BPD DSM-5 Criteria PDF
Simplify mental health practice management with Carepatron. Secure, easy-to-use software for telehealth, documentation, and collaboration.


What is borderline personality disorder?
Borderline Personality Disorder (BPD) stands as a multifaceted mental disorder defined by a pervasive pattern of instability in interpersonal relationships, self-image, and emotions. Individuals with BPD navigate through life with a persistently unstable self-image and experience chronic feelings of emptiness.
This condition is marked by intense emotional episodes, including anger, depression, and anxiety, varying in duration from a few hours to several days. The core of BPD involves a deep-seated fear of real or imagined abandonment, prompting individuals to make frantic efforts to avoid being left alone.
As a subset of personality disorders, BPD reflects a complex interplay of mental disorders characterized by these persistent patterns and emotional turmoil.
Characteristics of a person with borderline personality disorder
Individuals with BPD exhibit a range of symptoms that significantly impact their ability to function in everyday life. These include:
- Chronic feelings of emptiness and boredom.
- Difficulty controlling anger leads to frequent temper displays or recurrent physical fights.
- Intense and unstable interpersonal relationships characterized by alternating between extremes of idealization and devaluation.
- Impulsivity in areas that are potentially self-damaging, such as binge eating, substance abuse, and reckless driving.
- Recurrent suicidal behavior, gestures, threats, or self-mutilating behavior.
What problems can this personality disorder lead to if left unmanaged?
If left unmanaged, BPD can lead to numerous problems, including severe interpersonal conflicts, job losses, and academic failures due to impulsivity and intense emotional reactions. Substance abuse, depression, and anxiety disorders are common comorbidities, complicating the treatment landscape. Moreover, individuals with BPD are at a higher risk for suicide.
BPD DSM-5 Criteria PDF Template
BPD DSM-5 Criteria PDF Example
How do mental healthcare professionals diagnose this disorder?
Diagnosing Borderline Personality Disorder (BPD) is a meticulous process that mental health professionals undertake with precision and sensitivity. Here is a step-by-step overview of how this complex disorder is diagnosed based on the criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5):
Step 1: Initial consultation
The process begins with an in-depth interview to gather a comprehensive history of the patient, including their current symptoms, life circumstances, medical history, and any previous mental health diagnoses or treatments.
Step 2: Symptom assessment
The mental health professional explores the range and intensity of symptoms the patient experiences, focusing on patterns of instability in relationships, self-image, and emotions, as well as instances of marked impulsivity. Questionnaires and psychological tests may be used to systematically assess symptoms and their impact on the patient’s life. These tools help differentiate BPD from other similar mental health conditions.
Step 3: Criteria matching
The professional reviews the specific criteria for BPD outlined in the DSM-5. A diagnosis of BPD requires that at least five of the nine criteria be met. These include patterns of unstable interpersonal relationships, identity disturbance, impulsivity, suicidal behavior, emotional instability, chronic feelings of emptiness, intense anger, transient, stress-related paranoid thoughts, or severe dissociative symptoms.
Step 4: Differential diagnosis
Distinguishing Borderline Personality Disorder (BPD) from other mental health disorders is a nuanced process that is essential for accurate diagnosis and effective treatment planning. The overlap of symptoms between BPD and disorders such as mood disorders, other personality disorders, and symptoms resulting from substance abuse requires a thorough evaluation. This evaluation entails an in-depth analysis of the patient's history, symptoms' manifestation, and consistency across various contexts.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR), it is recognized that BPD can co-occur with several other disorders. Importantly, if the diagnostic criteria for BPD and another disorder are both met, concurrent diagnoses should be made. This underscores the complexity of mental health disorders and the importance of a comprehensive assessment by a healthcare professional.
In the differential diagnosis phase, it's critical to consider the full spectrum of mental health disorders, acknowledging the possibility of comorbidities, to tailor an appropriate and effective treatment plan for the individual.
Step 5: Assessing functioning and impact
The clinician assesses how BPD symptoms affect the patient's life, including relationships, work, and personal well-being. This helps to understand the severity and pervasiveness of the disorder.
Step 6: Consideration of context
Cultural, familial, and social backgrounds ensure that the diagnosis accurately reflects the individual's experiences and not just the presence of symptoms.
Step 7: Collaborative diagnosis
Diagnosis is a collaborative effort between the patient and the mental health professional. It involves open communication, with the professional explaining and clarifying the diagnostic process and criteria for borderline patients.
Step 8: Diagnosis and discussion
If the patient meets the criteria for BPD, the mental health professional will make the diagnosis and discuss it with the patient. This discussion includes an explanation of the disorder, its symptoms, and the criteria met.
Step 9: Treatment planning
Following the diagnosis, the professional and patient develop a comprehensive treatment plan. This plan may include psychotherapy, medication, and other support services tailored to the individual’s needs.
By following these steps, mental health professionals ensure that the diagnosis of BPD is accurate, comprehensive, and tailored to the individual’s unique circumstances. This careful process lays the groundwork for effective treatment and management of the disorder, providing hope and direction for those affected by BPD.
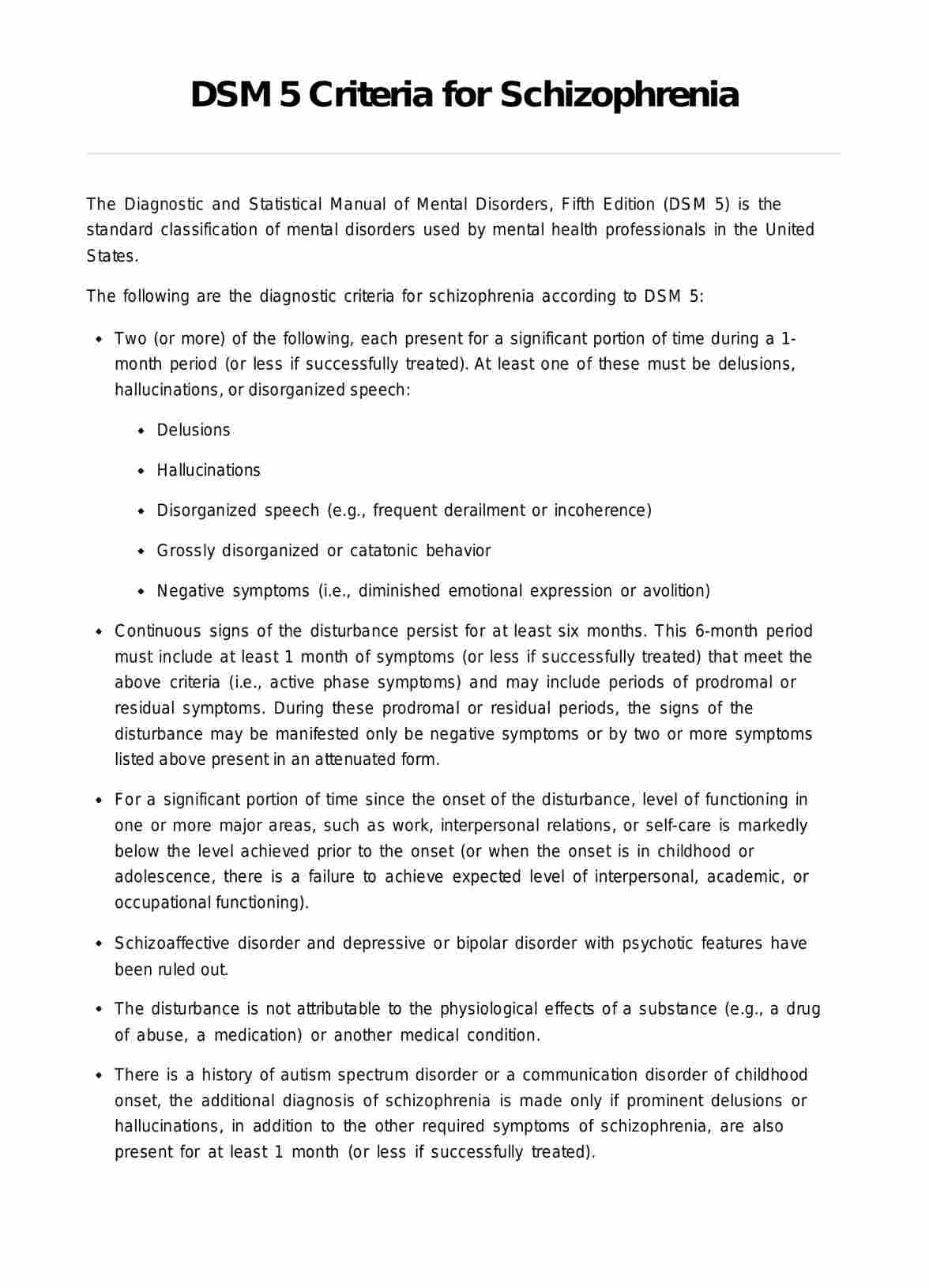
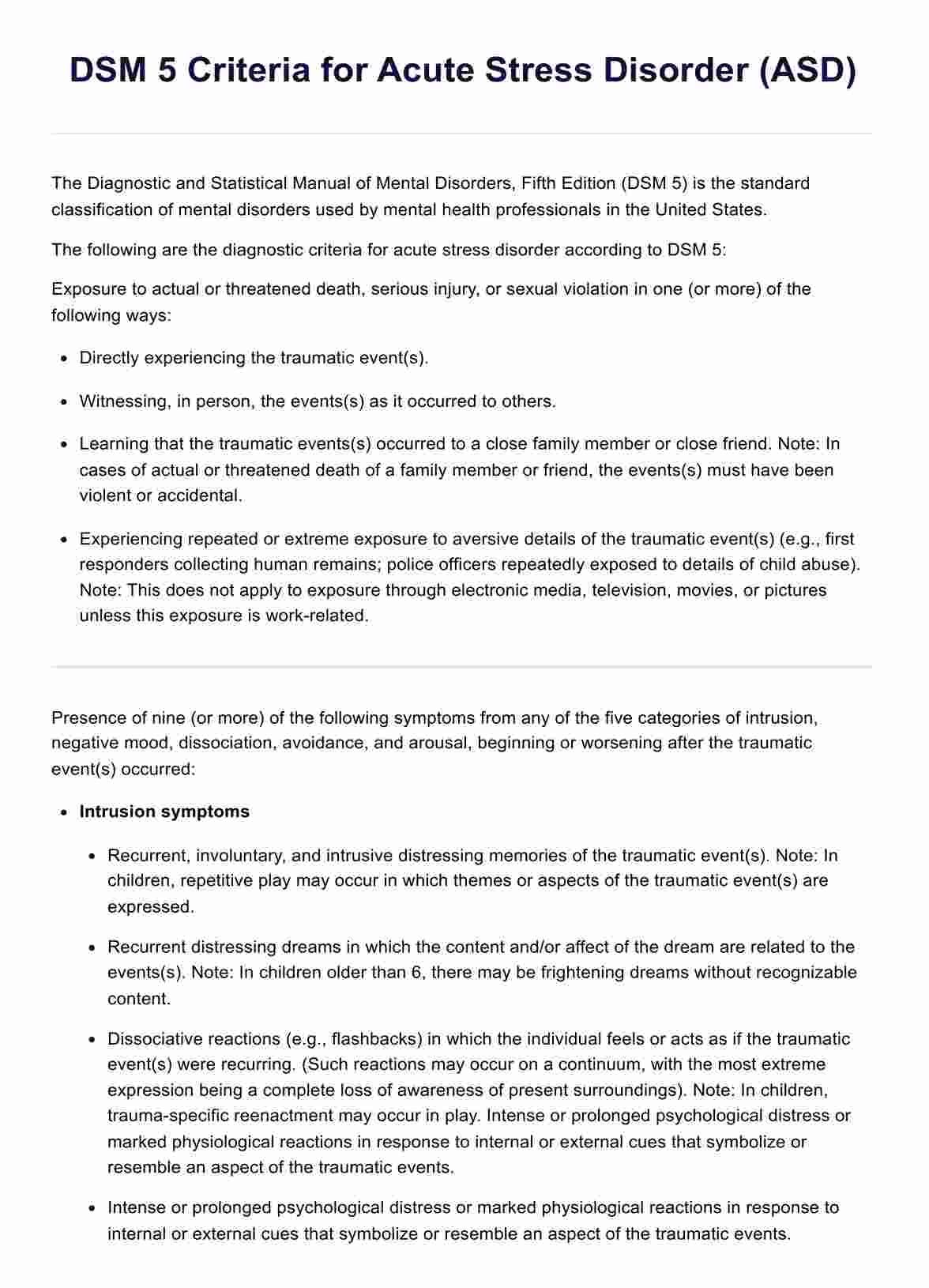
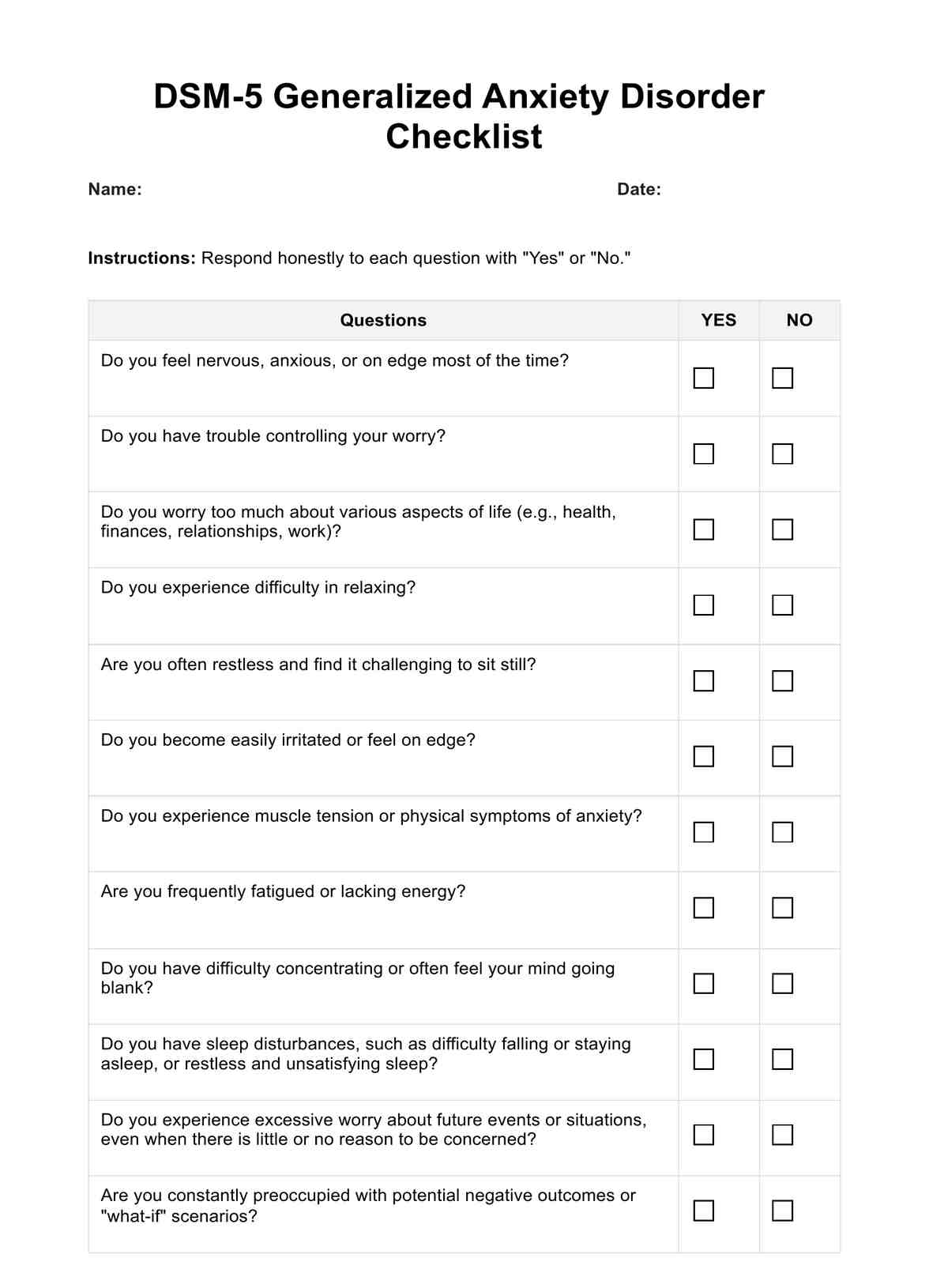
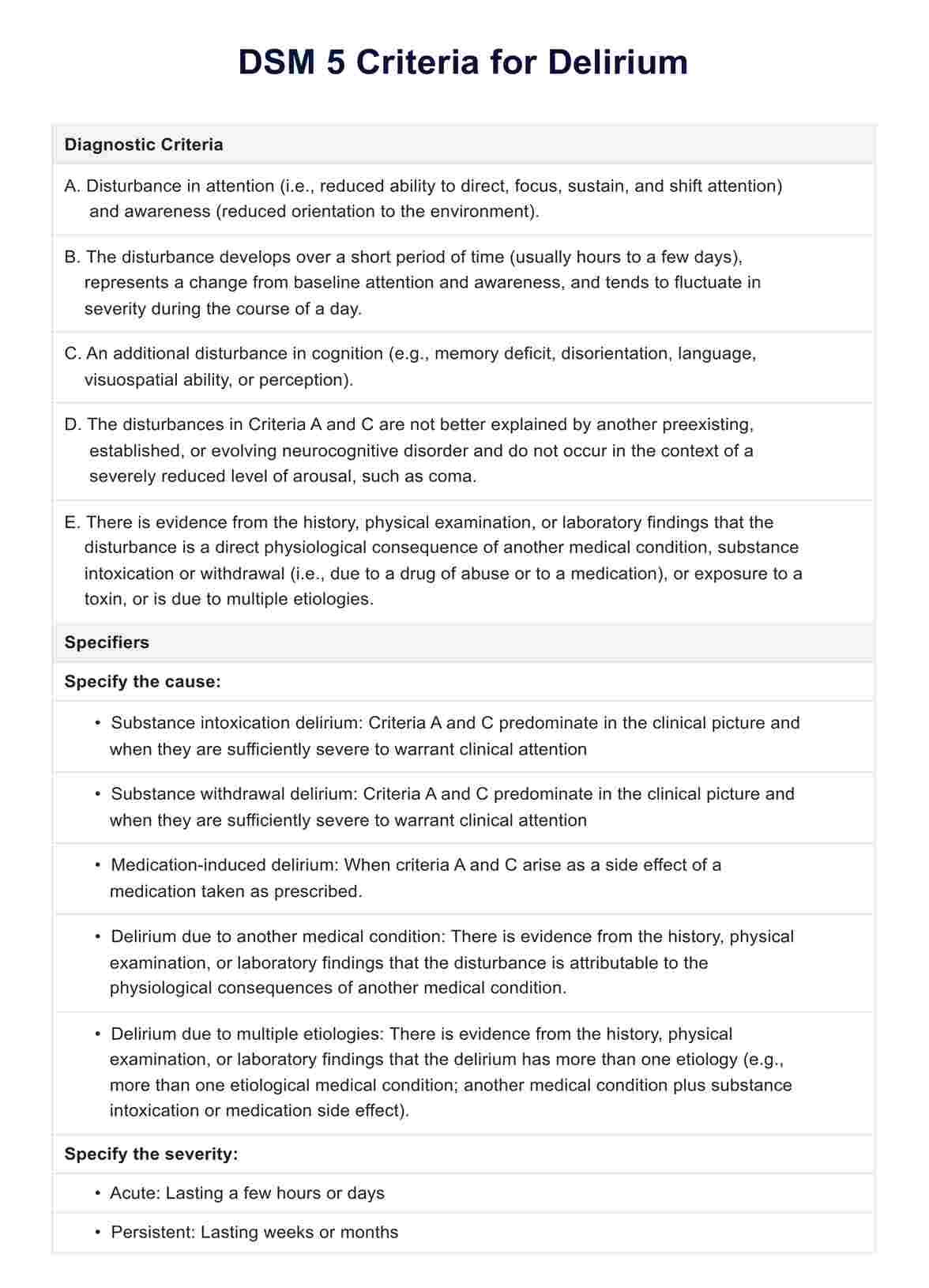
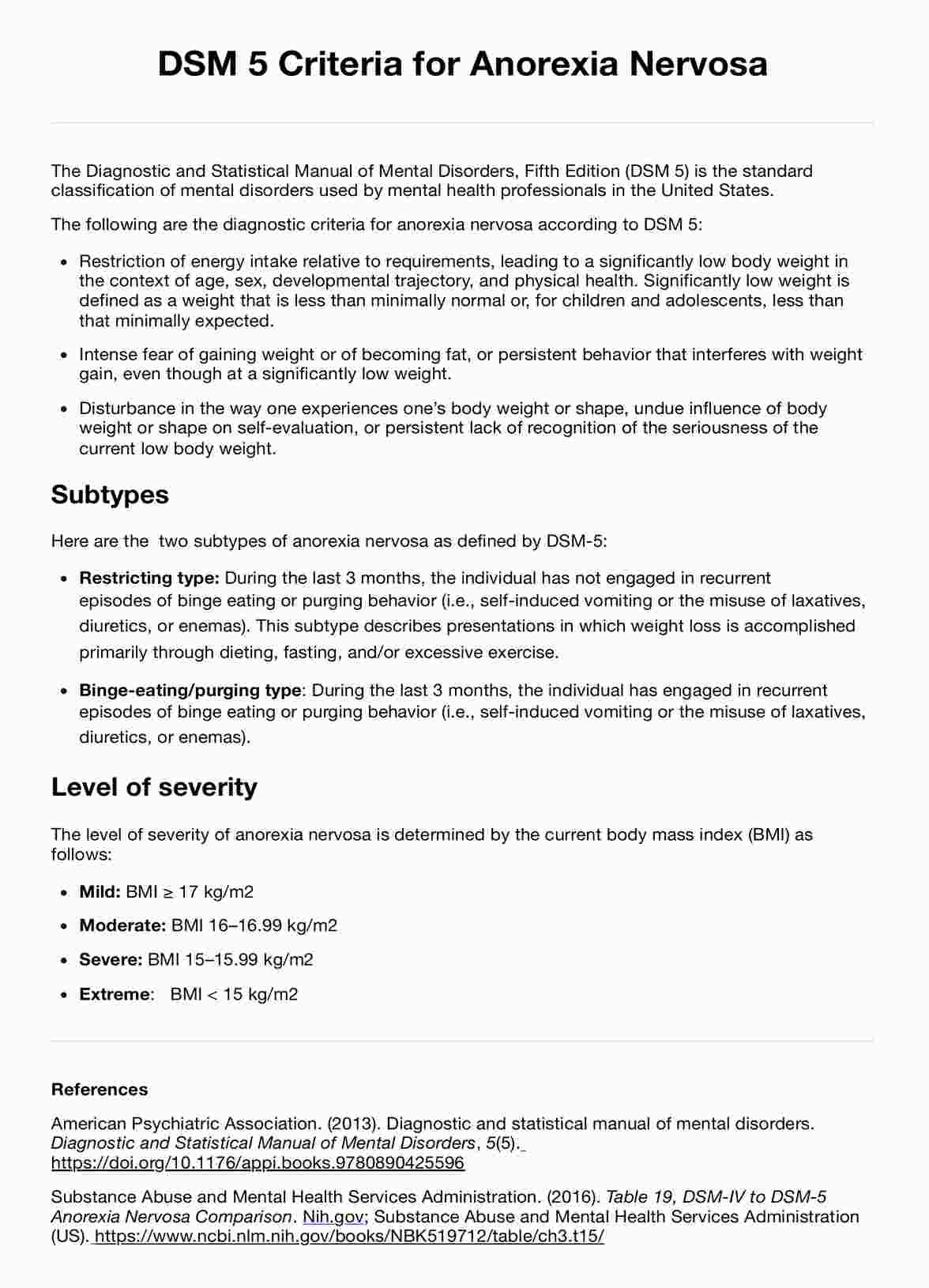
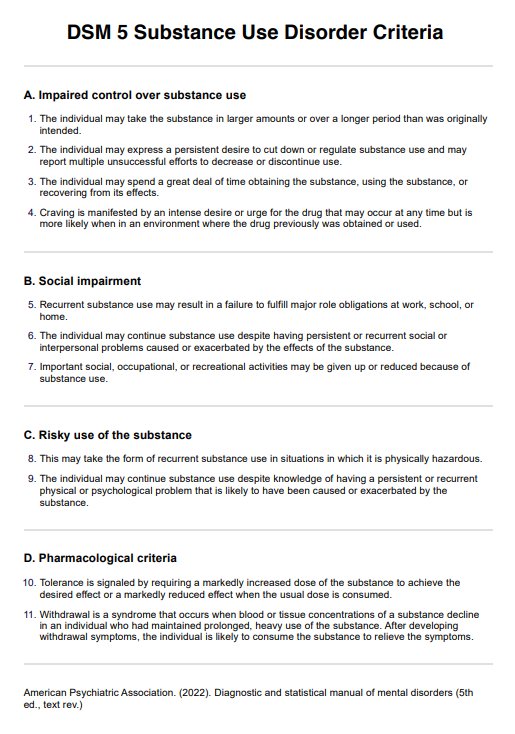
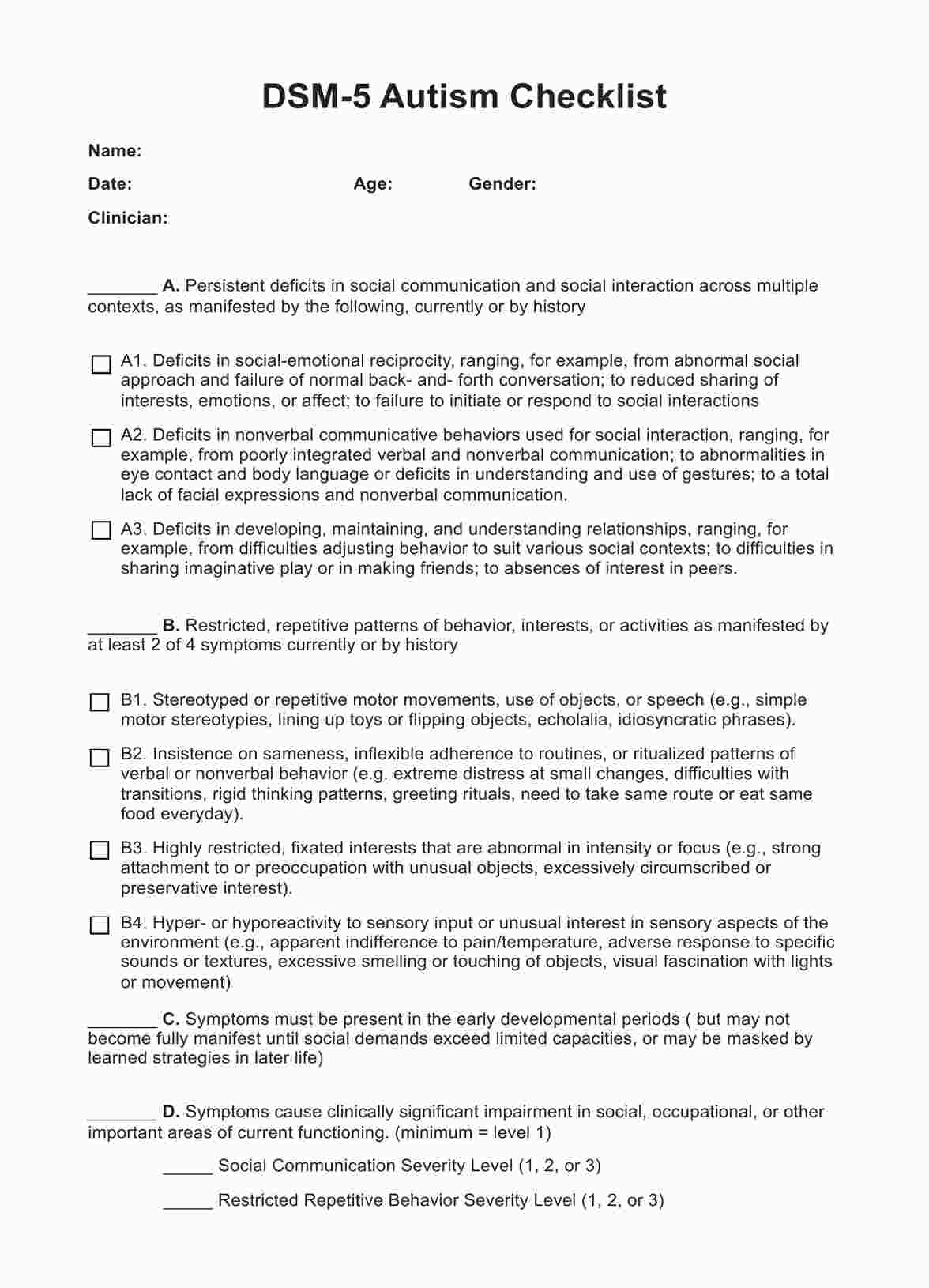
What is the DSM-5?
The DSM-5, the latest edition of the Diagnostic and Statistical Manual of Mental Disorders, is a handbook used by healthcare professionals as a guide to diagnosing mental disorders. It outlines specific criteria for each disorder, including BPD, facilitating an accurate diagnosis and informing treatment plans.
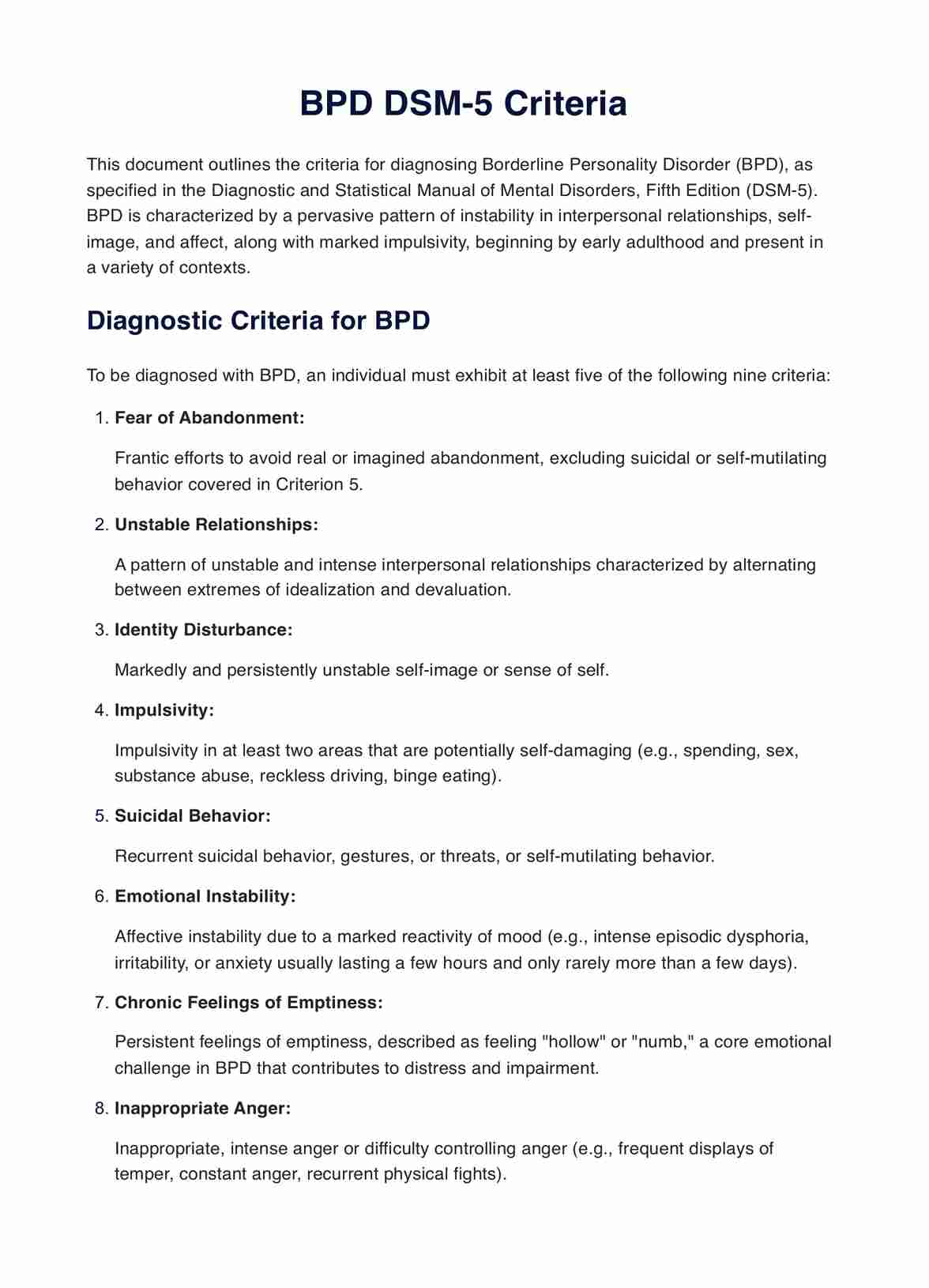
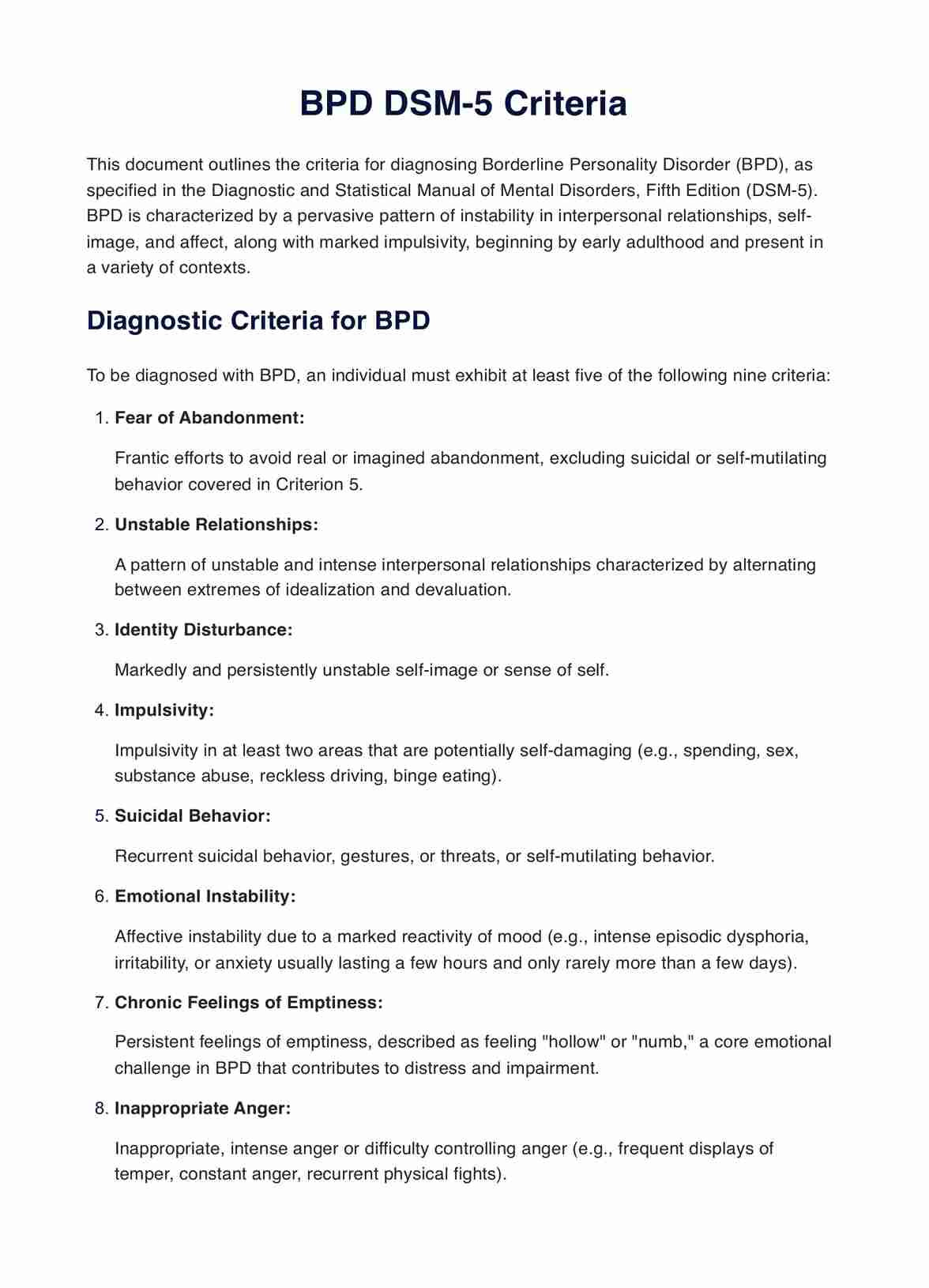
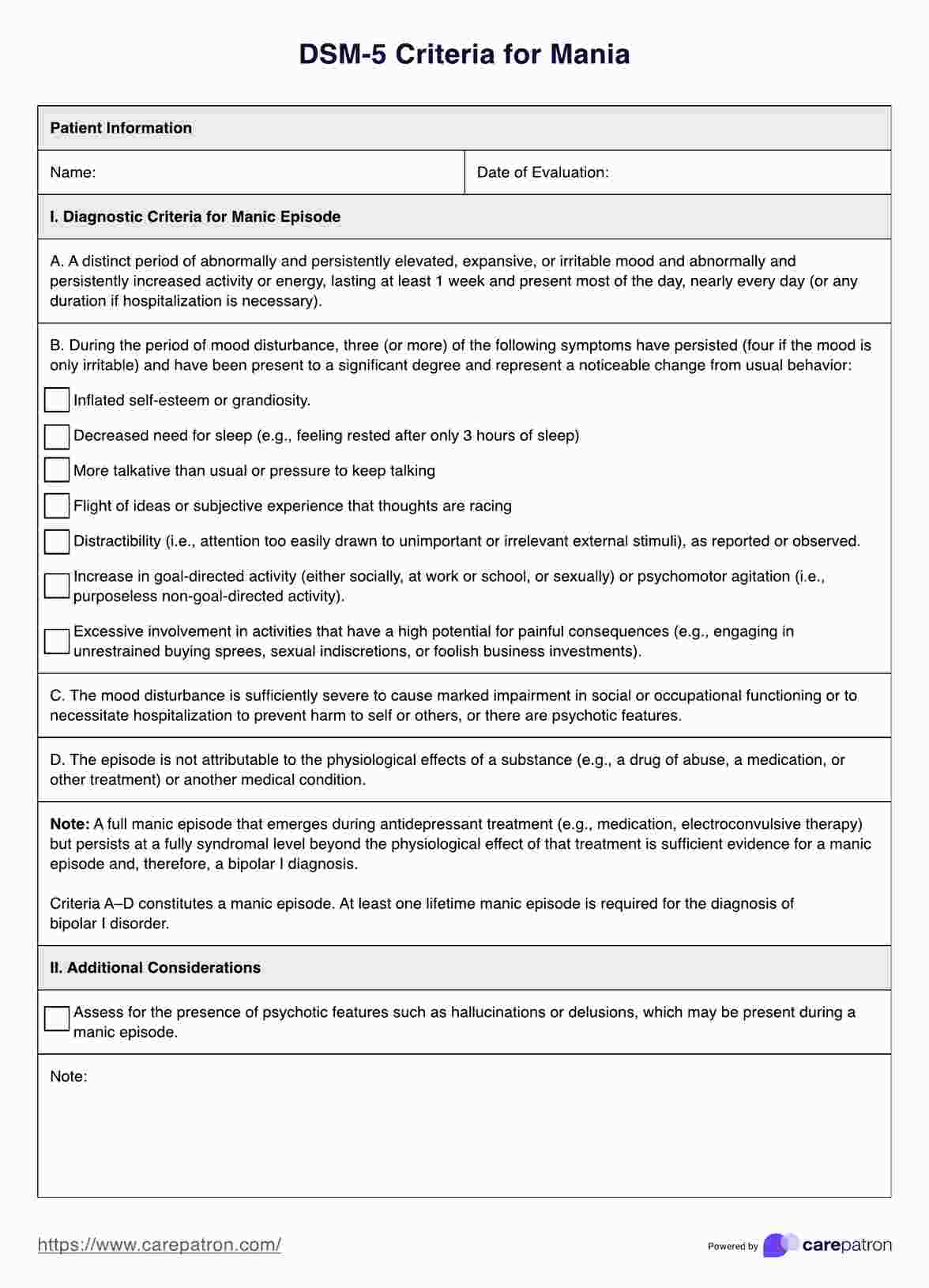
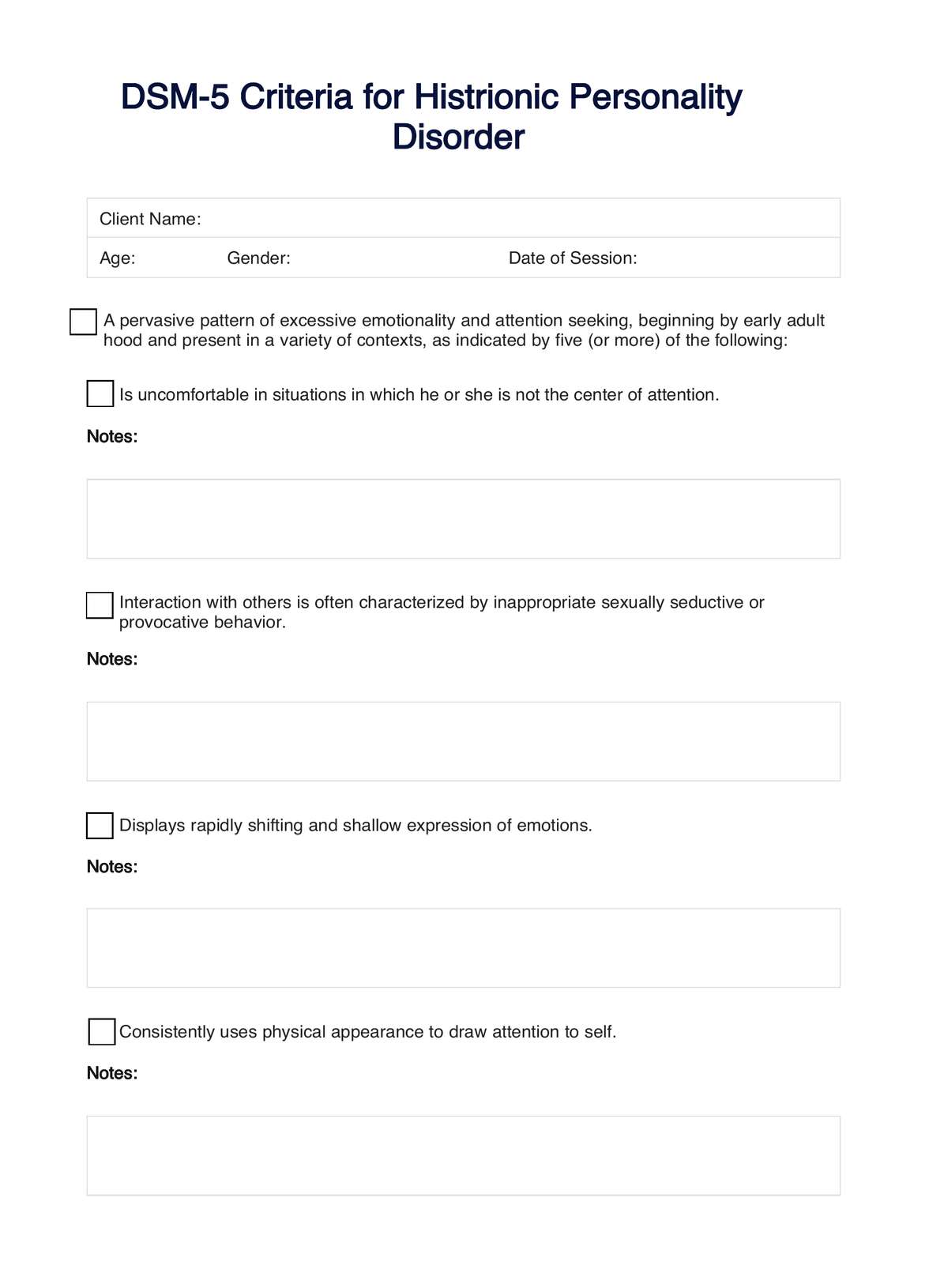
What is the DSM-5's criteria for borderline personality disorder?
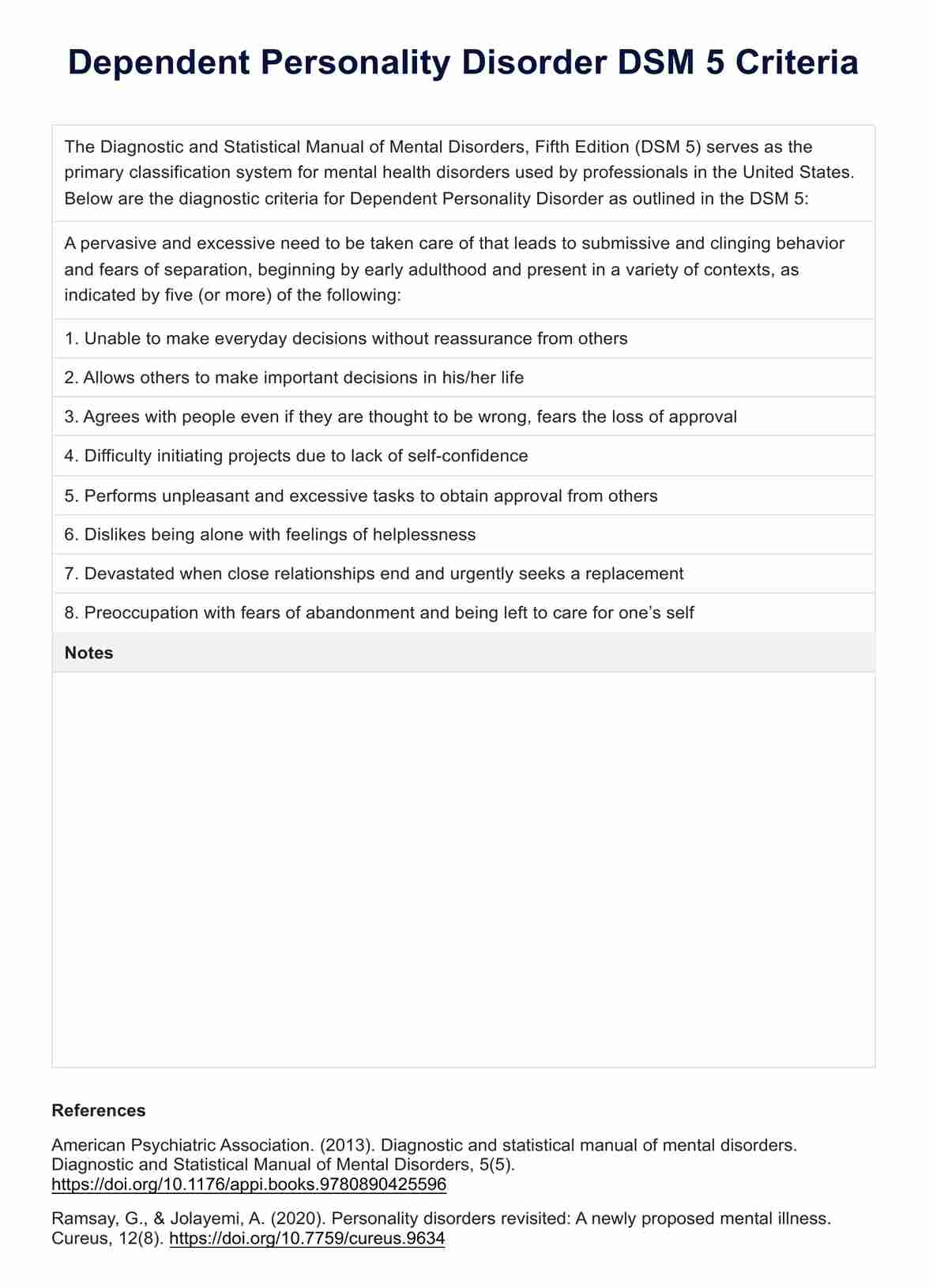
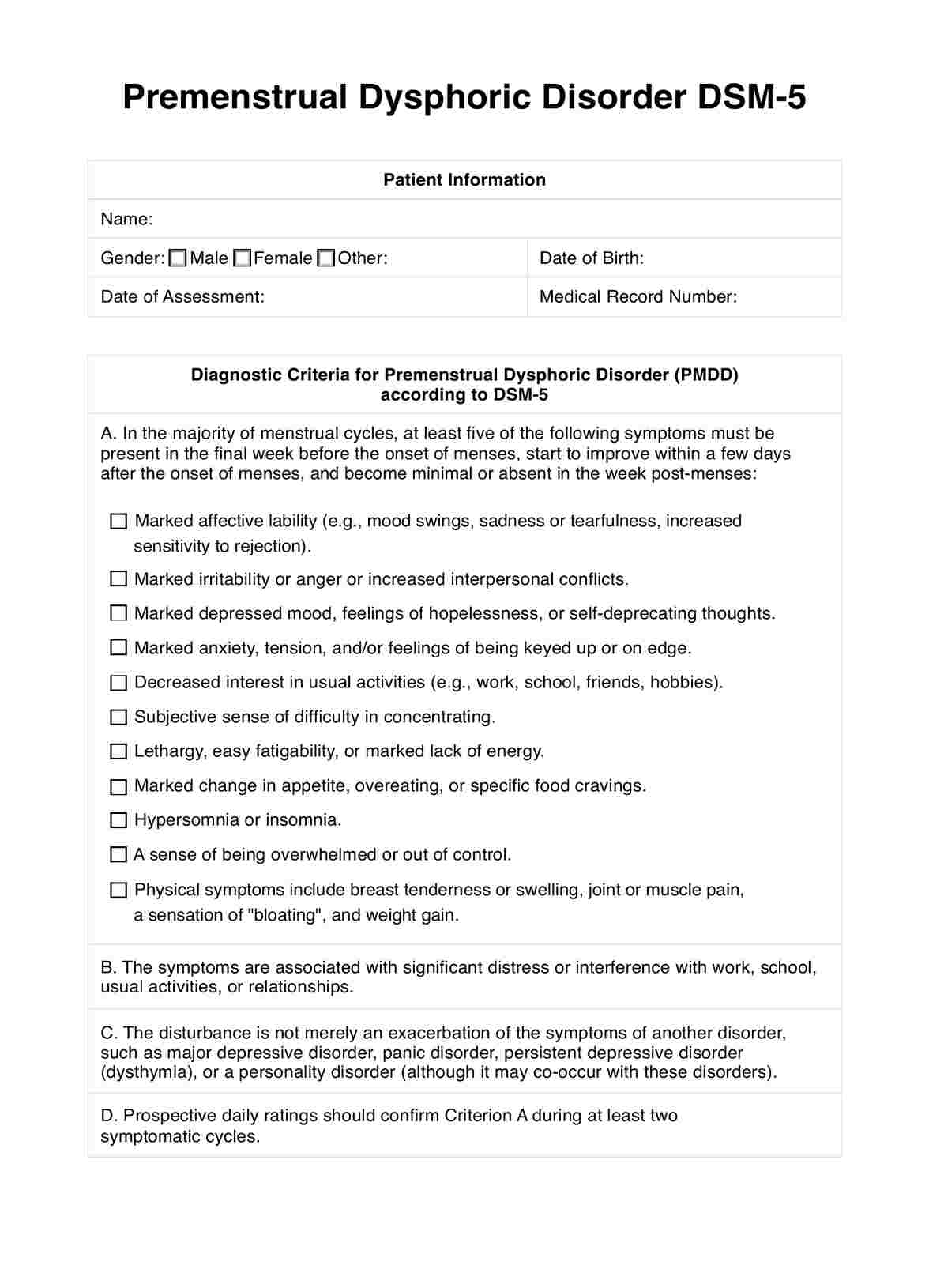
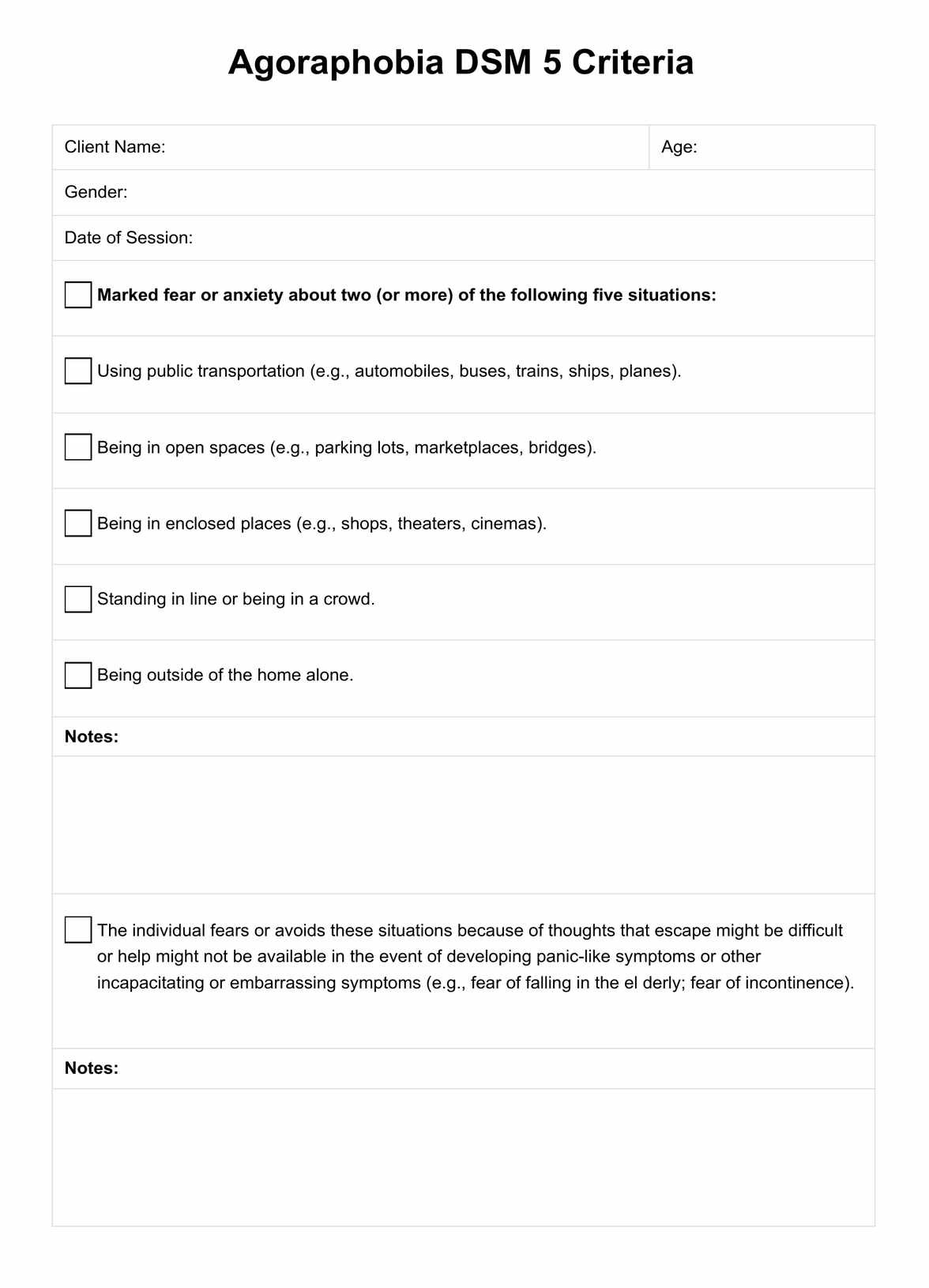
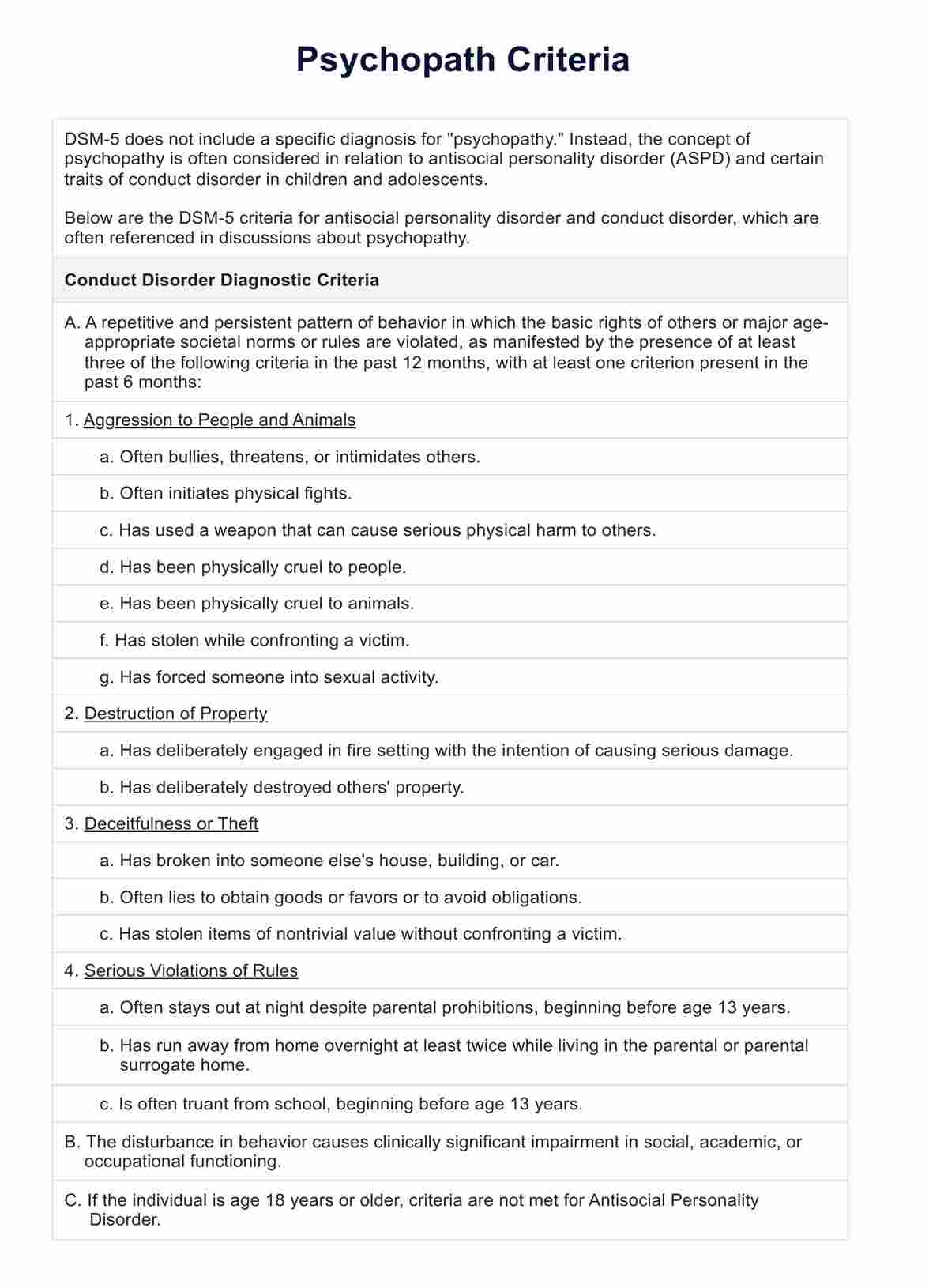
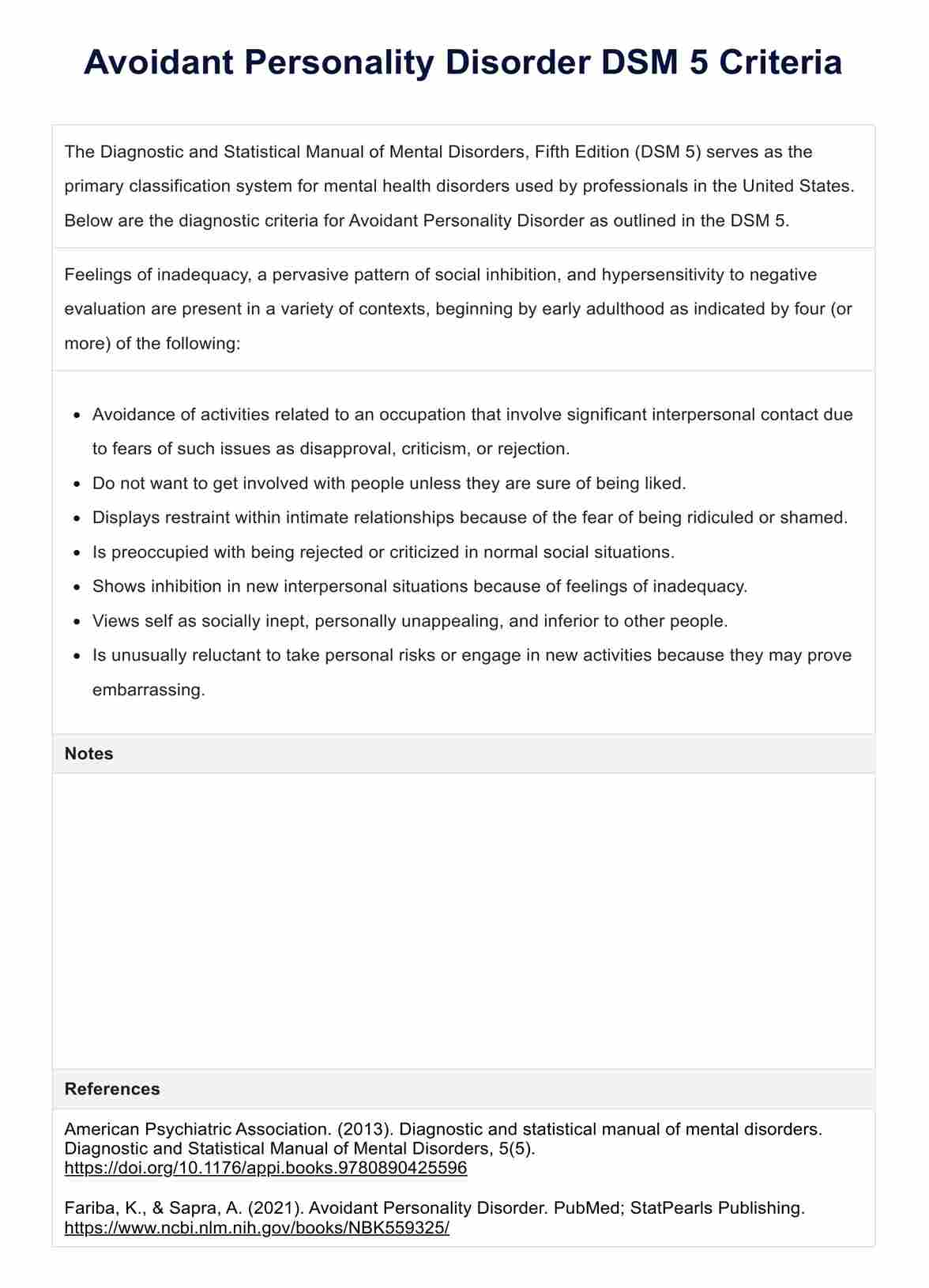
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) specifies criteria for diagnosing Borderline Personality Disorder (BPD), emphasizing a pervasive pattern of instability in interpersonal relationships, self-image, and affects, as well as marked impulsivity. This pattern begins in early adulthood and is present across various contexts. For a diagnosis of BPD, at least five of the following nine criteria must be met:
- Frantic efforts to avoid real or imagined abandonment. Note: This does not include suicidal or self-mutilating behavior considered in criterion 5.
- A pattern of unstable and intense interpersonal relationships characterized by alternating between extremes of idealization and devaluation.
- Identity disturbance: markedly and persistently unstable self-image or sense of self.
- Impulsivity in at least two areas that are potentially self-damaging (e.g., spending, sex, substance abuse, reckless driving, binge eating). Note: Do not include suicidal or self-mutilating behavior covered in criterion 5.
- Recurrent suicidal behavior, gestures, threats, or self-mutilating behavior.
- Affective instability due to a marked reactivity of mood (e.g., intense episodic dysphoria, irritability, or anxiety usually lasting a few hours and only rarely more than a few days).
- Chronic feelings of emptiness.
- Inappropriate, intense anger or difficulty controlling anger (e.g., frequent displays of temper, constant anger, recurrent physical fights).
- Transient, stress-related paranoid ideation or severe dissociative symptoms.
These criteria, as outlined in the DSM-5, are crucial for a thorough and accurate diagnosis of Borderline Personality Disorder, underscoring the importance of adhering closely to this diagnostic framework to ensure the integrity of the diagnosis and subsequent treatment planning.
How does this BPD DSM-5 Criteria PDF work?
Our BPD DSM-5 Criteria PDF is a tool designed to help clinicians and patients understand the diagnostic criteria set forth by the DSM-5. It breaks down the complex language of the manual into more accessible terms, provides examples of how each criterion may present in real life, and offers a template for mental health professionals to assess their patients against these benchmarks.
What are the benefits of using this template?
The BPD DSM-5 Criteria PDF template stands as a pivotal tool in the realm of mental health diagnostics, offering a multitude of benefits for both clinicians and individuals seeking insight into Borderline Personality Disorder. Here are some of the key advantages of utilizing this template:
- Streamlines the diagnostic process: The template serves as a structured guide for mental health professionals, ensuring no critical diagnostic criterion is overlooked. This systematic approach is vital for evaluating BPD's complex and often overlapping symptoms, thereby facilitating a more efficient and thorough assessment process.
- Enhances diagnostic accuracy: By providing a clear and detailed breakdown of each DSM-5 criterion, the template helps minimize subjective interpretation and potential oversight. This contributes significantly to diagnostic accuracy, the cornerstone of formulating an effective treatment strategy. Accurate diagnosis leads to targeted interventions that address the specific needs of the individual, improving the overall outcome of therapeutic interventions.
- Educational resource: For patients and their loved ones, the template demystifies the criteria for BPD, presenting them in a more digestible format. This educational aspect is crucial, as it empowers individuals with knowledge about their condition, fostering a better understanding and acceptance of their symptoms. Education on one's condition can enhance cooperation with treatment plans and promote self-awareness, improving disorder management.
- Facilitates open dialogue: The clarity and accessibility of the template can catalyze open discussions between patients and healthcare providers. Having a tangible reference point makes patients feel more comfortable discussing their symptoms and concerns, leading to a more productive and collaborative therapeutic relationship.
- Promotes early intervention: Early diagnosis and intervention are critical in managing BPD effectively. The template can help identify the disorder earlier, allowing for timely therapeutic intervention. Early treatment is associated with a better prognosis, as it can prevent the progression of symptoms and the development of comorbid conditions.
- Supports personalized care: Understanding an individual's specific criteria allows clinicians to tailor their therapeutic approach to fit each patient's unique needs. This personalized care is essential in treating BPD, as it addresses the individual's struggles and strengths.
The BPD DSM-5 Criteria PDF template is more than just a diagnostic tool; it's a comprehensive resource that enhances the understanding, accuracy, and treatment of Borderline Personality Disorder. Its benefits extend beyond the clinical setting, touching the lives of those affected by BPD by offering them clarity, hope, and a path towards recovery.
Commonly asked questions
BPD is unique due to its intense emotional reactions, fear of abandonment, and unstable relationships.
Yes, with a combination of psychotherapy, medication, and support, many individuals with BPD can lead fulfilling lives.
Not necessarily. Many people see significant improvement in their symptoms and quality of life with appropriate treatment.

.jpg)

















-template.jpg)






















































































