Ottawa Ankle Rules
Use the Ottawa Ankle Rules to decide whether your patients' ankle and foot injuries need imaging. Try our template today!


What are the Ottawa Ankle Rules?
The Ottawa Ankle Rules, also known as the Ottawa Rules, are a set of clinical guidelines for deciding whether patients with acute ankle injuries or foot injuries need radiography for diagnosis. The Ottawa Ankle Rules have been found to be accurate in assessing whether an injury is an ankle or foot fracture, with a sensitivity of almost 100%; that is why it is called a decision-making assessment and is used to determine whether a radiograph is necessary (Kerkhoffs et al., 2012).
Ankle and foot injuries are commonly encountered in emergency departments and take an enormous toll on radiography or imaging requests. However, only a small percentage of the imaging done on ankle and midfoot injuries show fractures. Not only because it contributes to hospital costs, but some injuries also do not really need to be ordered for an x-ray. In order to mitigate this waste, Stiell and colleagues pioneered a study to develop clinical decision rules for using radiography on an acute ankle injury, which meant to decrease unnecessary requests for imaging or radiography (Stiell et al., 1992). The Ottawa Ankle Rules direct the attending physician on whether to request imaging for the patient.
Many types of healthcare professionals can apply the Ottawa Ankle Rules to guide their clinical decisions. Physicians, physical therapists, nurses, radiologists, chiropractors, physiotherapists, and occupational therapists can utilize these rules to determine if radiography is required. This ensures that various practitioners involved in patient care can rely on the same evidence-based criteria, promoting accurate diagnosis, reducing unnecessary imaging, and improving overall patient management.
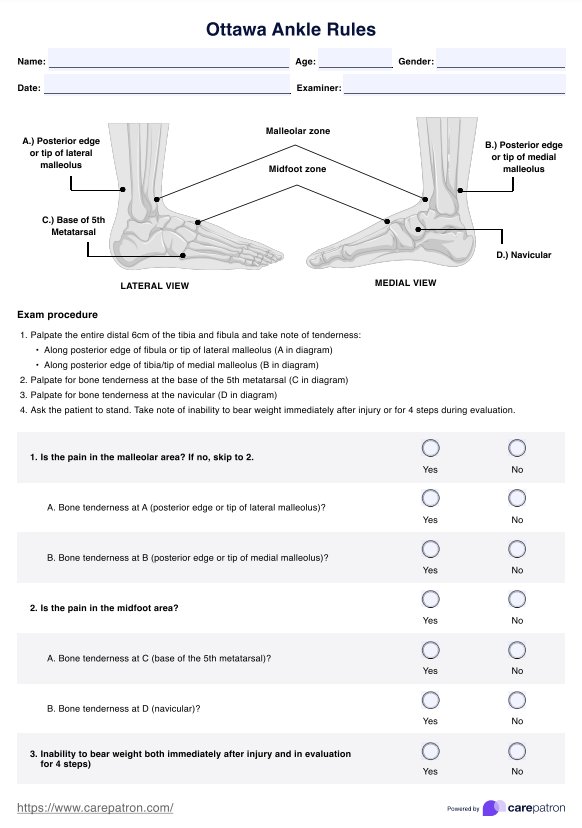
Ottawa Ankle Rules Template
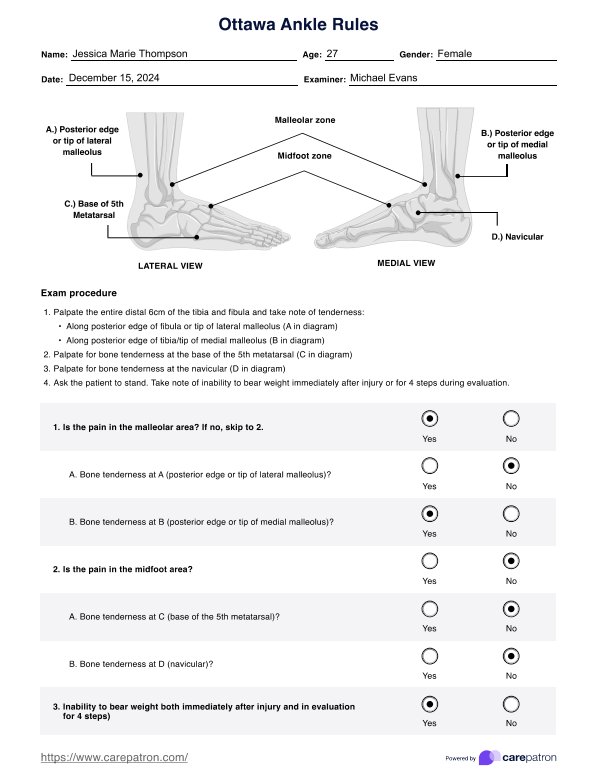
Ottawa Ankle Rules Example
How to use our Ottawa Ankle Rules template
Our Carepatron Ottawa Ankle Rules template helps healthcare professionals systematically evaluate patients for ankle and midfoot fractures and ankle fractures, determine when to order imaging, and exclude fractures when appropriate. It provides procedures for examination (including palpation of the posterior edge of the tibia and fibula, checking for bone tenderness, and assessing the navicular bone) and includes a guide for interpreting results. This ensures clinicians can effectively distinguish between an ankle sprain injury and a fracture, as well as identify traumatic ankle pain and inability to bear weight immediately. The template also has fields for recording patient information and clinical notes, making the entire process more efficient and organized.
Step 1: Access the template
Click the “Use template” button to open the template in the Carepatron app. You can customize the template before you fill it out or print it. You can also click the “Download” button for a printable, ready-to-fill PDF.
Step 2: Assess the patient
Explain the examination process to the patient. Palpate the posterior edge of the tibia and fibula and check for bone tenderness at the navicular bone and the base of the 5th metatarsal. Evaluate for ankle sprain injury or traumatic ankle pain and note any inability to bear weight immediately. Document your findings on the template to determine if ankle and midfoot fractures or ankle fractures are likely and whether you can exclude fractures from consideration.
Step 3: Interpret the findings
Use the guidelines indicated in the templates to determine if ankle and midfoot fractures or ankle fractures are likely. If the criteria suggest imaging, proceed with radiographs. If not, you can exclude fractures confidently. Record your interpretations and recommended next steps.
Step 4: Discuss results & teach the patient
Review the assessment results with the patient. If you recommend radiographic imaging, explain why it’s needed. If imaging isn’t required, reassure them of your clinical judgment. Show the patient how to read and use the template if they wish to follow their own progress or share the findings with other healthcare professionals. This approach promotes transparency, patient involvement, and efficient communication.
Interpreting the results
If the findings match the Ottawa Ankle Rules criteria, such as bone tenderness in specified areas or inability to bear weight immediately, then radiographic imaging is recommended. This helps confirm or rule out fractures and guides appropriate interventions. If the patient’s presentation does not meet these criteria, you can often forgo imaging and manage the condition conservatively, which saves time and resources.
The Ottawa Ankle Rules primarily address acute injuries but can also help differentiate conditions that might lead to chronic ankle pain. Identifying fractures early prevents improper healing and long-term discomfort. Ensuring you request imaging only when indicated sets the patient on the right treatment path and helps avoid unnecessary procedures.
When to use the Ottawa Ankle Test
Healthcare professionals often rely on the Ottawa Ankle Test to identify when radiographic imaging may be necessary for patients presenting with ankle or foot injuries. By applying the Ottawa Ankle Rule, you can determine if imaging can help confirm or exclude fractures, reducing the likelihood of unnecessary radiographs and improving patient flow. Below are scenarios where the test proves valuable:
- Assessing an acute ankle sprain or ankle trauma: Emergency physicians can quickly decide if imaging is required, streamlining diagnosis and treatment.
- Evaluating traumatic midfoot pain: Determine whether the injury involves bone pathology that warrants imaging.
- Avoiding excess imaging: Use the test to guide clinical judgment, ensuring that patients only undergo imaging when the findings suggest a potential fracture.
Benefits of our free Ottawa Ankle Rules template
Our free Ottawa Ankle Rules template from Carepatron streamlines the assessment process and provides an organized, user-friendly tool for healthcare professionals. This template gives you immediate access to a convenient and customizable form that helps you evaluate injuries efficiently and guide patient care decisions.
- Accurate and evidence-based: Follow the well-established Ottawa Ankle Rules criteria within an easy-to-use format, ensuring reliable and clinically sound evaluations.
- Improved workflow: Clarify when to order radiographic tests to reduce unnecessary imaging requests and streamline patient care in your emergency department.
- Time-saving layout: Minimize repetitive documentation and quickly record essential findings, allowing you to focus on patient care.
- Enhanced patient communication: Use the template as a reference point when explaining the rationale behind imaging or conservative management, helping patients understand their treatment plan.
In addition to these benefits, using Carepatron’s free template connects you to the broader Carepatron healthcare practice management platform. Signing up for the Carepatron app allows you to access secure, cloud-based storage, seamless team collaboration, and integrated patient engagement tools that further optimize your practice.
References
Kerkhoffs, G. M., van den Bekerom, M., Elders, L. A. M., van Beek, P. A., Hullegie, W. A. M., Bloemers, G. M. F. M., de Heus, E. M., Loogman, M. C. M., Rosenbrand, K. C. J. G. M., Kuipers, T., Hoogstraten, J. W. A. P., Dekker, R., ten Duis, H.-J., van Dijk, C. N., van Tulder, M. W., van der Wees, P. J., & de Bie, R. A. (2012). Diagnosis, treatment and prevention of ankle sprains: an evidence-based clinical guideline. British Journal of Sports Medicine, 46(12), 854–860. https://doi.org/10.1136/bjsports-2011-090490
Stiell, I. G., Greenberg, G. H., McKnight, R. D., Nair, R. C., McDowell, I., & Worthington, J. R. (1992). A study to develop clinical decision rules for the use of radiography in acute ankle injuries. Annals of Emergency Medicine, 21(4), 384–390. https://doi.org/10.1016/s0196-0644(05)82656-3
Commonly asked questions
While there isn’t a universally recognized mnemonic, some clinicians remember "44-55-66-PM", which helps you remember the criteria that indicate a need for imaging. "44" stands for inability to bear weight for 4 steps immediately after the injury and 4 steps in the clinical setting; "55" is for bone tenderness at the base of the 5th metatarsal and at the navicular bone; and "66" is for bone tenderness along the posterior edge of both the lateral and medial malleoli, typically assessed over 6 cm.
They include five key criteria: bone tenderness at the posterior edge or tip of the lateral malleolus, bone tenderness at the posterior edge or tip of the medial malleolus, bone tenderness at the base of the 5th metatarsal, bone tenderness at the navicular bone, and inability to bear weight immediately and in the emergency department for four steps. Radiographic imaging is usually indicated if these criteria are met within their respective zones (malleolar or midfoot).
If a patient cannot bear weight both immediately after the injury and for four steps during evaluation, this finding typically indicates a higher likelihood of fracture and signals the need for radiographic imaging. This weight-bearing criterion helps identify significant injuries that conservative management might otherwise overlook.