Dependent Personality Disorder DSM 5 Criteria
Learn about Dependent Personality Disorder DSM 5 Criteria, understand symptoms and treatment to form healthy relationships. Download the free PDF now.


What is dependent personality disorder (DPD)?
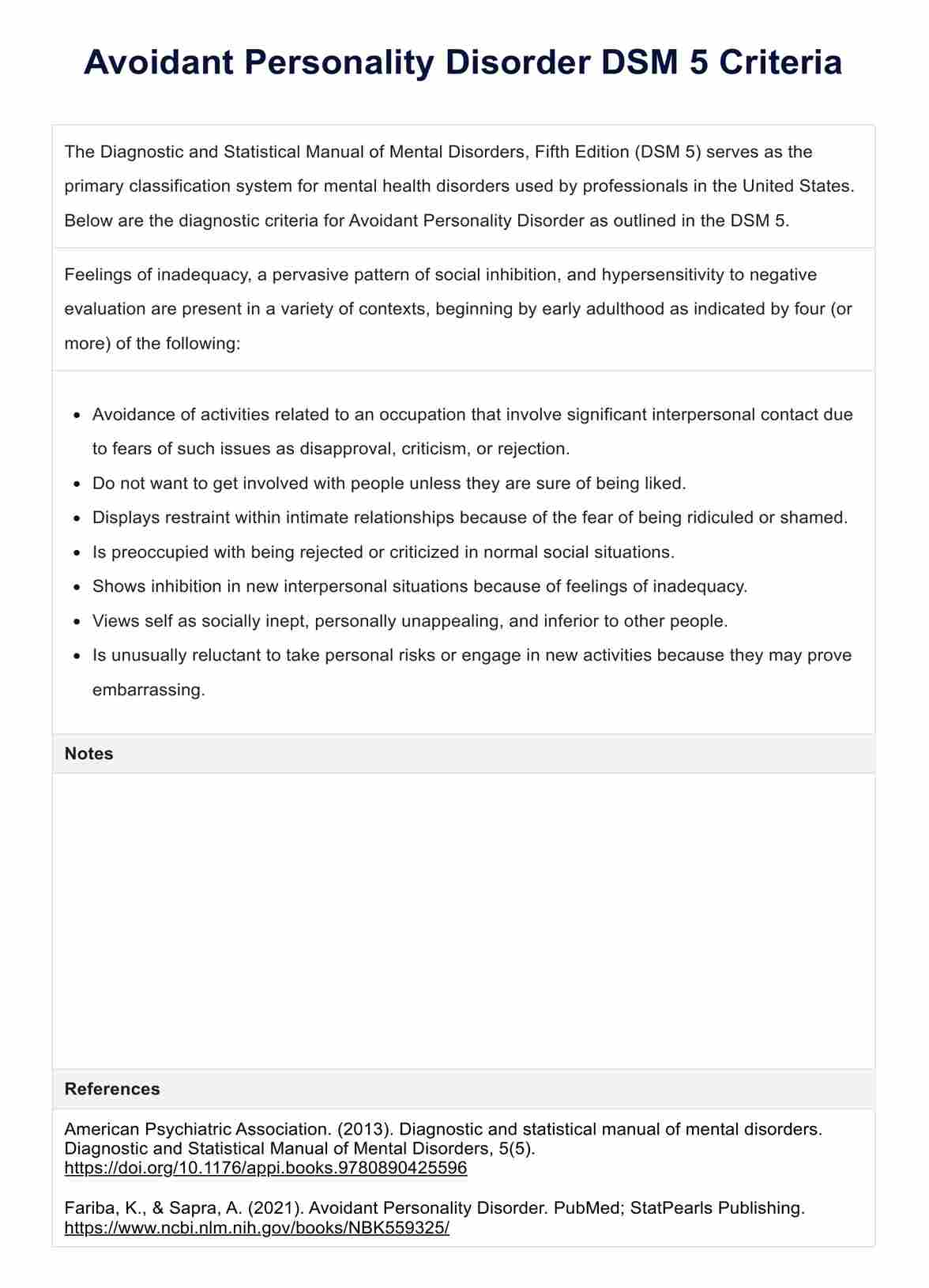
Personality disorders refer to persistent and ingrained patterns of thoughts, emotions, and actions that significantly stray from what is typical within a particular culture. These patterns often lead to difficulties in functioning and maintaining relationships. They're typically categorized into clusters, with Cluster C personality disorders exhibiting a common thread of encountering unwarranted anxiety, unusual fears, and a longing for unattainable social connections. Included in this cluster are avoidant, dependent, and obsessive-compulsive personality disorders (American Psychiatric Association, 2013).
Individuals with Dependent Personality Disorder (DPD) display an overwhelming need for care, resulting in submissive behavior, difficulty making decisions independently, and a fear of abandonment, hindering their ability to maintain relationships autonomously.
People with DPD may sacrifice their own needs and desires to satisfy those of others, often to their disadvantage. This pattern of dependent behavior can impair daily functioning and cause significant distress. However, with appropriate therapy and support, individuals with DPD can learn to foster more independence and form stable relationships based on mutual respect and autonomy
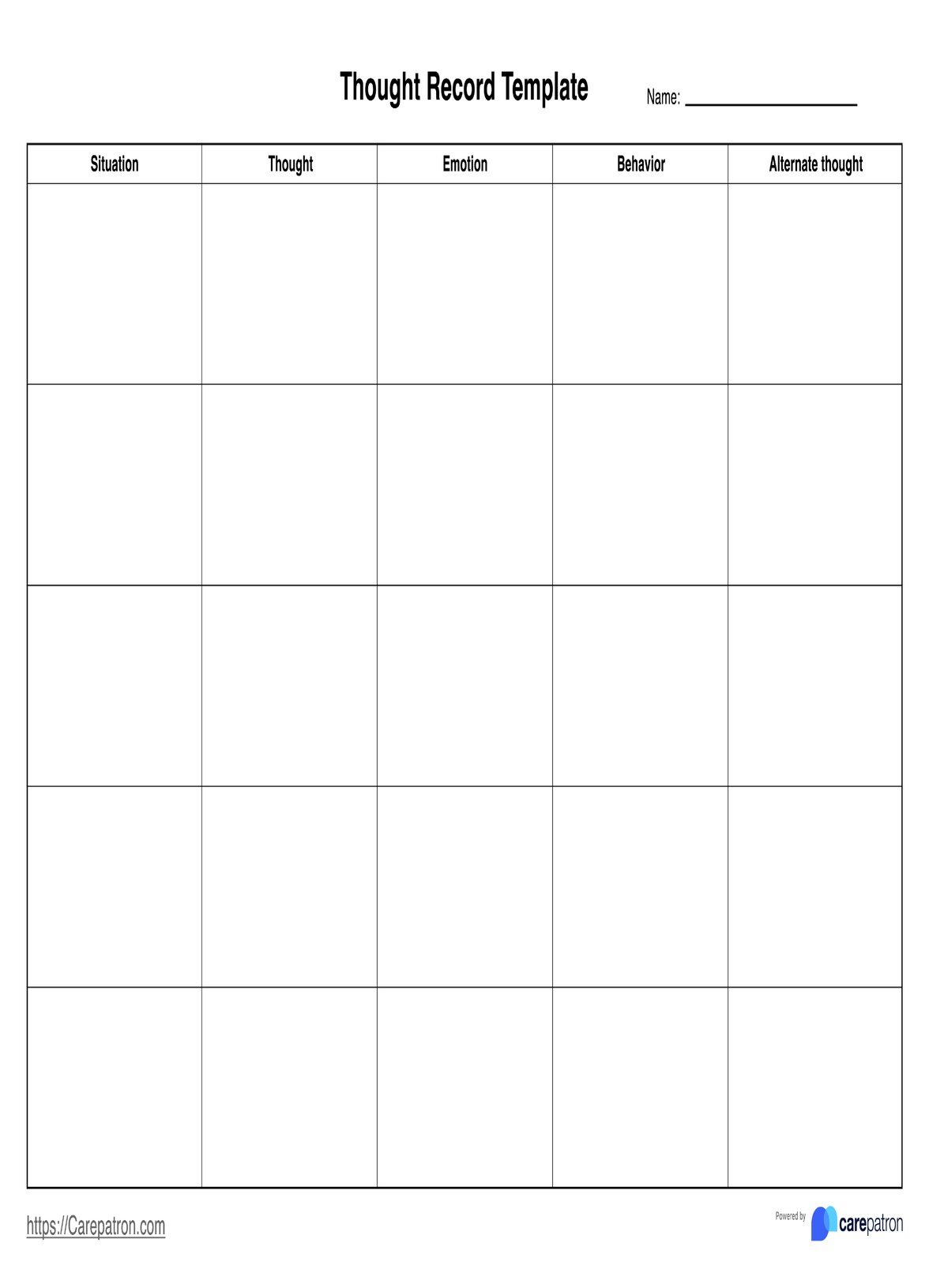
Dependent Personality Disorder DSM 5 Criteria Template
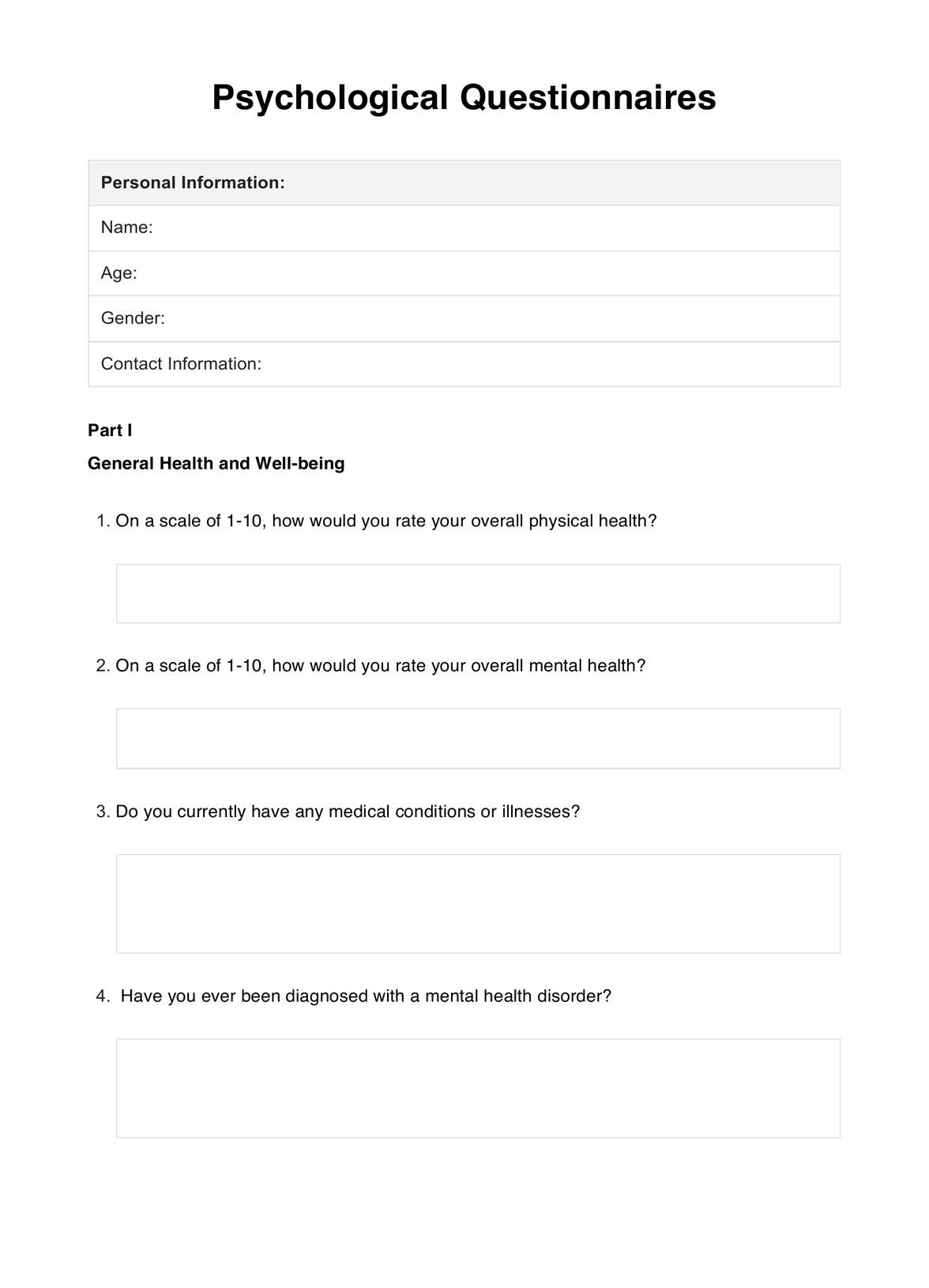
Dependent Personality Disorder DSM 5 Criteria Example
Dependent personality disorder symptoms
Understanding and addressing the underlying fears and insecurities driving their dependent behavior is crucial for effective treatment and long-term recovery. Zimmerman (2023) cites four symptoms of this specific personality disorder:
- Need for care: Those with dependent personality disorder rely heavily on others for support and guidance, seeking reassurance even for mundane decisions.
- Excessive submissiveness: Due to fear of losing support, individuals with dependent personality disorder may agree to actions they know are wrong and endure abuse rather than risk being alone.
- Lack of confidence: Those with dependent personality disorder perceive themselves as inferior, interpreting criticism as evidence of incompetence, further diminishing their self-esteem.
- Lack of independence: Individuals with dependent personality disorder avoid taking responsibility, struggle to initiate tasks independently, and fear appearing too competent, hindering their career advancement.
How does dependent personality disorder develop?
Dependent Personality Disorder (DPD) often develops through a complex interplay of genetic, environmental, and psychological factors. Early experiences of neglect, overprotection, or inconsistent caregiving can contribute to the development of dependency patterns in adulthood.
Early attachment patterns
Children who experience inconsistent or overprotective caregiving may develop insecure attachment styles, leading to a heightened need for reassurance and dependence on others in adulthood. These individuals may learn to rely excessively on caregivers to provide for their emotional and physical needs, laying the foundation for dependent behaviors later in life. Moreover, a background of chronic illness during childhood or experiencing separation anxiety disorder increases the likelihood of developing dependent personality disorder.
Family
Family situations can shape how someone sees themselves and their ability to handle things alone. If parents are overly protective or strict, it might make someone feel like they can't do things without help. Also, if there's a history of anxiety disorders in the family, it can make someone more likely to feel anxious about being independent and rely on others for support.
Cultural factors
Cultural factors can also play a role in the development of DPD. Societies that emphasize collectivism and interdependence over individualism may inadvertently reinforce dependent behaviors. Individuals raised in such cultures may internalize the belief that seeking help and relying on others is unacceptable and expected, further perpetuating their dependency.
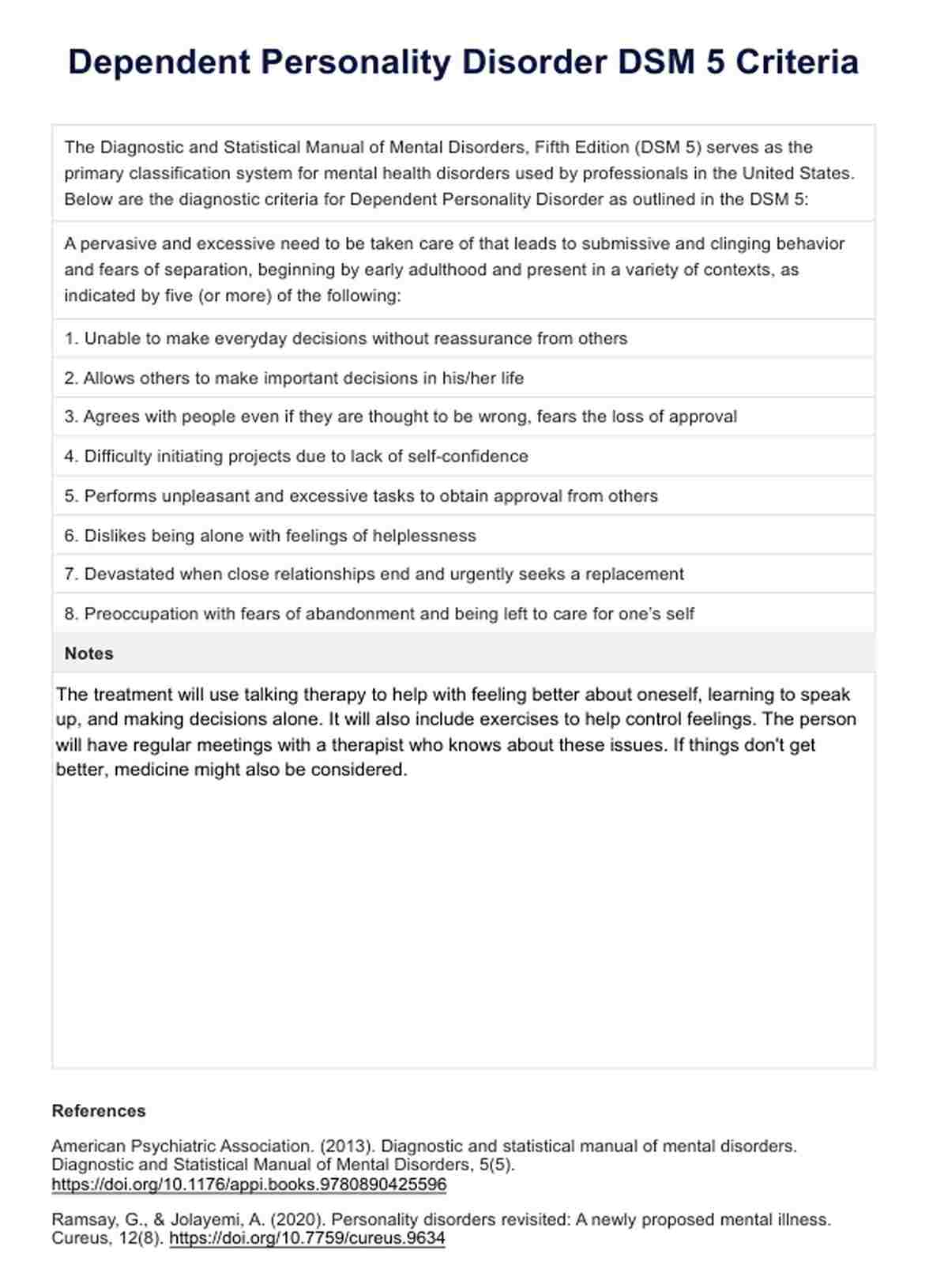
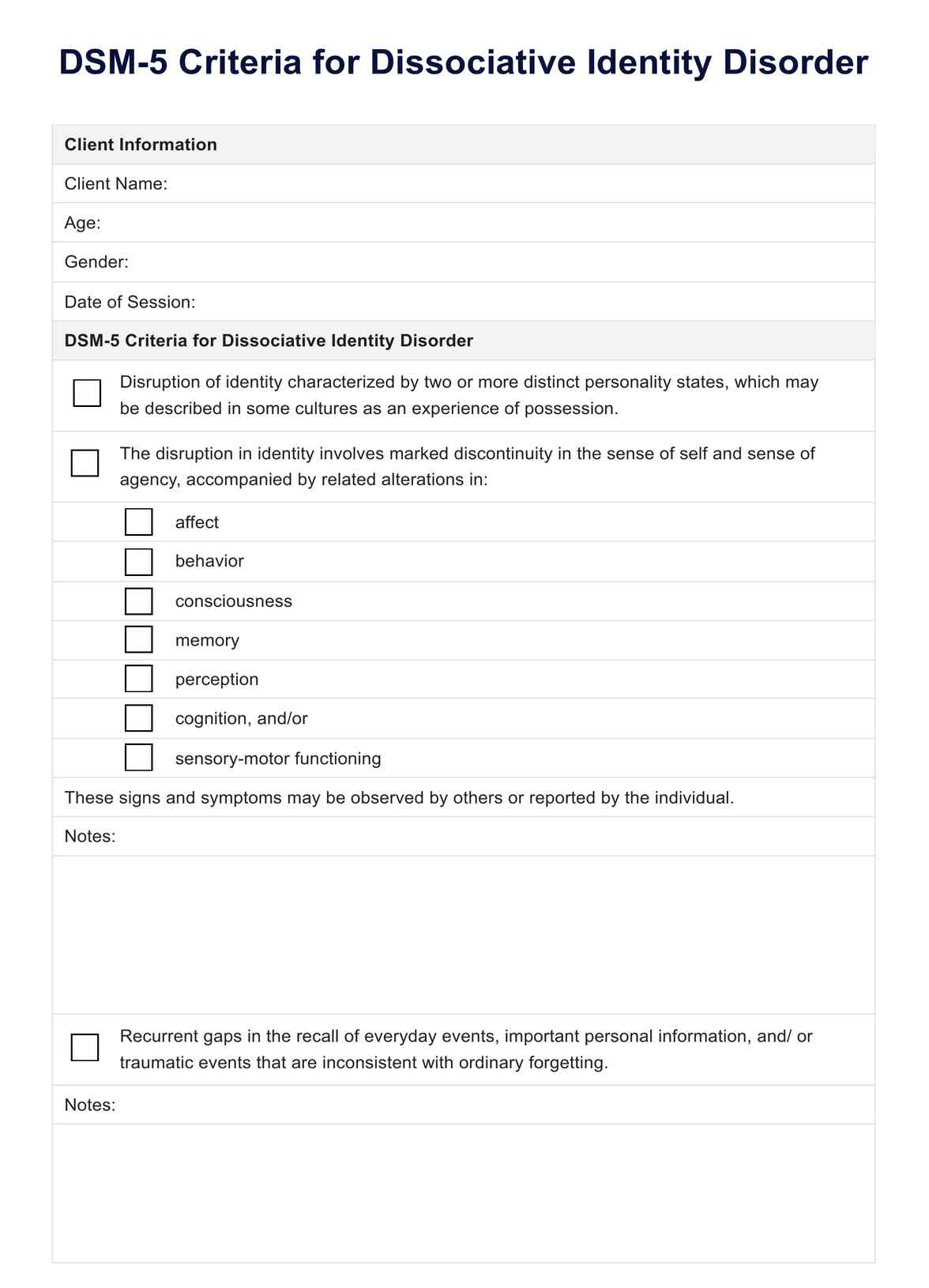
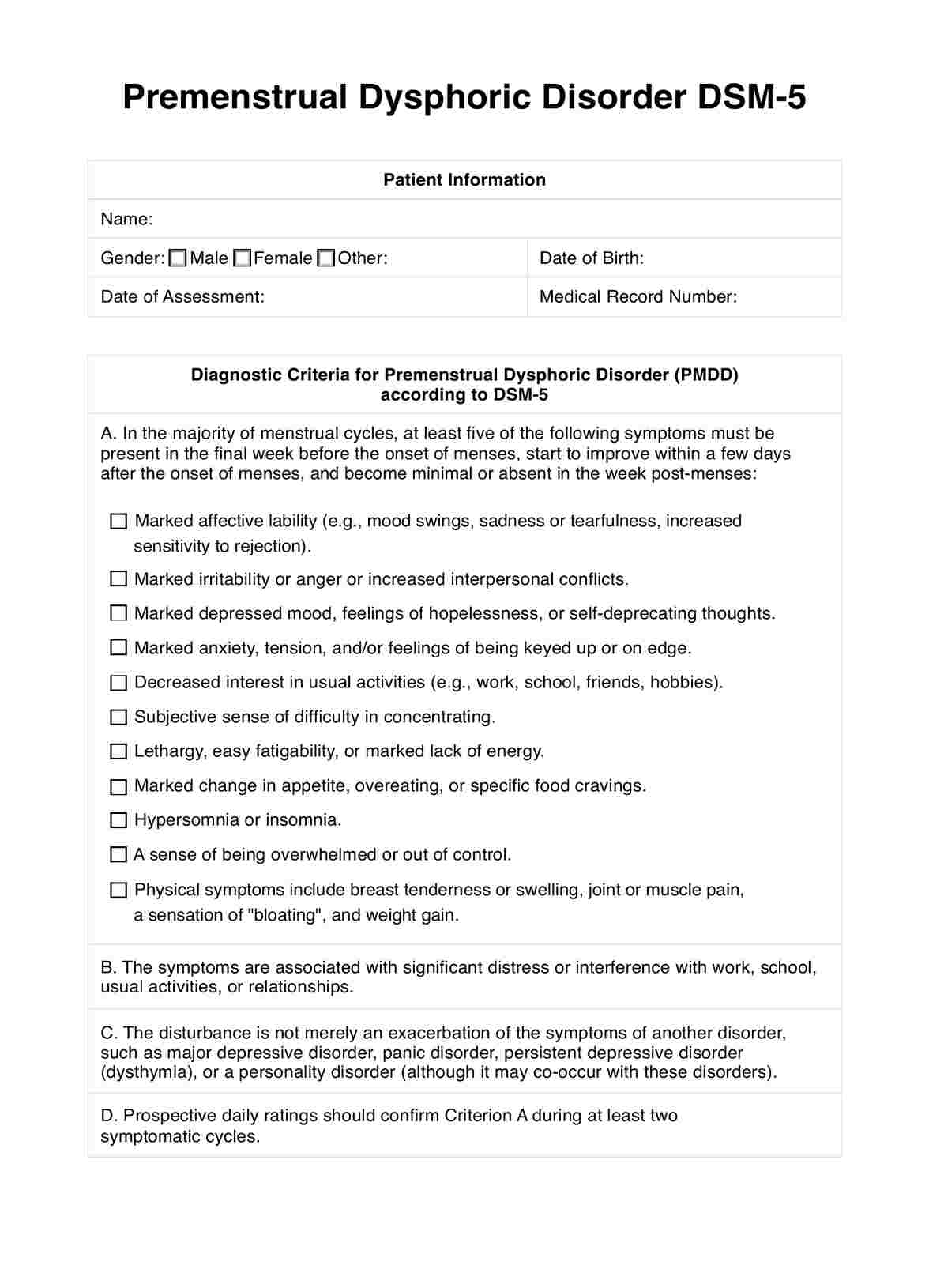
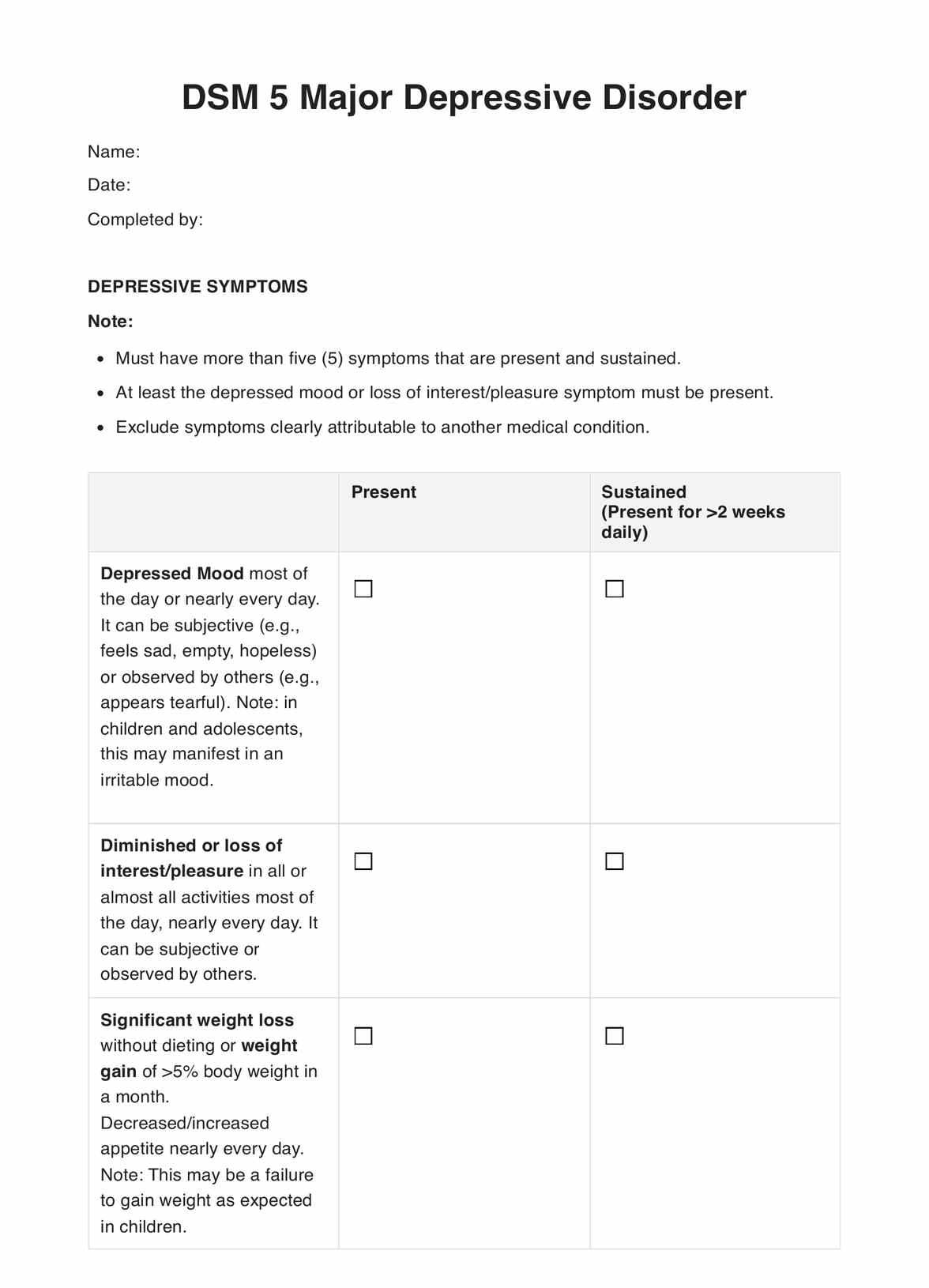
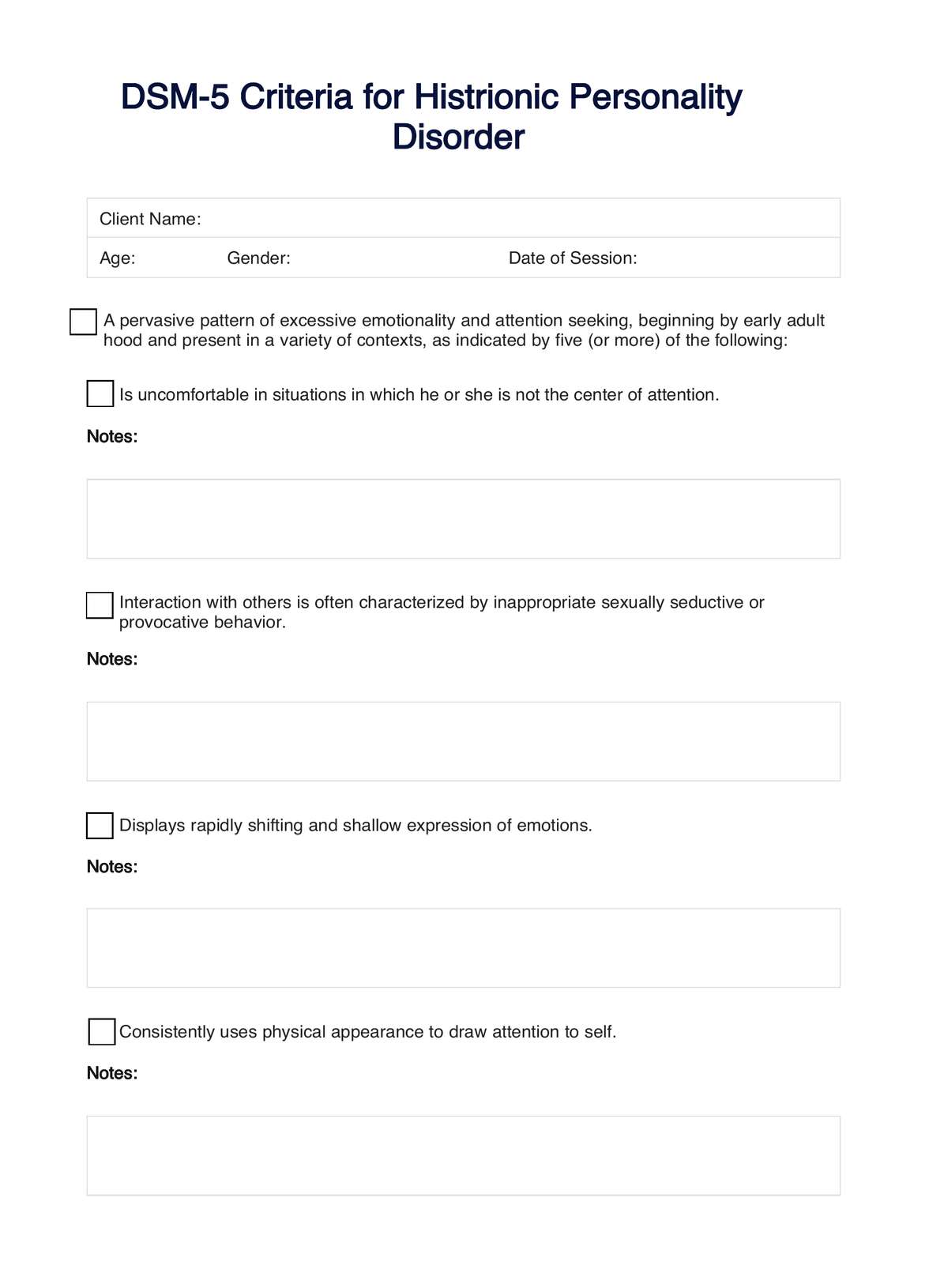
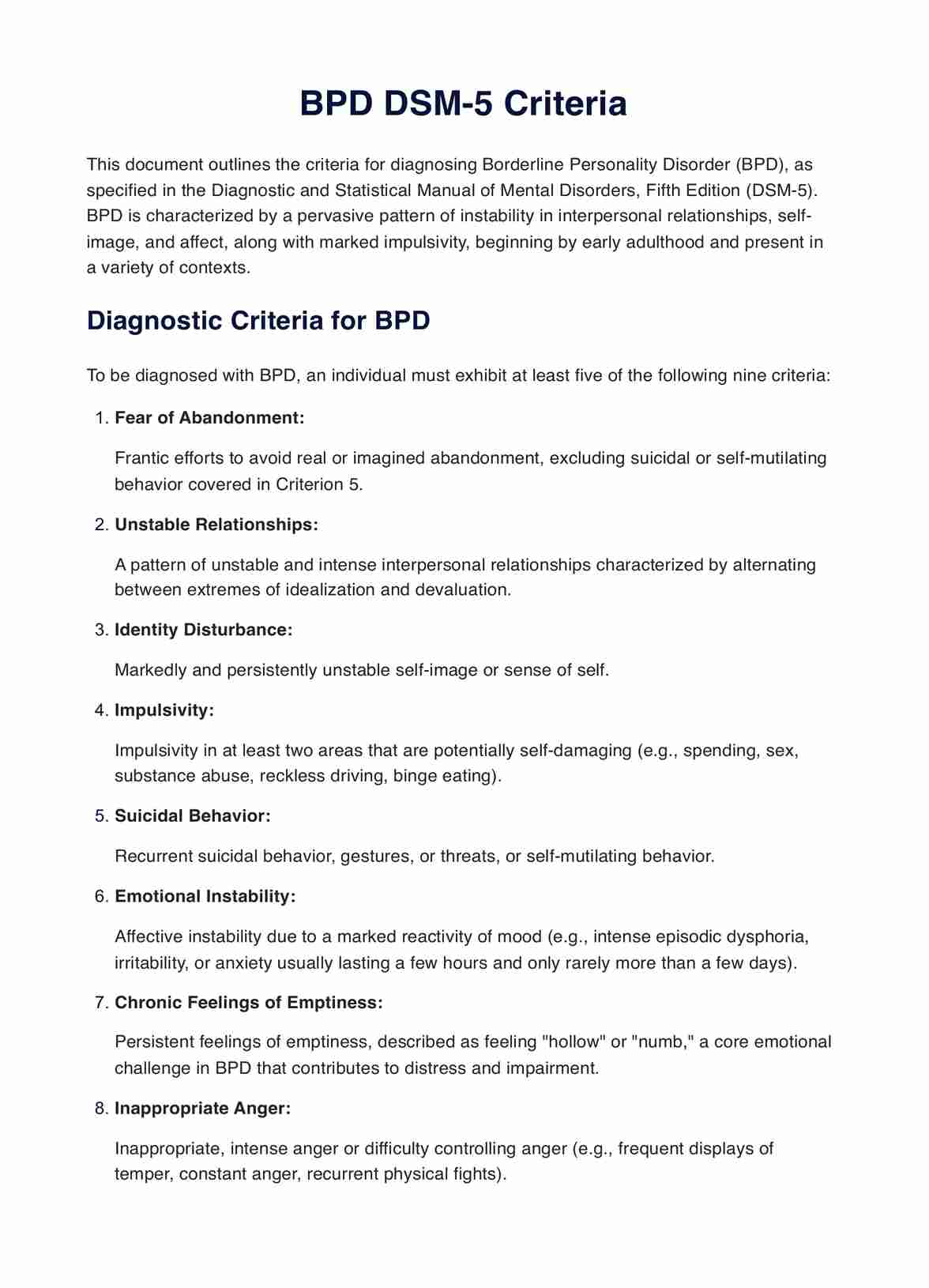
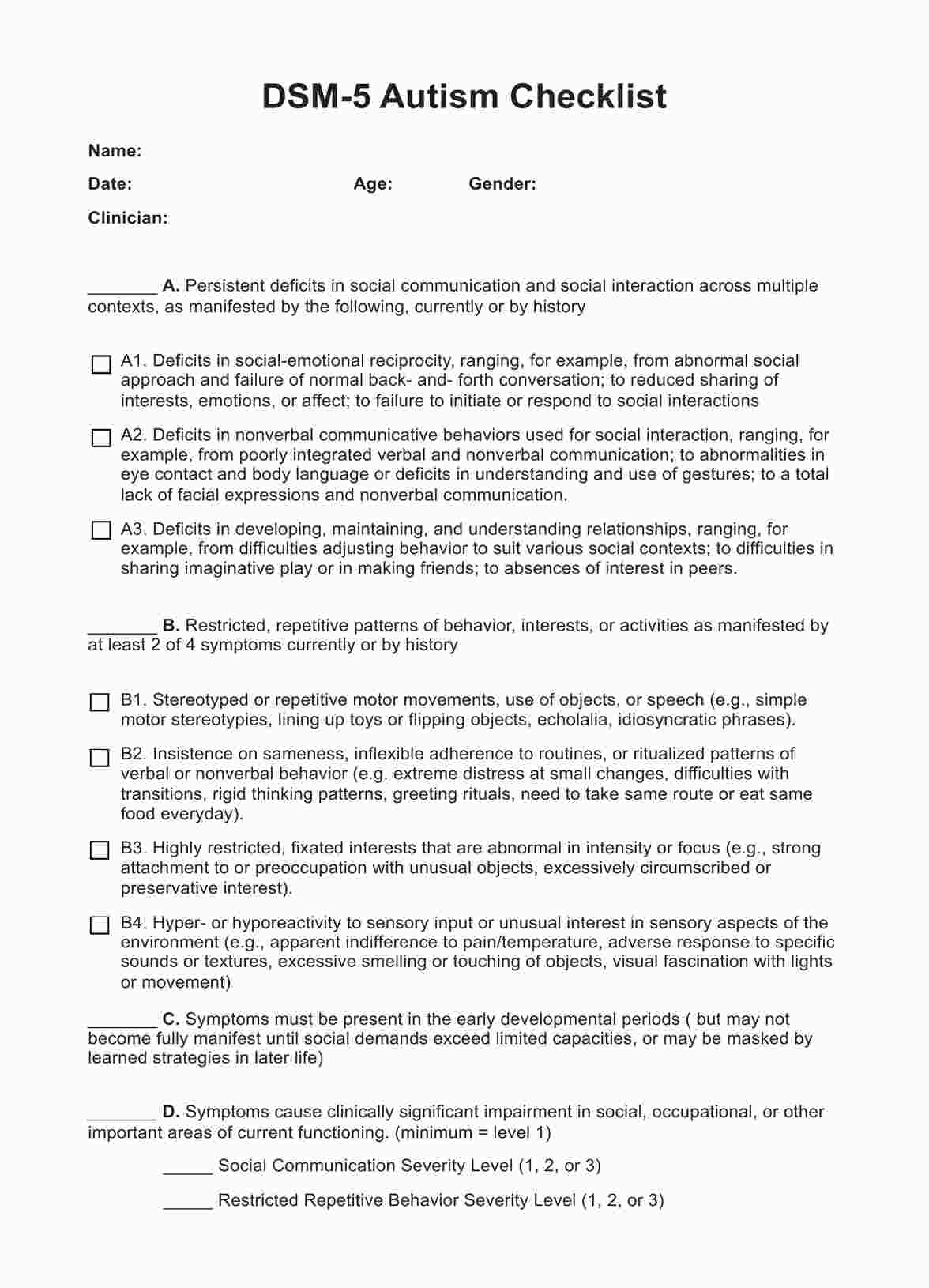
What are the DSM 5 criteria for DPD?
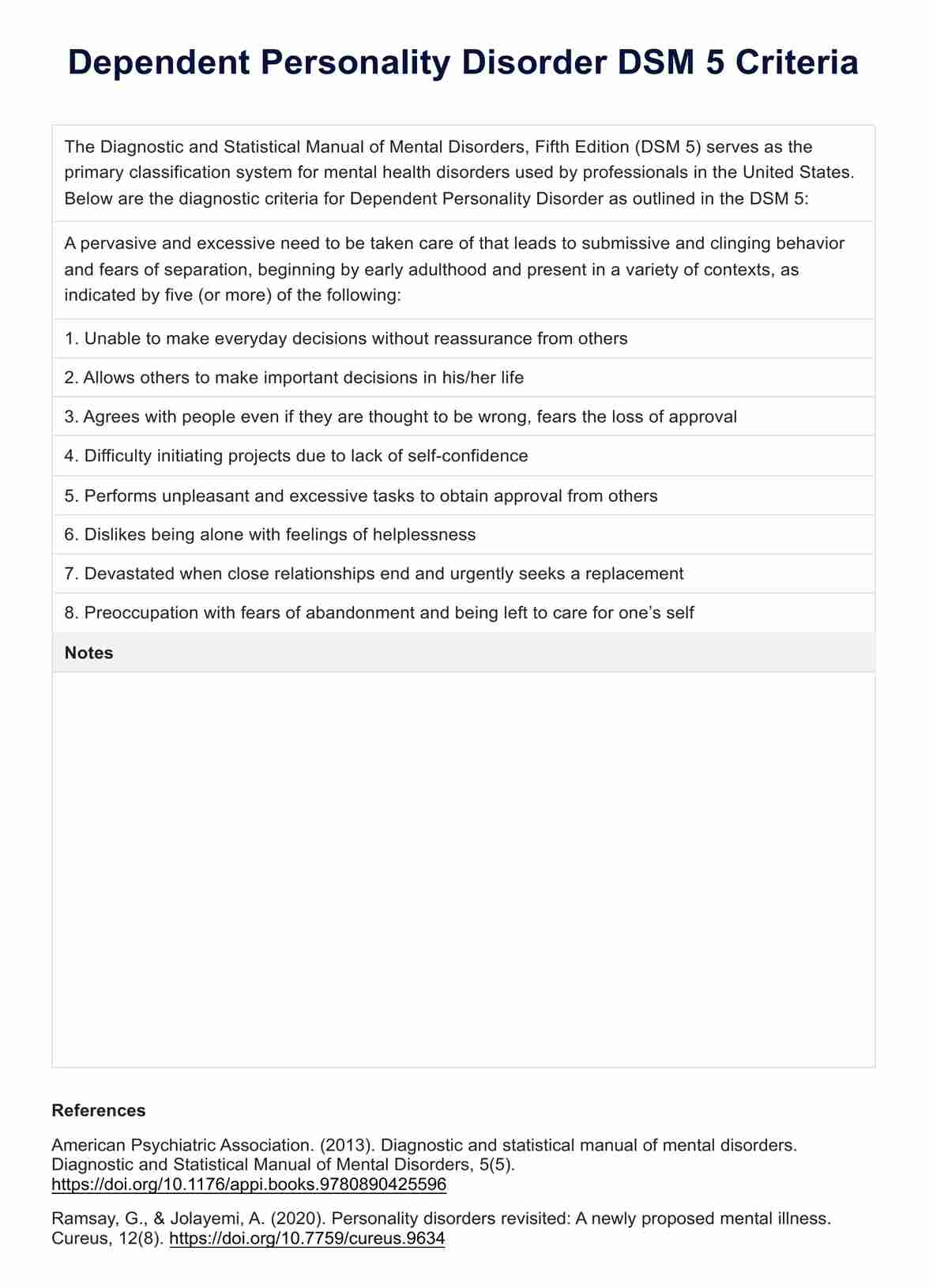
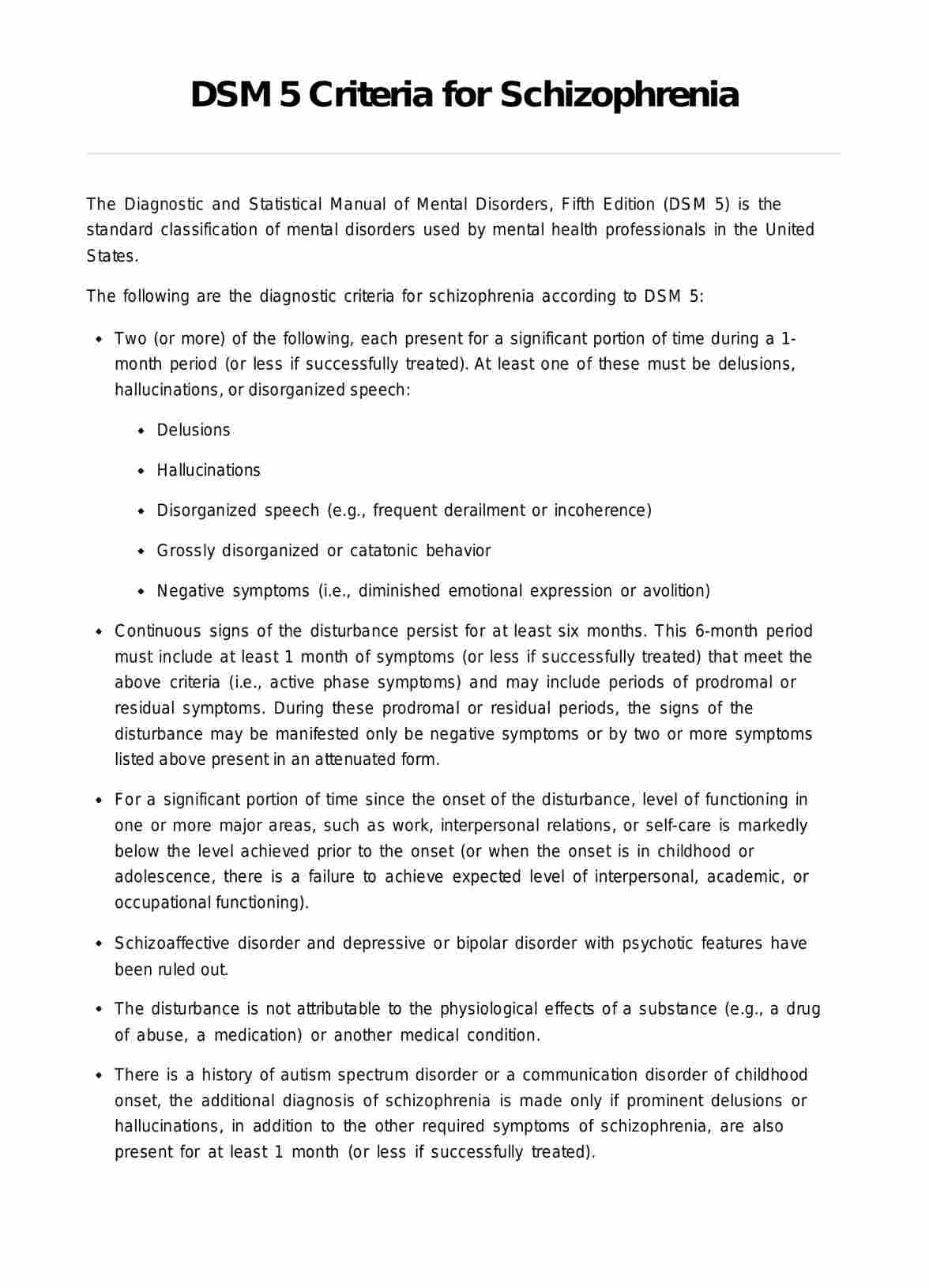
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), published by the American Psychiatric Association, is the primary classification tool for mental health disorders used by U.S. professionals. Here are the DSM-5 diagnostic criteria for Dependent Personality Disorder:
A pervasive and excessive need to be taken care of that leads to submissive and clinging behavior and fears of separation, beginning by early adulthood and present in a variety of contexts, as indicated by five (or more) of the following:
- Unable to make everyday decisions without reassurance from others
- Allows others to make important decisions in his/her life
- Agrees with people even if they are thought to be wrong, fears the loss of approval
- Difficulty initiating projects due to lack of self-confidence
- Performs unpleasant and excessive tasks to obtain approval from others
- Dislikes being alone with feelings of helplessness
- Devastated when close relationships end and urgently seeks a replacement
- Preoccupation with fears of abandonment and being left to care for one's self
How is DPD treated?
An in-depth understanding of Dependent Personality Disorder (DPD) is somewhat limited, with fewer studies and academic developments (Ramsay & Jolayemi, 2020). However, there are known therapeutic approaches that have shown promise in helping individuals with DPD manage their symptoms and improve their quality of life. Among these approaches are psychodynamic therapy and cognitive behavioral therapy (CBT):
Psychodynamic therapy
Psychodynamic therapy for Dependent Personality Disorder (DPD) focuses on exploring unconscious conflicts and past experiences that contribute to dependency patterns. Therapists help patients understand how early relationships and unresolved issues influence their current behavior, fostering insight and promoting healthier coping mechanisms. Through this process, individuals with DPD can develop greater autonomy and self-awareness, ultimately reducing dependency on others.
Cognitive behavioral therapy
Cognitive Behavioral Therapy (CBT) for DPD targets maladaptive thought patterns and behaviors associated with dependency. Therapists assist patients in identifying and challenging negative beliefs about themselves and their abilities, promoting self-confidence and assertiveness. CBT empowers individuals with DPD to gradually take on more responsibility and make independent decisions by teaching practical skills and problem-solving techniques, fostering greater autonomy and resilience.
References
American Psychiatric Association. (2013). Section I: DSM-5 basics introduction use of the manual cautionary statement for forensic use of DSM-5. https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/DSM/APA_DSM-5-Contents.pdf
Ramsay, G., & Jolayemi, A. (2020). Personality disorders revisited: A newly proposed mental illness. Cureus, 12(8). https://doi.org/10.7759/cureus.9634
Zimmerman, M. (2023, September). Dependent personality disorder - mental health disorders. MSD Manual Consumer Version. https://www.msdmanuals.com/home/mental-health-disorders/personality-disorders/dependent-personality-disorder
Commonly asked questions
Individuals with DPD often display clingy behavior, reluctance to make decisions without reassurance, and an excessive need to be cared for by others.
DPD can hinder one's capacity to take initiative and responsibility for one's actions or decisions due to pervasive psychological dependence on others for guidance and support.
Yes, therapy facilitated by mental health professionals can be highly beneficial in addressing the underlying fears and insecurities driving dependency, empowering individuals to take more responsibility for their own lives and decisions gradually.




















-template.jpg)