Other than dissociative identity disorder (DID), three other main types of dissociative disorders are recognized. First is dissociative amnesia, a significant memory loss not associated with a physical condition. Then, there is also depersonalization/derealization disorder, where individuals experience a sense of detachment from themselves or their surroundings. Finally, there is a dissociative fugue, a subtype of dissociative amnesia featuring sudden, unexpected travel and confusion about personal identity.
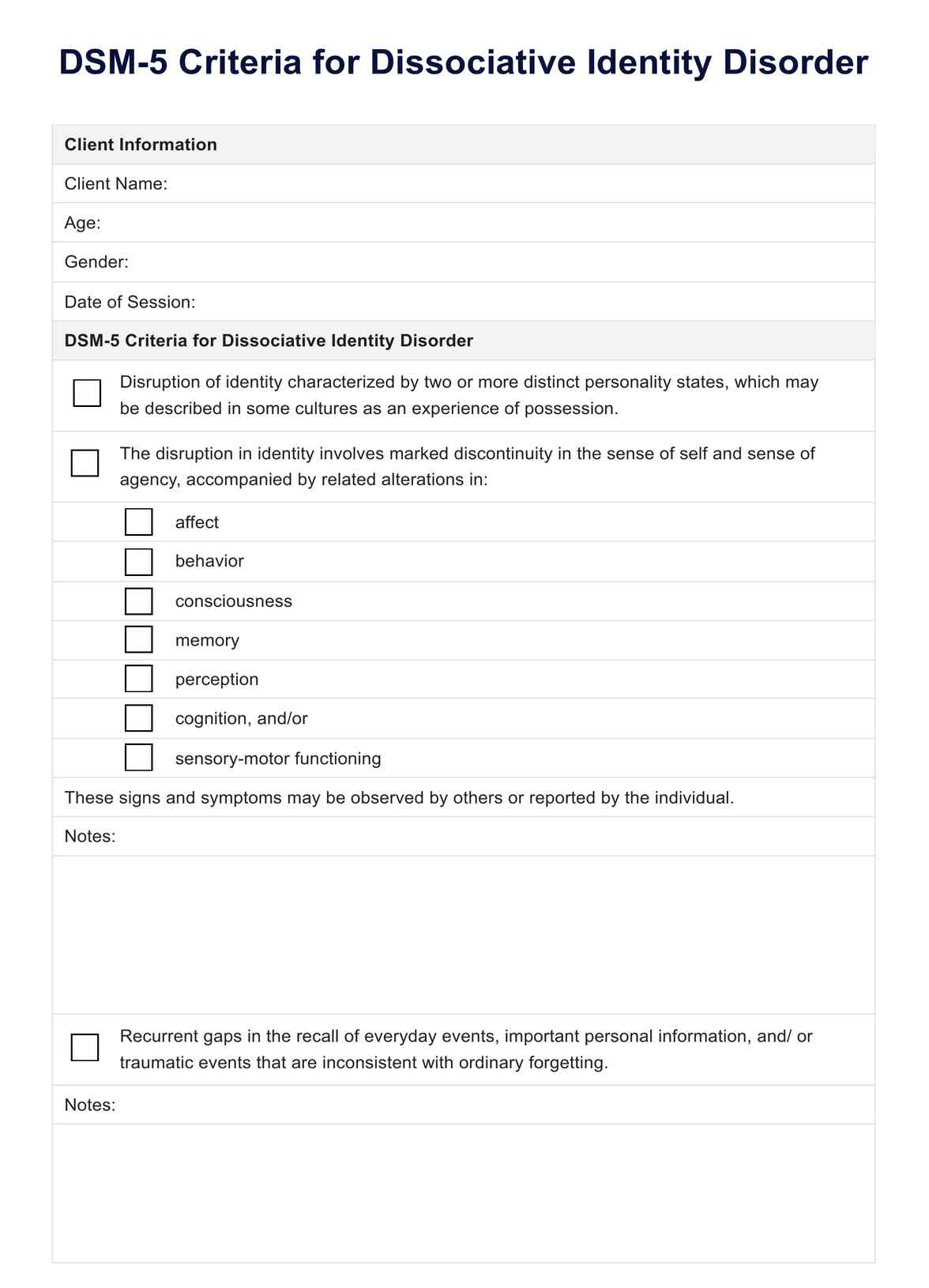
DID DSM-5 Criteria
Guide your diagnostic process of dissociative identity disorder with our DID DSM-5 Criteria checklist. Access your free PDF resource here.
DID DSM-5 Criteria Template
Commonly asked questions
The cause of dissociative identity disorder (DID) is typically severe trauma during early childhood, often in the form of repetitive physical, sexual, or emotional abuse, leading to dissociation as a coping mechanism.
Conditions that can be mistaken for dissociative identity disorder (DID) include borderline personality disorder, which may feature dissociative states. Schizophrenia is also included due to its hallucinations and disorganized thinking. Bipolar disorder, where drastic mood swings could also mimic identity switches, and post-traumatic stress disorder, given its dissociative symptoms associated with trauma.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











