Spasticity Test
Download our free Spasticity Test example and learn how these tests aid in diagnosing and managing muscle spasticity effectively.


What is spasticity?
Spasticity is a neurological condition characterized by an abnormal increase in muscle tone or stiffness, which can interfere with movement, speech, and gait. It is often a symptom of various neurological disorders, including traumatic brain injury (TBI), cerebral palsy, multiple sclerosis, and spinal cord injury. Spasticity disrupts normal central nervous system (CNS) control over muscle tone and muscle contraction, leading to involuntary muscle contractions, exaggerated reflexes, and reduced functional abilities.
The severity of spasticity can range from mild muscle stiffness to severe, painful muscle spasms and contractures, significantly impacting an individual's quality of life. It can affect any body part but is most commonly seen in the limbs. The condition can lead to secondary complications like joint deformities, skin breakdown, and chronic pain. Understanding spasticity is crucial for effective management and treatment, as it plays a significant role in rehabilitation therapy and overall patient care.
A multidisciplinary approach involving physical therapists, occupational therapists, neurologists, and other healthcare professionals is often required to manage spasticity. Treatment options include physical therapy, medication, botulinum toxin injections, and, in severe cases, surgery. The treatment goals are to reduce muscle stiffness, improve mobility and function, and enhance the patient's quality of life.
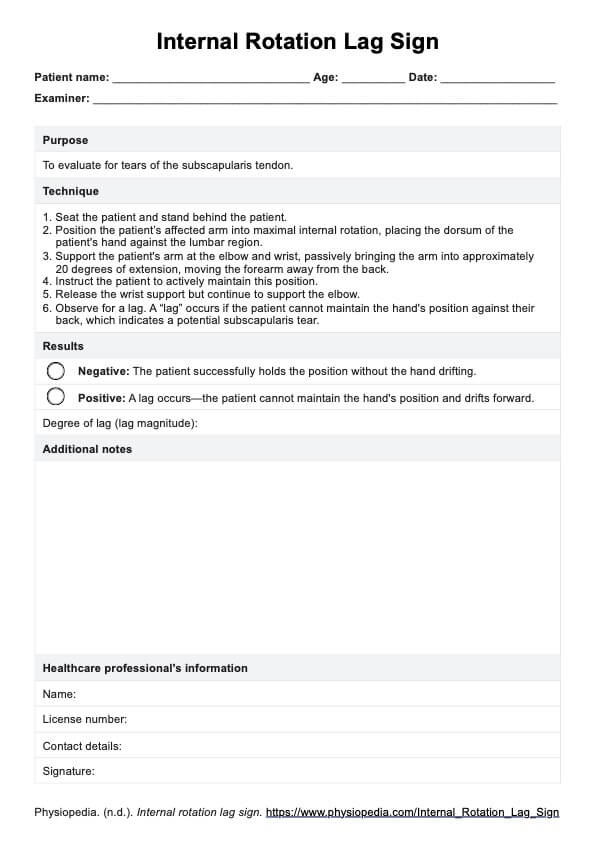
Spasticity Test Template
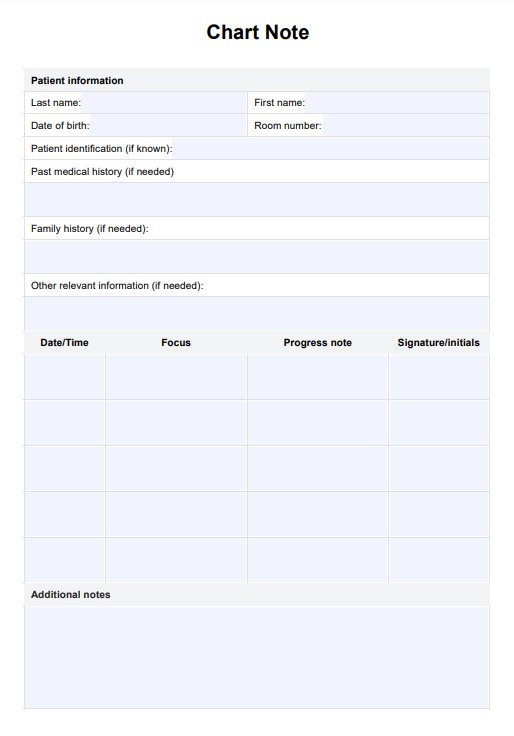
Spasticity Test Example
Spasticity and traumatic brain injury
Spasticity is a common complication following a traumatic brain injury (TBI). It occurs due to damage to the brain's areas that control voluntary muscle movement. In TBI patients, spasticity can manifest in various ways, including increased muscle tone, spasms, and clonus (rapid muscle contractions). These symptoms can develop days, weeks, or even months after the initial injury.
The presence of spasticity in TBI patients can significantly hinder the rehabilitation process. It can limit the range of motion, reduce functional abilities, and increase the risk of developing secondary complications like contractures and pressure sores. Early identification and management of spasticity are crucial in TBI care.
Treatment typically involves a combination of physical therapy, medication, and other modalities like splinting or casting. In some cases, more invasive treatments like intrathecal baclofen therapy or botulinum toxin injections may be necessary. Managing spasticity in TBI patients requires a patient-centered approach, considering the individual's needs, goals, and overall health status. Rehabilitation programs should be tailored to address the unique challenges of spasticity, focusing on improving mobility, function, and independence.
Clinical measures of spasticity
Clinical measures of spasticity are indispensable in the assessment and management of patients with conditions like cerebral palsy, traumatic brain injury, multiple sclerosis, and spinal cord injury. These measures aid in diagnosing spasticity and play a crucial role in monitoring its progression and evaluating the effectiveness of various treatment interventions. Here's an expanded look at some of the most commonly used clinical measures:
Modified Ashworth Scale (MAS)
The MAS is a widely recognized tool for assessing spasticity. It measures the resistance encountered during passive stretching of a muscle, with a scale ranging from 0 (no increase in muscle tone) to 4 (limb rigid in flexion or extension). The MAS is particularly useful for its simplicity and ease of use, making it a popular choice in clinical and research settings. However, it's important to note that while the MAS is effective in measuring resistance, it may not fully capture the dynamic aspects of spasticity (Bohannon & Smith, 1987).
Tardieu scale
The Tardieu Scale offers a more nuanced assessment compared to the MAS. It evaluates the quality of muscle reaction to stretch at different velocities, providing valuable information about the severe spinal spasticity and muscle's response to speed. This scale is particularly useful in distinguishing between spasticity and contracture and planning treatment strategies tailored to the patient's needs (Haugh et al., 2006).
Penn spasm frequency scale
This scale evaluates the frequency and severity of muscle spasms, a common symptom in patients with spinal cord injuries. The scale helps quantify the impact of spasms on the patient's quality of life and monitor the effectiveness of interventions aimed at reducing spasm frequency (Penn et al., 1989).
Functional Independence Measure (FIM)
While the FIM is not a direct measure of spasticity, it is crucial in assessing the impact of spasticity on a patient's functional independence. The FIM evaluates activities of daily living, including self-care, mobility, and social function. By understanding how spasticity affects these areas, healthcare providers can develop more targeted rehabilitation plans (Hamilton et al., 1994).
Other measures
In addition to these scales, other tools like electromyography (EMG) and goniometry can provide a more comprehensive assessment. EMG measures muscle activity, while goniometry assesses joint angles, which are important in understanding the biomechanical aspects of spasticity.
Clinical measures of spasticity are critical in providing healthcare professionals with the necessary information to make informed decisions about patient care. These measures aid in diagnosis and monitoring and are pivotal in guiding treatment and rehabilitation efforts, ultimately improving patient outcomes.
What does this test measure?
Spasticity tests are crucial in the clinical assessment of patients with neurological disorders. These tests measure several key aspects:
- Muscle tone: One of the primary measurements in spasticity tests is muscle tone. Muscle tone refers to the muscle's resistance to passive movement or stretching. Muscle tone is often increased in individuals with spasticity, leading to stiffness and reduced mobility.
- Resistance to passive stretching: Spasticity tests evaluate how muscles respond to being stretched passively. Increased resistance to stretching is a hallmark of spasticity. This resistance is often velocity-dependent, meaning it varies with the speed of the stretch.
- Exaggerated reflexes: The tests assess reflexes, often heightened in spasticity. These exaggerated reflexes can contribute to muscle stiffness and involuntary muscle contractions.
- Range of motion and muscle stiffness: The tests measure the range of motion in affected joints. Spasticity can limit this range due to increased muscle stiffness. Assessing the range of motion helps understand the functional impact of spasticity on the patient.
- Functional impact: Beyond the physical measurements, spasticity tests also aim to understand how spasticity affects a patient's daily activities and overall function. This includes assessing the impact on mobility, self-care activities, and quality of life.
- Differentiation from other conditions: Spasticity tests help differentiate spasticity from other muscle tone abnormalities like rigidity or dystonia, characterized by different resistance patterns to passive movement.
By accurately measuring these aspects, healthcare providers can tailor treatment plans to the individual's needs, including physical therapy, medication, and other interventions.
How does this assessment work?
The assessment of spasticity is a multi-faceted process that involves both clinical and physical examination, and the use of specific measurement tools:
- Clinical examination: The initial step in spasticity assessment is a thorough clinical examination. This includes evaluating the patient's muscle tone, reflexes, and range of motion. The clinician observes the patient's response to passive movement of the limbs, noting any resistance or involuntary muscle contractions.
- Use of measurement tools: Tools like the Modified Ashworth Scale (MAS) or the Tardieu Scale provide a more objective measurement of spasticity. The MAS measures resistance during passive muscle stretching, while the Tardieu Scale assesses muscle reaction at different velocities.
- Observation of reflexes: Testing reflexes is integral to the assessment. This involves evaluating the stretch reflexes, which are often exaggerated in spasticity.
- Functional assessment: The assessment also includes evaluating how spasticity affects the patient's daily activities. This may involve observing the patient performing specific tasks or activities to understand the functional implications of spasticity.
- Patient history: A comprehensive patient history, including the onset of symptoms, progression of the condition, and any previous treatments, is crucial for a complete assessment.
- Collaboration with other specialists: In some cases, collaboration with other specialists, such as neurologists or rehabilitation therapists, may be necessary to assess and plan treatment for spasticity fully.
This comprehensive approach to assessment is vital for accurately diagnosing spasticity, determining its severity, and planning effective interventions. Regular reassessment is also important to monitor the progression of spasticity and the effectiveness of treatments.
Interpreting the results & next steps
Interpreting the results of a spasticity test is a nuanced process that requires a comprehensive understanding of the patient's condition and the impact of spasticity on their daily life. The interpretation and subsequent steps involve several vital aspects:
- Analyzing measurement scores: The scores obtained from tools like the Modified Ashworth Scale or the Tardieu Scale provide quantitative data on muscle tone and resistance to passive movement. These scores are crucial in determining the severity of spasticity. Higher scores typically indicate more severe spasticity, characterized by increased muscle stiffness and reduced range of motion.
- Clinical observations: Besides the scores, clinical observations made during the assessment are equally important. These observations include the patient's response to passive movement, involuntary muscle contractions, and any observed abnormalities in reflexes. Clinicians also consider any reported discomfort or pain during the assessment.
- Functional impact assessment: Understanding how spasticity affects the patient's daily activities is vital. This includes evaluating the impact on mobility, self-care, work, and recreational activities. The goal is to gauge how spasticity hinders the patient's ability to perform everyday tasks and participate in social and occupational activities.
- Developing a treatment plan: Healthcare providers develop a personalized treatment plan based on the assessment results.
- Monitoring and follow-up: Regular follow-up assessments are essential to monitor the effectiveness of the treatment plan. Adjustments to the plan may be necessary based on the patient's progress and any changes in their condition.
- Patient education and support: It is crucial to educate the patient and their family about spasticity, its implications, and the importance of adherence to the treatment plan. Providing emotional support and addressing any concerns or questions they may have is also an integral part of the treatment process.
- Collaboration with other specialists: In some cases, collaboration with other healthcare professionals, such as neurologists, rehabilitation specialists, or pain management experts, may be necessary to provide comprehensive care.
- Setting realistic goals: Establishing realistic and achievable goals with the patient is essential for successful treatment. These goals should focus on improving functional abilities, reducing discomfort, and enhancing the patient's overall quality of life.
- Evaluating the need for assistive devices: Assessing the need for assistive devices such as wheelchairs, walkers, or adaptive equipment can be part of the treatment plan to enhance mobility and independence.
- Considering alternative therapies: Exploring alternative therapies like acupuncture, massage, or hydrotherapy as adjunct treatments may benefit some patients.
Interpreting the results of a spasticity test is a multifaceted process that guides the development of a comprehensive, patient-centered treatment plan. This plan should address the physical, functional, and emotional aspects of living with spasticity, aiming to improve the patient's quality of life and enable them to achieve their maximum potential.
You can take advantage of this electromyography template and Tardieu scale template to optimize your diagnostic procedures and ensure detailed muscle assessments. This tool helps in capturing and analyzing muscle electrical activity, contributing to a more thorough understanding of neuromuscular health.
Research and evidence
Research in the field of spasticity has made substantial contributions to the understanding and management of this complex condition. Spasticity, characterized by an abnormal increase in muscle tone or stiffness, often results from conditions affecting the brain or spinal cord, such as cerebral palsy, traumatic brain injury, stroke, and multiple sclerosis. The body of research in this area encompasses various aspects, including developing and validating assessment tools, exploring underlying mechanisms, and evaluating treatment effectiveness.
A significant research focus has been creating reliable and valid tools for assessing spasticity. The Modified Ashworth Scale (MAS) and the Tardieu Scale are among the most widely used measures measuring spasticity. Studies have examined their inter-rater and intra-rater reliability, providing clinicians with dependable tools for evaluating spasticity severity (Pandyan et al., 1999; Gracies et al., 2010). These tools have been essential in clinical settings and research studies for quantifying spasticity and monitoring treatment outcomes.
Research has delved into the neurophysiological mechanisms underlying spasticity. It is understood that spasticity results from an imbalance in signals from the central nervous system to the muscles, often due to lesions in the upper motor neurons. This imbalance increases muscle tone and exaggerated tendon reflexes (Lance, 1980). Understanding these mechanisms is crucial for developing targeted therapies.
A substantial body of research has been dedicated to evaluating the effectiveness of various spasticity treatments. These include physical therapy interventions, pharmacological treatments (such as baclofen, tizanidine, and botulinum toxin), and surgical procedures.
Studies have shown that an integrated approach combining physical therapy with pharmacological treatments can be efficient (Francisco et al., 2013). Research has also explored newer modalities like intrathecal baclofen therapy and botulinum toxin injections, demonstrating their efficacy in reducing spasticity and improving functional outcomes (Meythaler et al., 2001; Wissel et al., 2009).
Research has consistently highlighted the impact of spasticity on patients' quality of life. Spasticity can significantly impair mobility, daily activities, and social participation. Studies have shown that effective spasticity management can improve these areas, enhancing patients' overall quality of life (Sköld et al., 1999).
Ongoing research continues to explore new treatment avenues, including novel pharmacological agents and advanced physical and rehabilitation medicine techniques. There is also a growing interest in understanding the long-term outcomes of spasticity management and its impact on healthcare systems.
Research in spasticity has been instrumental in advancing clinical practice. It has provided valuable insights into assessment, treatment, and the overall impact of spasticity on individuals' lives. This body of work continues to evolve, offering hope for improved management strategies and better outcomes for patients affected by spasticity.
References
Francisco, G. E., McGuire, J. R., Post, A. B., & Zorowitz, R. D. (2013). The role of intrathecal baclofen in the treatment of spasticity. PM&R, 5(1), S18-S24.
Gracies, J. M., Burke, K., Clegg, N. J., Browne, R., Rushing, C., Fehlings, D., ... & Delgado, M. R. (2010). Reliability of the Tardieu Scale for assessing spasticity in children with cerebral palsy. Archives of Physical Medicine and Rehabilitation, 91(3), 421-428.
Lance, J. W. (1980). Symposium synopsis. In Spasticity: Disordered Motor Control (pp. 485-494). Year Book Medical Publishers.
Meythaler, J. M., Guin-Renfroe, S., Johnson, A., & Brunner, R. C. (2001). Prospective assessment of tizanidine for spasticity due to acquired brain injury. Archives of Physical Medicine and Rehabilitation, 82(9), 1155-1163.
Pandyan, A. D., Johnson, G. R., Price, C. I., Curless, R. H., Barnes, M. P., & Rodgers, H. (1999). A review of the properties and limitations of the Ashworth and Modified Ashworth Scales as measures of spasticity. Clinical Rehabilitation, 13(5), 373-383.
Sköld, A., Levi, R., & Seiger, Å. (1999). Spasticity after traumatic spinal cord injury: nature, severity, and location. Archives of Physical Medicine and Rehabilitation, 80(12), 1548-1557.
Wissel, J., Ward, A. B., Erztgaard, P., Bensmail, D., Hecht, M. J., Lejeune, T. M., ... & Schnider, P. (2009). European consensus table on botulinum toxin type A in adult spasticity. Journal of Rehabilitation Medicine, 41(1), 13-25.
Commonly asked questions
The spasticity test is designed to assess the degree of muscle stiffness, resistance to passive stretching, and exaggerated reflexes in individuals with neurological disorders. It helps in determining the severity of spasticity and guiding treatment plans.
Individuals with conditions like cerebral palsy, traumatic brain injury, multiple sclerosis, and spinal cord injury, which are known to cause spasticity, should undergo this test. It's essential for those experiencing increased muscle tone or difficulty with movement and gait.
The test typically involves clinical examination techniques such as the Modified Ashworth Scale or the Tardieu Scale, where a therapist assesses muscle tone and response to passive movement. It may also include observing reflexes and functional impacts of spasticity.

.jpg)