The most current guidelines for managing hypertension include the 2017 ACC/AHA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults, the 2018 ESC/ESH Guidelines for the management of arterial hypertension, and the 2020 International Society of Hypertension Global Hypertension Practice Guidelines.
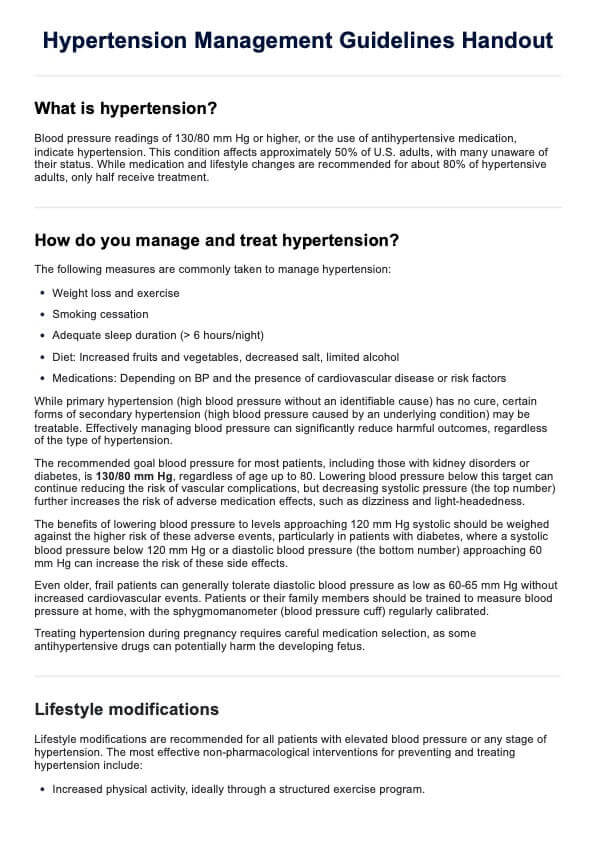
Hypertension Management Guidelines Handout
Download a Hypertension Management Guidelines Handout to serve as a reference and educational tool for patients with hypertension.
Hypertension Management Guidelines Handout Template
Commonly asked questions
Standard treatment guidelines recommend initiating pharmacotherapy for hypertension when blood pressure is >140/90 mmHg, with a target goal of <130/80 mmHg. Acceptable first-line antihypertensive medication is also recommended. Combination therapy with two agents is often required to achieve blood pressure targets.
The current first-line pharmacological treatment for hypertension includes ACE inhibitors, ARBs, dihydropyridine calcium channel blockers, and thiazide diuretics.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











