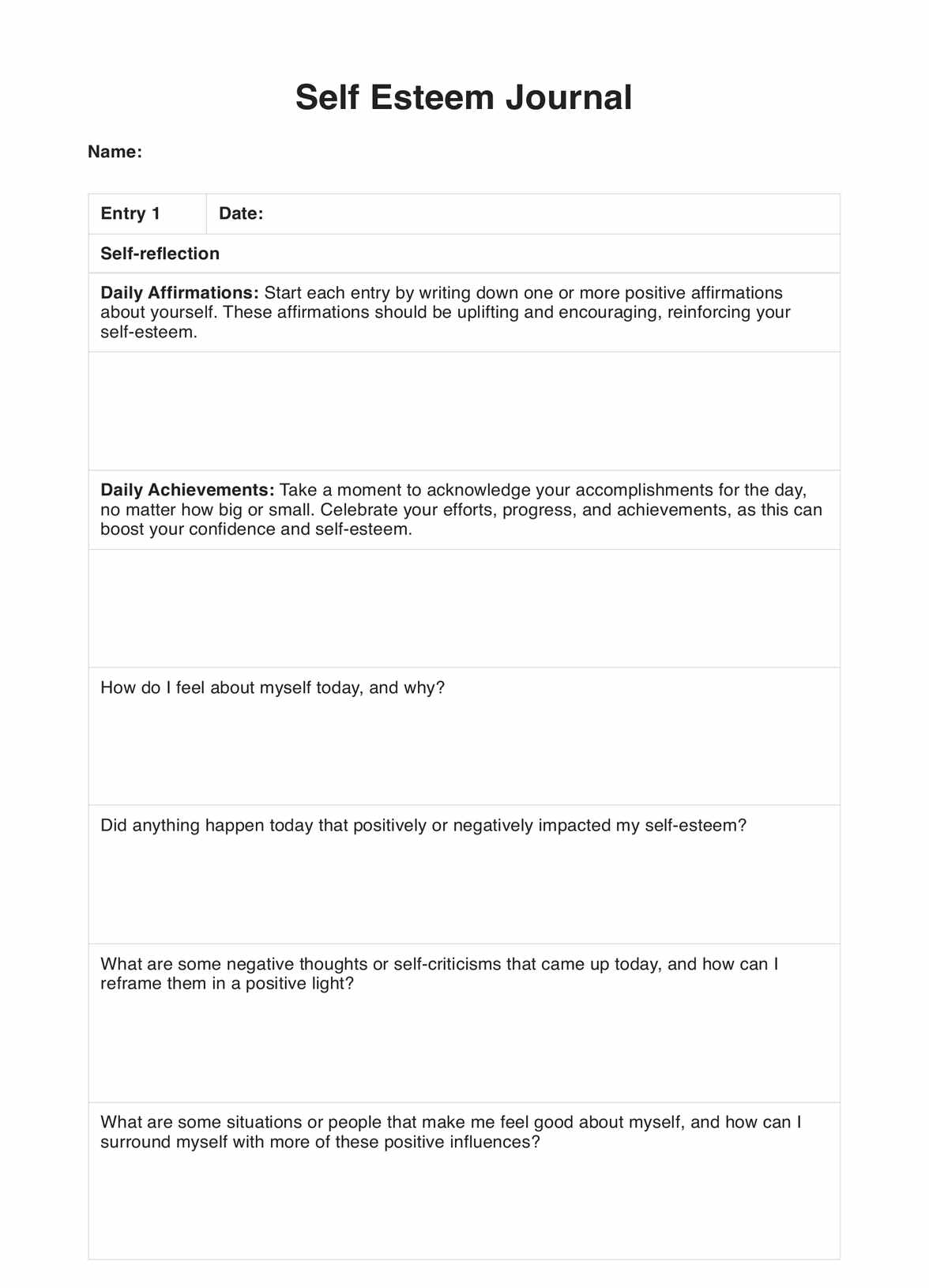
Based on the completed template review, finalize the diagnosis. It can also help develop a tailored treatment plan to use the results. Consider using the template in follow-ups to track progress and make necessary adjustments.
Agoraphobia treatment
Treating agoraphobia presents unique challenges. Understanding the scope and how these treatments work to address agoraphobia allows us, care providers, to form a more personalized and comprehensive treatment plan.
Cognitive behavioral therapy
CBT for agoraphobia is grounded in the principle that an individual's interpretation of situations influences their emotional and behavioral responses. It focuses on identifying and challenging negative thoughts and beliefs related to agoraphobic fears and systematically confronting and reducing avoidance behaviors.
Pharmacotherapy
Medication may be used alongside CBT, tailored to the individual's needs. Selective serotonin reuptake inhibitors (SSRIs) and serotonin and norepinephrine reuptake inhibitors (SNRIs) are commonly preferred for their efficacy and safety. Less frequently, benzodiazepines may be used.
Patient-centered approach
Treatment should suit individual needs, including symptom severity, psychiatric comorbidities, patient preference, and personal circumstances.
Long-term management
Long-term management aims at maintaining therapeutic gains and early detection of any sign of relapse. This involves regular follow-ups, reassessments, and fine-tuning therapy as required.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC.
Barlow, D. H., Mark, V., & Hofmann, S. G. (2018). Abnormal psychology: An integrative approach (8th ed.). Cengage Learning.
National Health Service. (2021). Diagnosis - agoraphobia. Nhs. uk. https://www.nhs.uk/mental-health/conditions/agoraphobia/diagnosis/
Roest, A. M., de Vries, Y. A., Lim, C. C. W., Wittchen, H.-U., Stein, D. J., Adamowski, T., Al-Hamzawi, A., Bromet, E. J., Viana, M. C., de Girolamo, G., Demyttenaere, K., Florescu, S., Gureje, O., Haro, J. M., Hu, C., Karam, E. G., Caldas-de-Almeida, J. M., Kawakami, N., Lépine, J. P., & Levinson, D. (2019). A comparison of DSM-5 and DSM-IV agoraphobia in the world mental health surveys. Depression and Anxiety, 36(6), 499–510. https://doi.org/10.1002/da.22885
Commonly asked questions
No. Agoraphobia and social anxiety disorder (social phobia) are two different conditions. Social anxiety focuses on a fear of social situations due to worries about embarrassment or being judged. Agoraphobia is a fear of being in situations where escape may be tricky, or help might not be available in the event of a panic attack.
Agoraphobia can heavily impact daily functioning, leading to avoidance of various places or situations, difficulty traveling far from home, or needing a companion when out of the house, thereby restricting independence and social interactions.
Agoraphobia can occur with or without panic disorder. With panic disorder, the person experiences panic attacks and intense fear of having one in specific situations. Agoraphobia without panic disorder involves fear of the situations themselves, not necessarily linked to expected or unexpected panic attacks.




















-template.jpg)