Celiac Disease Test
Discover a reliable way to diagnose Celiac Disease. Gain valuable insights into symptoms, screening, and management strategies. Take control of your health.
�?�


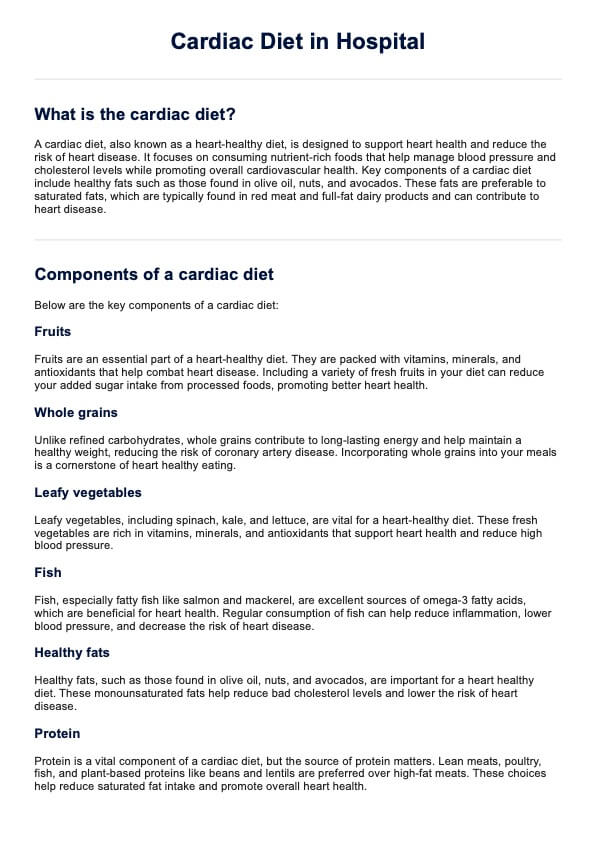
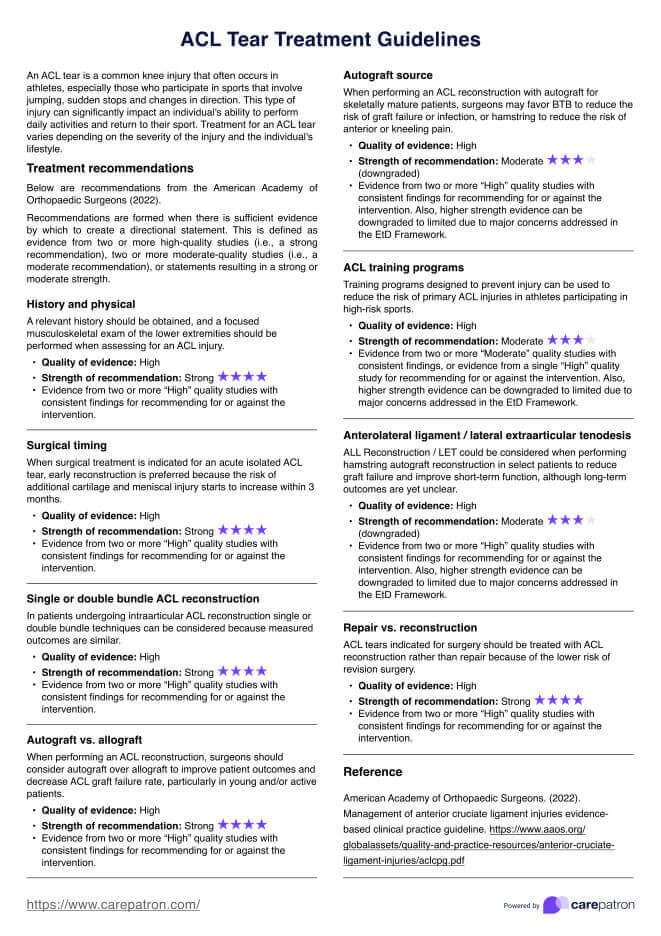
What is a Celiac Disease Test?
A Celiac Disease Test, also known as celiac panel or celiac serology, is a diagnostic procedure used to determine whether an individual has celiac disease, an autoimmune disorder triggered by the ingestion of gluten. Gluten is a protein found in wheat, barley, and rye, and for people with celiac disease, consuming even small amounts of gluten can lead to severe gastrointestinal and systemic symptoms.
The primary purpose of a Celiac Disease Test is to identify specific antibodies in the blood that are indicative of an immune response to gluten. The three primary antibodies tested for are:
- Anti-tissue transglutaminase (tTG) antibodies: These antibodies are commonly found in individuals with celiac disease. They are produced when the immune system mistakenly targets the small intestine's lining in response to gluten consumption.
- Anti-endomysial antibodies (EMA): EMA antibodies are another marker of the autoimmune reaction in celiac disease. They target the endomysium, a connective tissue layer surrounding muscle fibers.
- Anti-deamidated gliadin peptides (DGP) antibodies: These antibodies target a component of gluten called gliadin. Elevated levels of DGP antibodies can suggest celiac disease.
A blood sample is typically collected from the patient to perform the test. If the initial blood test results suggest celiac disease, a small intestine biopsy may be recommended to confirm the diagnosis. In the biopsy, a small piece of tissue is extracted from the small intestine and examined for characteristic damage caused by the autoimmune response to gluten.
Early and accurate diagnosis of celiac disease is crucial because it allows individuals to adopt a strict gluten-free diet, the only effective treatment for the condition. Celiac disease can lead to serious health complications without proper management, including malnutrition, osteoporosis, and an increased risk of other autoimmune disorders.
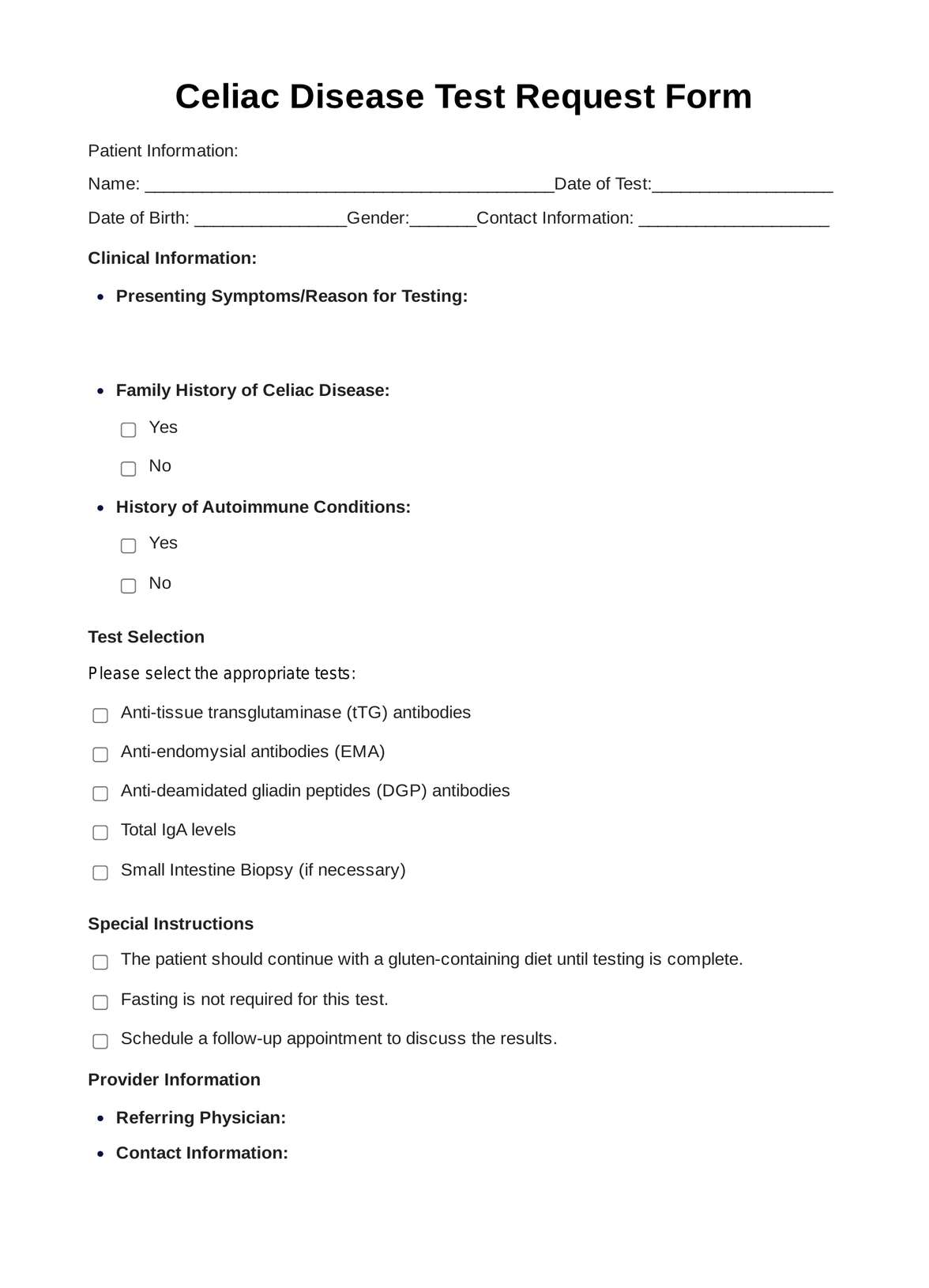
Celiac Disease Test Template
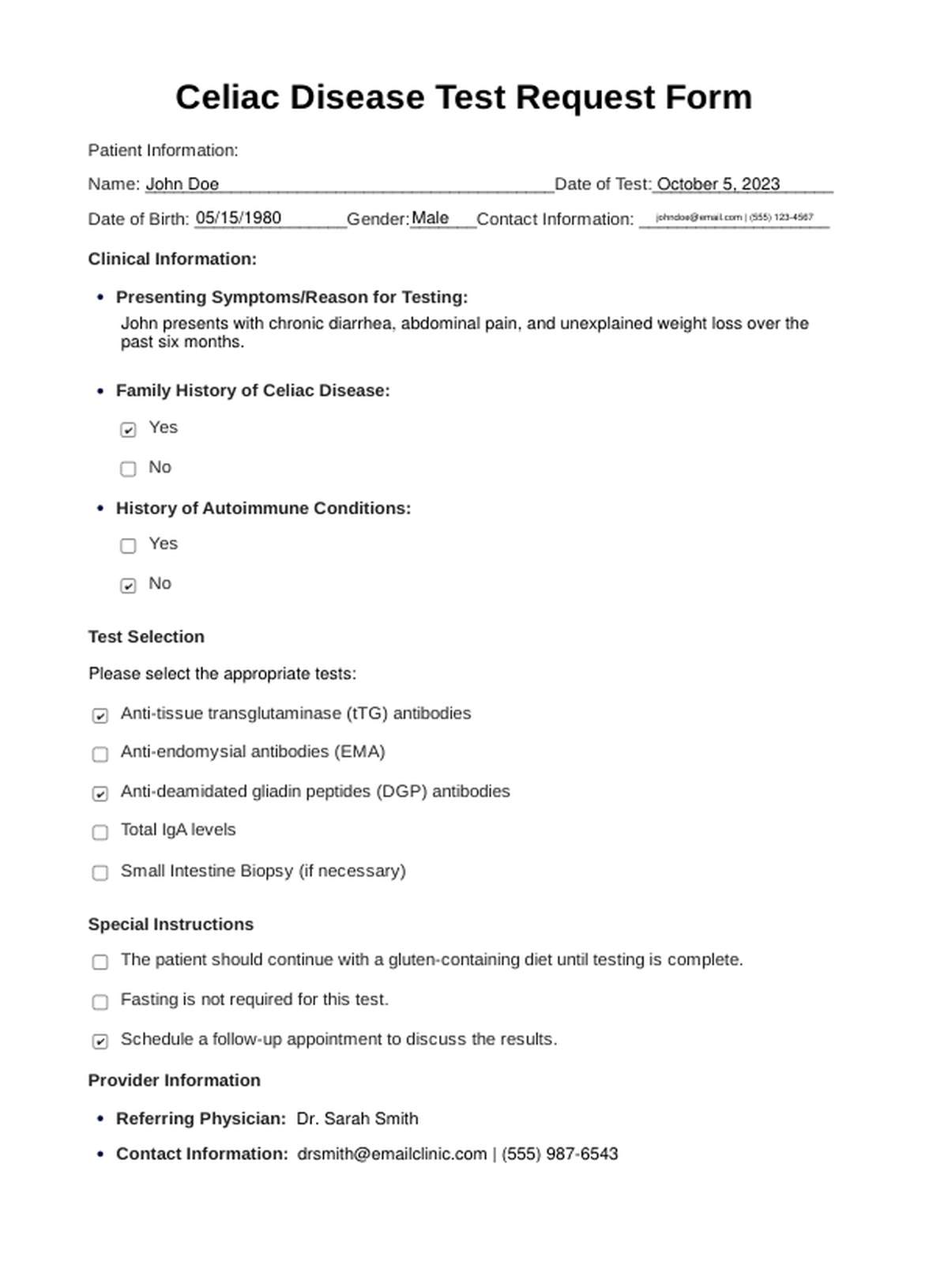
Celiac Disease Test Example
How Does it Work?
Consultation
Before undergoing a Celiac Disease Test, individuals should consult a healthcare provider, usually a gastroenterologist or primary care physician. These professionals can assess symptoms, medical history, and family history to determine the need for testing.
Blood Sample Collection
The primary diagnostic step involves drawing a blood sample from the individual. This sample is collected in a vial or test tube.
Laboratory Analysis
The blood sample is sent to a clinical laboratory for analysis. Technicians perform various tests in the lab to detect specific antibodies related to celiac disease. The primary antibodies analyzed include anti-tissue transglutaminase (tTG), anti-endomysial antibodies (EMA), and anti-deamidated gliadin peptides (DGP).
Results Interpretation
The healthcare provider receives the results once the laboratory analysis is complete. They interpret the findings and determine whether the individual has celiac disease based on antibody levels. Positive results may indicate the presence of celiac disease, while negative results suggest its absence.
Additional Testing (if necessary)
In some cases, further testing may be required to confirm the diagnosis. This can include a small intestine biopsy. During a biopsy, a thin, flexible tube with a camera (endoscope) is passed through the mouth and into the small intestine to collect tissue samples. These samples are examined for characteristic damage caused by celiac disease.
Consultation and Diagnosis
After reviewing the test results and, if necessary, biopsy findings, the healthcare provider discusses the diagnosis with the individual. If celiac disease is confirmed, the healthcare provider educates the patient about its management.
For individuals seeking a printable Celiac Disease Test form, it's important to note that healthcare professionals typically administer the test in a clinical setting. Patients usually wait to fill out the test form. Instead, they may be asked to provide personal information and consent for the test documented by healthcare staff.
When Would you use this Test?
The Celiac Disease Test is utilized by healthcare practitioners when specific clinical scenarios or symptoms suggest the possibility of celiac disease. Here are vital situations that prompt the use of this test:
- Gastrointestinal Symptoms: When patients present with persistent gastrointestinal symptoms such as chronic diarrhea, abdominal pain, bloating, vomiting, or unexplained weight loss, healthcare providers consider the Celiac Disease Test. These symptoms can indicate celiac disease, particularly if they do not respond to standard treatments.
- Failure to Thrive in Children: In pediatric medicine, the test is employed when children experience growth delays, poor weight gain, or failure to thrive. These signs may raise suspicion of celiac disease as it can interfere with nutrient absorption in children.
- Autoimmune Diseases: When patients are diagnosed with autoimmune disorders such as type 1 diabetes, rheumatoid arthritis, or autoimmune thyroid disease, practitioners may use the Celiac Disease Test. These conditions are associated with an increased risk of celiac disease, and screening can be beneficial.
- Family History: Individuals with a history of celiac disease have a higher risk of developing the condition. Therefore, practitioners might recommend the test for individuals with close relatives with a confirmed diagnosis.
- Dermatological Symptoms: Dermatologists consider the Celiac Disease Test when patients exhibit skin conditions like dermatitis herpetiformis, characterized by itchy, blistering rashes. Dermatitis herpetiformis is strongly linked to celiac disease.
- Suspected Gluten Sensitivity: For patients who report gluten sensitivity or non-specific gastrointestinal complaints in response to gluten consumption, the Celiac Disease Test can help determine if celiac disease is the underlying cause.
- Monitoring Celiac Disease Management: After an initial diagnosis of celiac disease, healthcare providers may use the test to monitor the effectiveness of a gluten-free diet and check for any ongoing antibody production, ensuring the patient's condition is well-controlled.
What do the Results Mean?
Interpreting the results of a Celiac Disease Test is a critical step in diagnosing and managing this autoimmune condition. Here's what common test results mean:
- Negative Results: A negative result on the Celiac Disease Test means that the antibodies associated with the disease were not detected in the blood, indicating that celiac disease is unlikely the cause of symptoms. False negatives are possible, especially if the individual has recently started a gluten-free diet or the disease is in its early stages.
- Positive Results: A positive Celiac Disease Test indicates elevated celiac-related antibodies in the blood, a strong indicator of the condition. Further confirmation is sought through a small intestine biopsy, as positive results mean that gluten is causing damage to the intestine's lining.
- Indeterminate Results: Sometimes, test results are inconclusive, which means that further testing or monitoring may be recommended to clarify the diagnosis.
- Follow-Up Biopsy: A positive Celiac Disease Test result usually leads to a small intestine biopsy with a camera tube to confirm the diagnosis. Villous atrophy, or damage to the intestinal lining, confirms the diagnosis of celiac disease.
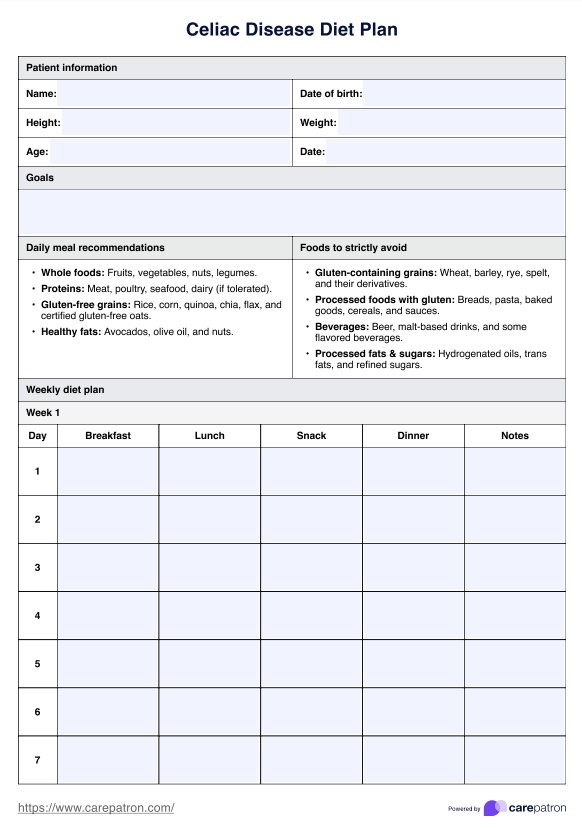
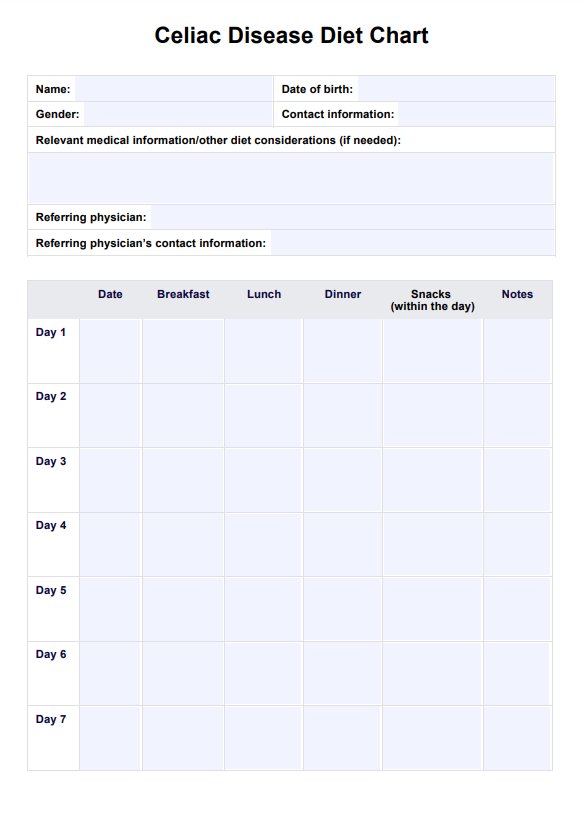
- Management: Regardless of the test results, if celiac disease is confirmed, the primary treatment is a strict, lifelong gluten-free diet. This diet eliminates all sources of gluten, including wheat, barley, and rye, to prevent further damage to the small intestine and alleviate symptoms. Nutritional counseling may be recommended to help patients adapt to the dietary restrictions and ensure they receive essential nutrients.
Research & Evidence
Celiac disease has been recognized for centuries, with documented cases dating back to ancient Greece and Rome. However, in the mid-20th century, researchers began understanding the disease's autoimmune nature.
In the 1950s and 1960s, physicians and scientists identified gluten, a protein found in wheat, barley, and rye, as triggering celiac disease symptoms. This discovery was a significant breakthrough in understanding the condition.
The 1980s and 1990s saw the development and refinement of antibody tests to diagnose celiac disease. These tests detect specific antibodies like anti-tissue transglutaminase (tTG), anti-endomysial antibodies (EMA), and anti-deamidated gliadin peptides (DGP). These tests revolutionized celiac disease diagnosis by providing non-invasive and accurate means of detection.
Over the years, a substantial body of research has emerged, further solidifying the link between celiac disease and gluten consumption. Research has also helped clarify the genetic factors involved, identifying specific genes associated with an increased risk of celiac disease, such as HLA-DQ2 and HLA-DQ8.
Leading medical organizations, such as the American College of Gastroenterology and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition, have developed clinical guidelines for diagnosing and managing celiac disease. These guidelines are based on robust scientific evidence and help inform healthcare practitioners about best practices.
Research into celiac disease continues to evolve, with ongoing studies exploring various aspects of the condition, including its epidemiology, genetics, immunology, and the development of new diagnostic and therapeutic approaches.
References
- Celiac disease - Diagnosis and treatment - Mayo Clinic. (2023, September 12). https://www.mayoclinic.org/diseases-conditions/celiac-disease/diagnosis-treatment/drc-20352225#:~:text=Two%20blood%20tests%20can%20help,to%20rule%20out%20celiac%20disease.
- Celiac disease screening. (n.d.). https://medlineplus.gov/lab-tests/celiac-disease-screening/
- Celiac disease screening | Celiac Disease Foundation. (n.d.). Celiac Disease Foundation. https://celiac.org/about-celiac-disease/screening-and-diagnosis/screening/
- Celiac Disease testing and diagnosis | BeyondCeliac.org. (2023, May 30). Beyond Celiac. https://www.beyondceliac.org/celiac-disease/get-tested/
- Celiac disease tests. (2022). National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/professionals/clinical-tools-patient-management/digestive-diseases/celiac-disease-health-care-professionals
- How Do I Know If I Have Celiac Disease? (2017, January 4). WebMD. https://www.webmd.com/digestive-disorders/celiac-disease/celiac-disease-diagnosis-tests
- Professional, C. C. M. (n.d.). Celiac disease. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/14240-celiac-disease
- Website, N. (2023, April 4). Diagnosis. nhs.uk. https://www.nhs.uk/conditions/coeliac-disease/diagnosis/
Commonly asked questions
Healthcare providers, including primary care physicians, gastroenterologists, pediatricians, and specialists in related fields, typically request a Celiac Disease Test based on patient symptoms, risk factors, or medical history.
Celiac Disease Tests are used when individuals present symptoms like chronic diarrhea, abdominal pain, unexplained weight loss, or a suspicion of celiac disease due to factors like family history or autoimmune conditions.
Celiac Disease Tests involve collecting blood samples to detect specific antibodies related to celiac disease. A small intestine biopsy may be performed for confirmation if initial tests are positive.
The blood sample collection for a Celiac Disease Test typically takes just a few minutes. The time for results varies but can range from a few days to a couple of weeks, depending on the laboratory and specific tests performed.