The Stroke Rehabilitation Assessment of Movement (STREAM)
Looking for a stroke rehabilitation assessment of movement? Download a free PDF from Carepatron and effectively assess movement in stroke patients.


What is the stroke rehabilitation assessment of movement?
The stroke rehabilitation assessment of movement is a crucial component in the overall rehabilitation process for individuals who have experienced a stroke. This assessment evaluates stroke survivors' motor abilities, coordination, and functional movement patterns.
Following a stroke, many individuals experience impairments in their ability to move, which can significantly impact their daily activities and quality of life.
The stroke rehabilitation assessment of movement aims to systematically evaluate these impairments and design a tailored rehabilitation plan to address specific challenges.
During the assessment, healthcare professionals, such as physical and occupational therapists, utilize a variety of standardized tests and outcome measures to quantify the extent of motor deficits.
These assessments often include evaluating muscle strength, range of motion, balance, coordination, and overall functional mobility.
Through these evaluations, therapists gain valuable insights into each individual's unique needs and limitations, laying the foundation for personalized rehabilitation strategies.
The importance of the stroke rehabilitation assessment of movement lies in its ability to guide therapeutic interventions effectively. By identifying specific areas of impairment, therapists can design targeted exercises and interventions to improve strength, coordination, and overall motor function.
This tailored approach enhances the efficiency of the rehabilitation process, facilitating a more rapid and comprehensive recovery for stroke survivors.
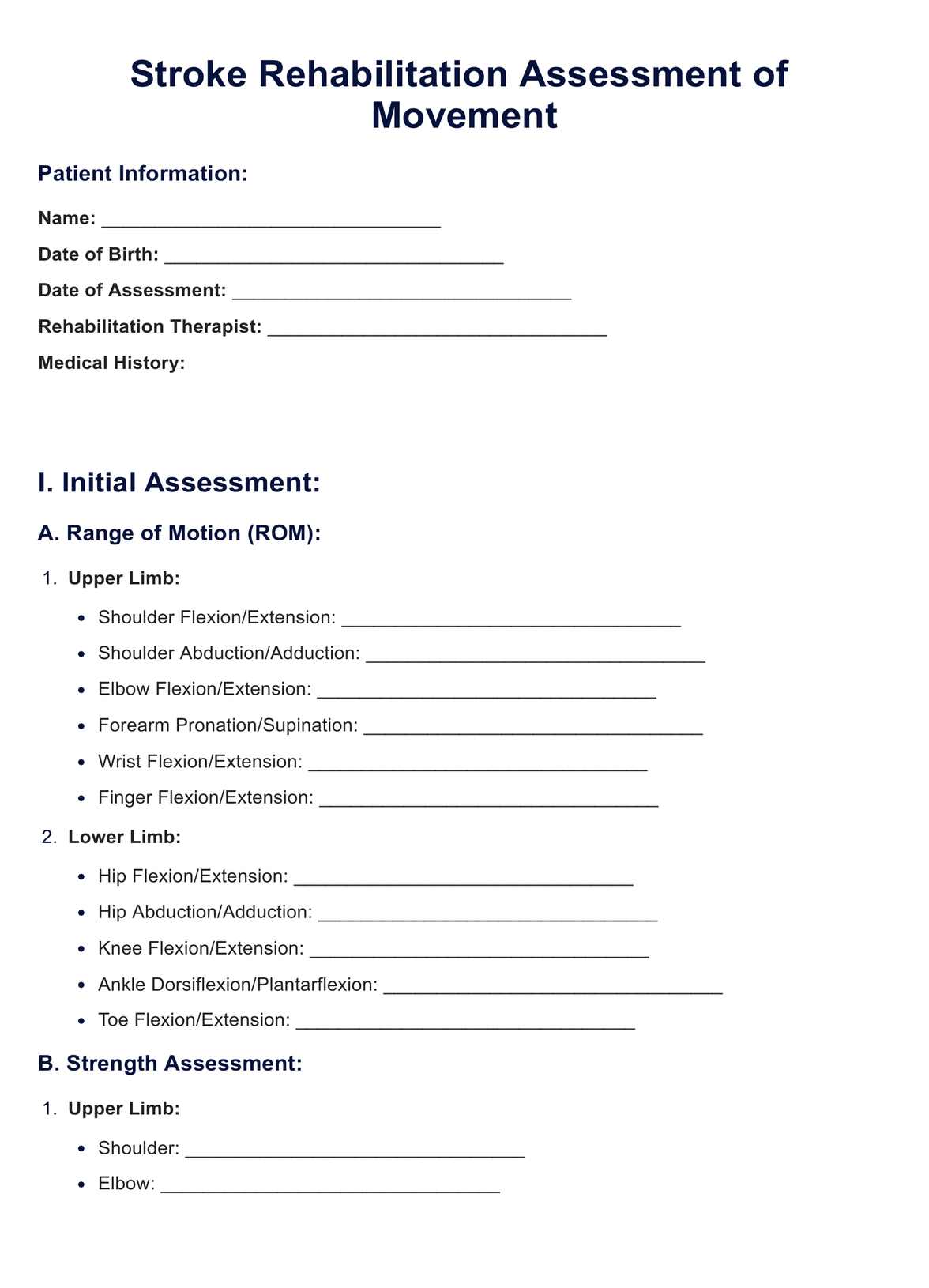
The Stroke Rehabilitation Assessment of Movement (STREAM) Template
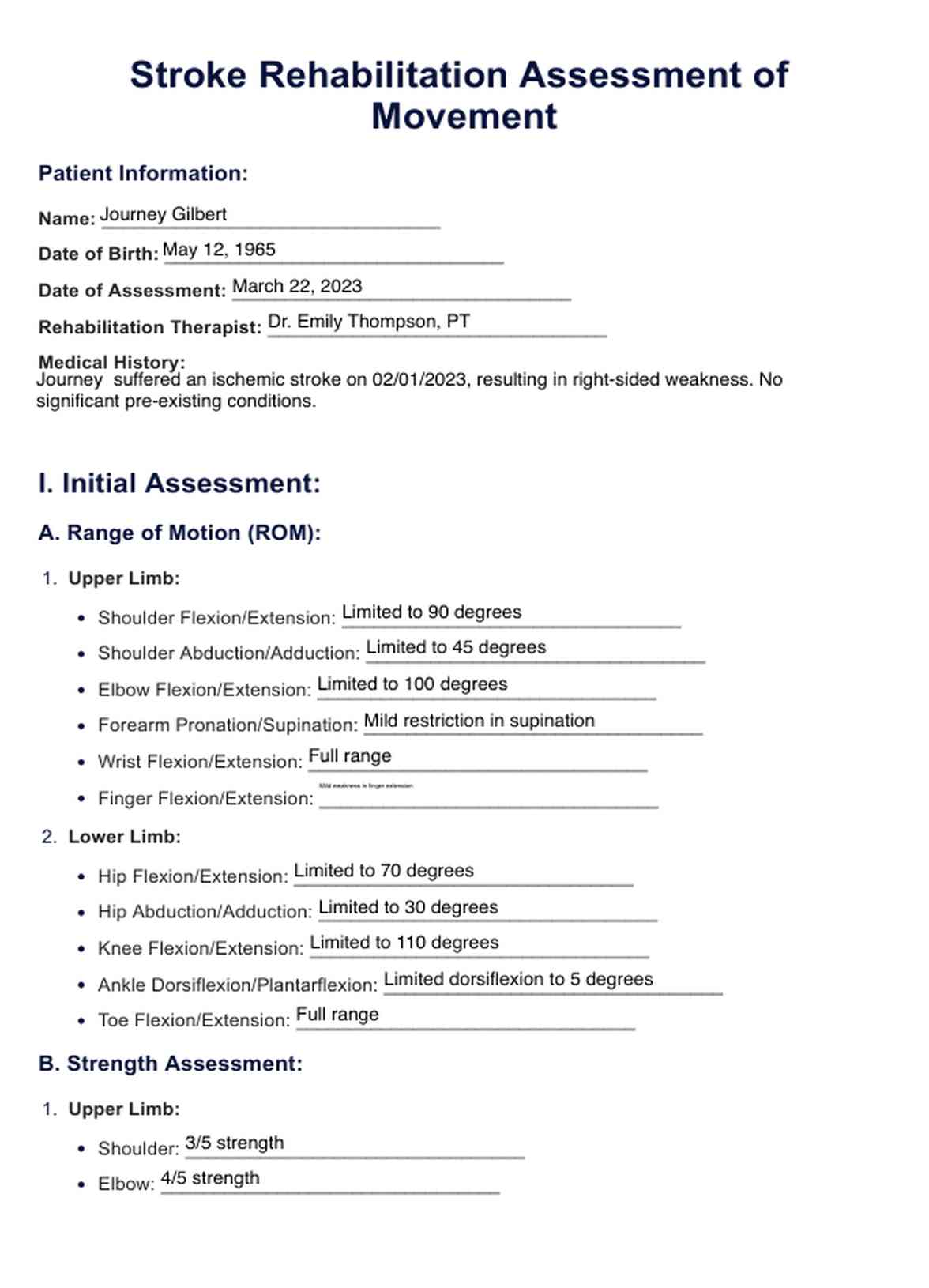
The Stroke Rehabilitation Assessment of Movement (STREAM) Example
When should this stroke rehabilitation assessment be administered?
The stroke rehabilitation assessment of movement is a critical tool that should be strategically administered at crucial points in the stroke rehabilitation journey.
To optimize its effectiveness, healthcare practitioners, including physical therapists, occupational therapists, and rehabilitation specialists, often leverage comprehensive templates like Carepatron's stroke rehabilitation assessment of movement.
This template is valuable for practitioners seeking streamlined, standardized approaches to assess stroke patients' progress.
Initial assessment and baseline measurement
The stroke rehabilitation assessment of movement is most commonly administered at the onset of rehabilitation. This initial assessment serves as a baseline measurement, providing practitioners with valuable insights into the extent of motor impairments and functional limitations.
Regular monitoring and progress tracking
Regular assessments are essential as rehabilitation progresses to track interventions' effectiveness and gauge stroke patients' improvement.
This ongoing assessment is crucial for making data-driven adjustments to the rehabilitation plan, ensuring it aligns with the evolving needs of the individual.
Transition points in rehabilitation
When transitioning between different phases of rehabilitation, such as moving from inpatient to outpatient care or adapting interventions based on changing goals, the stroke rehabilitation assessment of movement becomes instrumental.
Carepatron's template offers a comprehensive structure that supports practitioners in seamlessly transitioning assessment data, providing continuity in care, and promoting a holistic approach to acute stroke rehabilitation.
How to administer the assessment
Administering the stroke rehabilitation assessment of movement requires a systematic approach to ensure accuracy and consistency in evaluating motor function and overall functional mobility. Below are key steps to effectively conduct the assessment, incorporating crucial stream outcome measures for a comprehensive evaluation.
Pre-assessment preparation
Before initiating the assessment, gather relevant information about the individual's medical history, including the details of the acute stroke event. Ensure a suitable environment with adequate space and necessary equipment. Communicate with the patient, explaining the assessment process and addressing any concerns.
Initial patient evaluation
You can begin the assessment by initially evaluating the patient's baseline motor function. This involves observing the individual's posture, balance, and general mobility. Document any obvious impairments or asymmetries that may impact the assessment.
Muscular strength assessment
Evaluate muscle strength systematically, focusing on major muscle groups affected by the stroke. Utilize standardized measures, such as the Medical Research Council (MRC) scale, to quantify and document the strength of specific muscles. Record any weaknesses or asymmetries.
Range of motion assessment
Assess the range of motion in joints affected by the stroke, paying close attention to any restrictions or limitations. Utilize goniometers or inclinometers to measure joint angles accurately. Document any deviations from the expected range of motion.
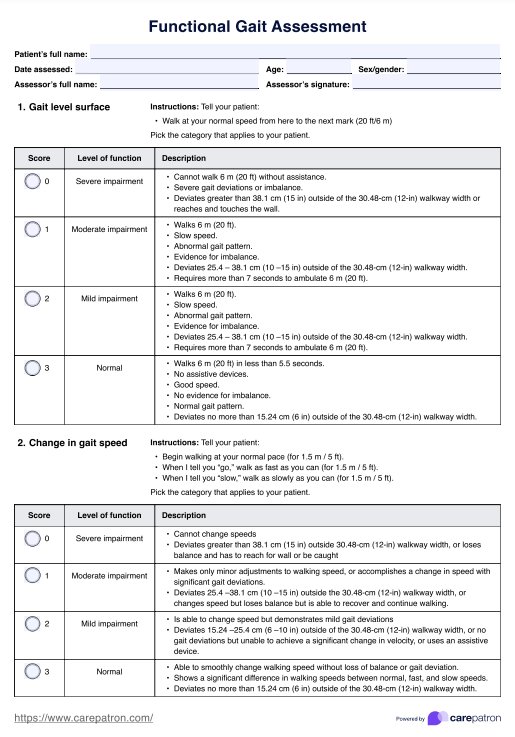
Balance and coordination assessment
Use standardized balance tests, such as the Berg Balance Scale or the Tinetti Balance Assessment, to evaluate the patient's balance and coordination. Observe the individual's ability to maintain equilibrium during static and dynamic activities. Document any signs of instability or imbalance.
Functional mobility assessment
Assess the patient's ability to perform functional tasks related to daily living. Include activities like walking, reaching, and grasping objects. Utilize outcome measures like the Timed Up and Go (TUG) test to quantify functional mobility and identify areas for improvement.
Post-assessment documentation
After you complete the assessment, please thoroughly document the findings, including objective measurements, observations, and any notable changes from the baseline evaluation. This documentation serves as a foundation for developing a personalized rehabilitation plan.
Interpreting the results
Upon completing the stroke rehabilitation assessment of movement, healthcare practitioners must interpret the results carefully to guide appropriate interventions. Below are common results and their implications:
Motor strength
Assessing muscle strength using standardized measures like the Medical Research Council (MRC) scale provides valuable insights. Weakness in specific muscle groups may indicate areas of impairment. Addressing these weaknesses through targeted exercises, as physical therapy prescribes, can improve overall motor function.
Range of motion
Evaluating joint range of motion is crucial, especially in acute stroke cases. Restricted range of motion may suggest muscle stiffness or joint contractures. Physical and occupational therapy interventions, including stretching exercises, can help enhance flexibility and restore optimal joint movement.
Balance and coordination
Results from balance assessments such as the Berg Balance Scale highlight an individual's ability to maintain stability during various tasks. Impaired balance and coordination may increase the risk of falls. Physical therapy interventions focus on exercises that improve balance and enhance overall coordination.
Functional mobility
Assessing functional mobility through a box and block test like the Timed Up and Go (TUG) provides insights into a patient's ability to perform daily activities. Difficulty in mobility tasks may indicate challenges in independence. Rehabilitation strategies, including gait training and task-specific exercises, aim to enhance functional mobility.
Overall outcome measures
In acute care hospital settings, assessing overall outcome measures helps gauge the effectiveness of rehabilitation interventions. Comparative analysis over time allows practitioners to track progress and make data-driven decisions. Collaborative efforts between physical and occupational therapy contribute to achieving optimal outcomes for stroke patients.
Improving the quality of life of stroke patients
Enhancing the quality of life for individuals who have experienced an acute stroke is a paramount goal in clinical practice, and physical therapy plays a pivotal role in achieving this objective.
The integration of streamlined outcome measures, such as the NIH Stroke Scale, Postural Assessment Scale, Chedoke McMaster Stroke Assessment, and simplified stroke rehabilitation assessments, is crucial in assessing the impact of stroke and tailoring rehabilitation interventions to improve overall well-being.
Optimizing functional independence
Physical therapy interventions, guided by comprehensive assessments like the NIH Stroke Scale, aim to optimize functional independence in stroke survivors. Addressing impairments identified in stream outcome measures ensures a targeted approach to regain lost abilities, promoting autonomy in daily activities.
Focusing on postural stability
The Postural Assessment Scale is instrumental in evaluating and addressing postural stability issues that may arise post-stroke. By identifying and targeting specific challenges through postural assessments, physical therapy interventions can enhance balance and reduce the risk of falls, contributing to an improved quality of life.
Tailored rehabilitation plans
The Chedoke McMaster Stroke Assessment aids in the creation of personalized rehabilitation plans. Identifying specific impairments using this assessment allows physical therapists to design interventions that directly address individual needs, fostering a more effective recovery process.
Simplified stroke rehabilitation assessment
The use of a simplified stroke rehabilitation assessment further streamlines the rehabilitation process. By simplifying assessments without compromising accuracy, practitioners can focus on efficient and targeted interventions, ensuring that the rehabilitation journey is effective and manageable for the patient.
Holistic approach to care
Improving the quality of life for stroke patients goes beyond addressing physical impairments. It involves adopting a holistic approach to care that considers individuals' emotional, social, and psychological well-being. Informed by a combination of outcome measures, physical therapy interventions contribute to a comprehensive, patient-centered rehabilitation strategy.
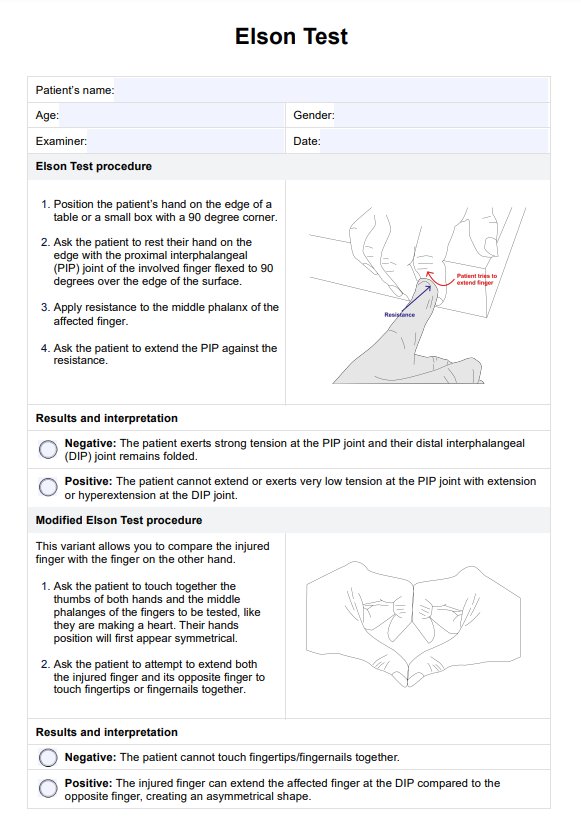
Other stroke rehabilitation assessments
In addition to the widely used assessments mentioned earlier, several others play a significant role in acute stroke rehabilitation within clinical practice and acute care hospital settings. These assessments provide valuable insights into various aspects of a stroke survivor's functional abilities and help guide rehabilitation strategies.
Box and block test
The Box and Block Test is a functional assessment that specifically evaluates manual dexterity and upper extremity coordination in stroke survivors. It involves moving blocks from one compartment to another within a set time frame.
This test provides clinicians with valuable information about a patient's ability to perform fine motor tasks, aiding in developing targeted rehabilitation interventions.
Predicting discharge destination
Specific assessments focus on predicting the most appropriate discharge destination for stroke patients. These assessments consider various factors, including functional independence and social support.
Predicting discharge destination is crucial in planning post-acute care and ensuring a smooth transition for patients from the hospital to rehabilitation or home.
Subscale stream scores
In stroke rehabilitation, subscale stream scores are often used to assess specific functional domains. These scores provide a detailed breakdown of a patient's mobility, self-care, and cognition performance.
Analyzing subscale stream scores allows for a more nuanced understanding of an individual's strengths and challenges, enabling targeted interventions.
Clinical outcome measures
Various clinical outcome measures are employed to assess the effectiveness of rehabilitation interventions. These measures include standardized assessments of mobility, balance, and activities of daily living.
Monitoring changes in clinical outcome measures over time helps healthcare practitioners gauge the progress of stroke patients and make informed decisions about the ongoing rehabilitation plan.
Supporting evidence for estimates
Several assessments involve estimating functional outcomes based on the patient's current status. These estimates often support these estimates and contribute to the overall rehabilitation plan.
Integrating evidence-based assessments ensures rehabilitation strategies are grounded in research and best practices, optimizing the chances of positive outcomes for stroke survivors.
To expand your resource pool and heighten client satisfaction, take a look at the NIH stroke scale, Outcome measures, Berg balance scale, Box and block test templates.
Research and evidence
The field of stroke rehabilitation has come a long way since its early beginnings. While helping stroke survivors regain function has been around for centuries, the development of standardized and objective methods for assessing movement impairments and progress is relatively recent.
One such tool, according to Physiopedia (2006), the Stroke Rehabilitation Assessment of Movement (STREAM), has significantly advanced stroke rehabilitation practice.
Records from ancient Egypt, Greece, and China indicate attempts to rehabilitate individuals with stroke-like symptoms as early as 3000 BC. These methods often involved massage, herbal remedies, and physical exercises.
During the 17th to the 19th century period, the understanding of stroke and its effects on movement improved significantly. According to Finger (2005), physicians like Thomas Willis and Jean-Martin Charcot contributed essentially to our knowledge of brain anatomy and function. However, rehabilitation methods remained largely empirical and lacked standardized assessment tools.
In the late 20th century, there was a growing emphasis on evidence-based practice in healthcare. This led to the development of several standardized outcome measures for stroke rehabilitation, including the STREAM.
According to the National Health Service (2017), a team of physiotherapists, psychologists, occupational therapists, speech and language therapists, dietitians, specialist nurses, and doctors developed the STREAM in the late 1980s. They recognized the need for a quick and easy-to-administer tool that could reliably assess movement impairments and track progress in patients with stroke.
The STREAM is unique in its focus on functional movement skills rather than isolated muscle strength or range of motion. This aligns with the overall goal of stroke rehabilitation, which is to help patients regain independence and quality of life.
References
Physiopedia. (2006). Stroke rehabilitation assessment of movement (stream). https://www.physio-pedia.com/Stroke_Rehabilitation_Assessment_of_Movement_(STREAM)Finger, S. (2005). Thomas willis: the functional organization of the brain. https://academic.oup.com/book/6739/chapter-abstract/150831441?redirectedFrom=fulltext
National Health Service UK. (2017). https://www.nhs.uk/conditions/stroke/recovery/#:~:text=A%20team%20of%20different%20specialists,and%20specialist%20nurses%20and%20doctors.
Commonly asked questions
The Stroke Rehabilitation Assessment of Movement systematically evaluates motor abilities and functional movement patterns in individuals recovering from a stroke. It involves standardized tests and measures to quantify impairments, guiding the development of personalized rehabilitation plans.
The physical assessment for a stroke patient involves evaluating muscle strength, range of motion, balance, and coordination. Physical therapists use this assessment to identify specific impairments and design targeted interventions to improve overall motor function.
The Stream Assessment aims to provide a streamlined and comprehensive evaluation of stroke patients' functional abilities. It focuses on key outcome measures, facilitating efficient data collection and contributing to developing personalized rehabilitation plans.