Pleural Effusion Nursing Care Plan
Learn the ins and outs of this disorder of the lungs and follow the guide to gain insight into its many causes and interventions!


What is a Pleural Effusion Nursing Care Plan?
A pleural effusion occurs when excess fluid accumulates in the pleural space—the area between the parietal pleura lining the chest wall and the visceral pleura covering the lungs. This fluid buildup can impair breathing by causing decreased lung expansion, leading to symptoms such as respiratory distress and absent breath sounds. The causes of pleural effusion can vary from infections to conditions like lung cancer or malignant pleural effusion.
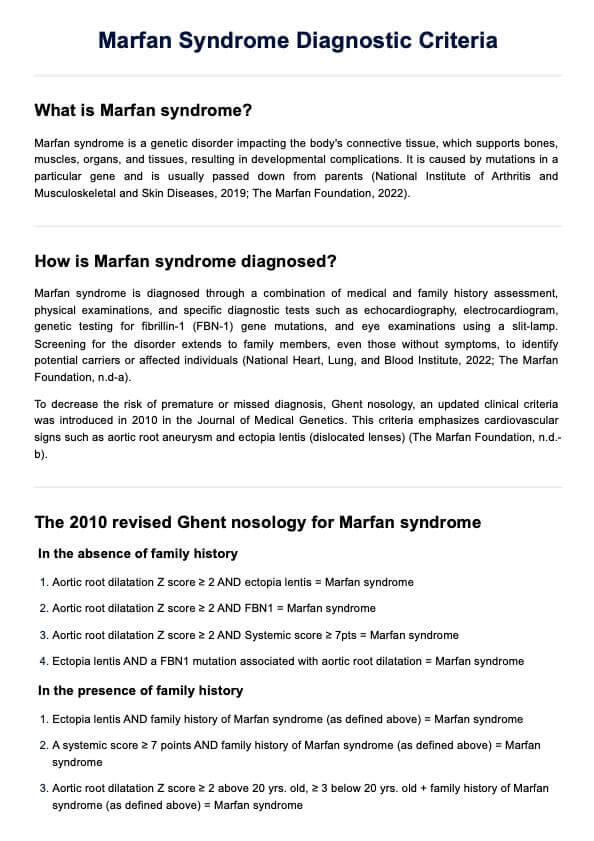
Pleural effusions are classified as transudative or exudative, based on the pleural fluid lactate dehydrogenase (LDH) and protein content, using the Light criteria. The fluid is considered exudative if specific criteria are met:
- A higher ratio of protein in the pleural fluid compared to blood serum.
- Elevated levels of lactate dehydrogenase (LDH) in the pleural fluid relative to serum LDH.
- Pleural fluid LDH exceeds two-thirds of the upper normal limit for serum LDH.
Transudative effusions are usually associated with systemic issues like heart failure or liver disease, while exudative effusions often result from infections, cancers, or inflammatory conditions. Identifying the correct type allows healthcare professionals to provide targeted treatment.
A nursing care plan helps clinicians systematically assess the patient’s respiratory function, monitor symptoms, and manage treatments. It includes setting clear goals and outcomes, planning interventions, and regularly evaluating patient progress. This structured approach ensures that individuals with pleural effusion, whether caused by infections, malignancies, or chronic diseases, receive comprehensive care tailored to improve their breathing and overall well-being.
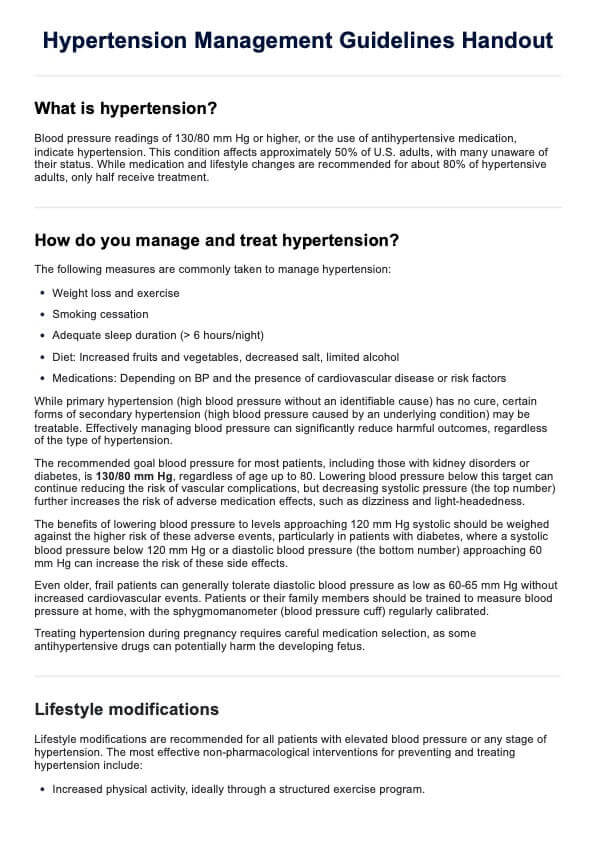
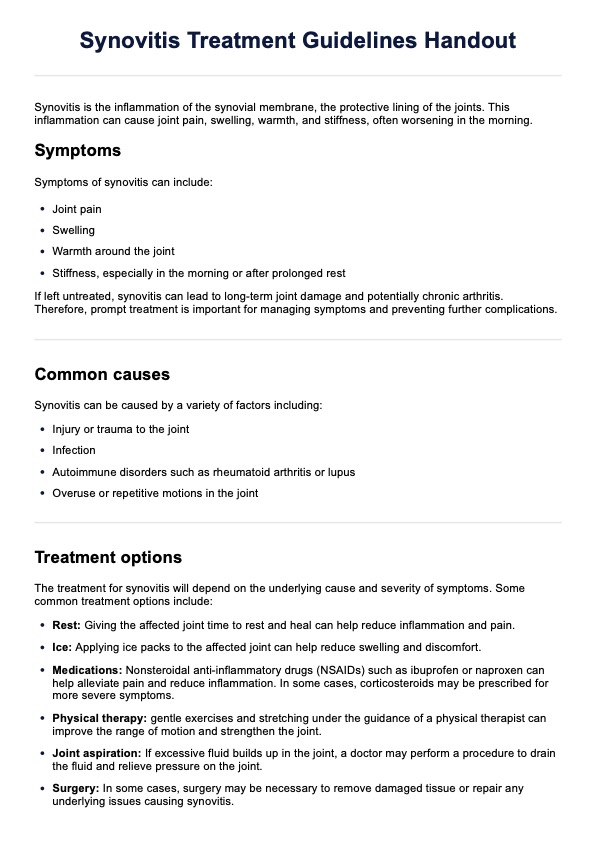
Pleural Effusion Nursing Care Plan Template
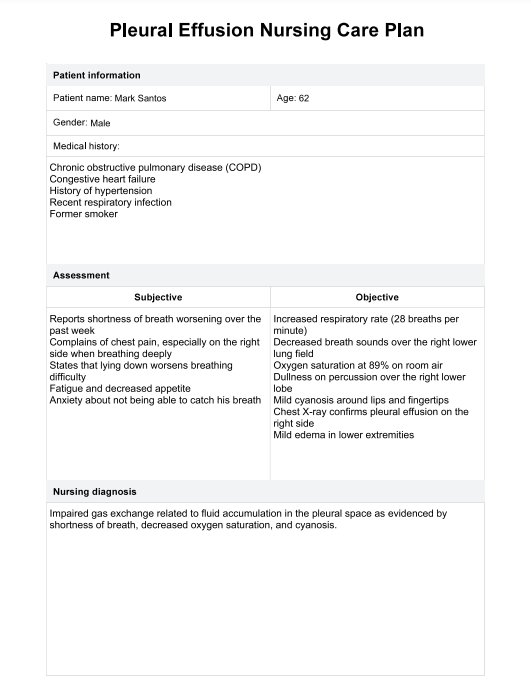
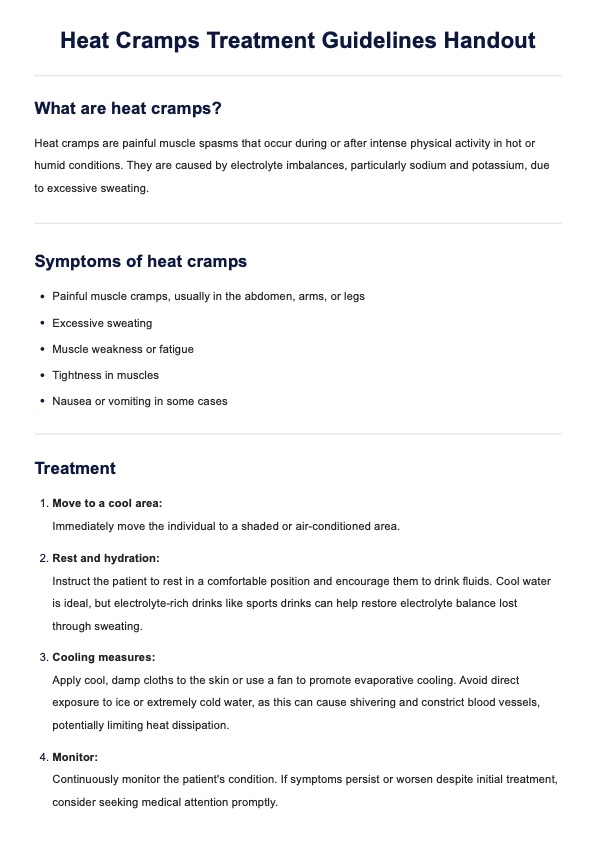
Pleural Effusion Nursing Care Plan Example
How to use our Pleural Effusion Nursing Care Plan template
Our Pleural Effusion Nursing Care Plan template provides empty fields that healthcare professionals can use to create a personalized care plan. It allows for documenting assessments, interventions, and outcomes efficiently. This template supports collaboration with patients and caregivers, promoting better communication and care outcomes.
Step 1: Access the template
Click the “Use template” button to open the template in the Carepatron app, where you can customize, share, and fill it. Alternatively, download a fillable PDF by clicking the “Download” button for offline use or printing.
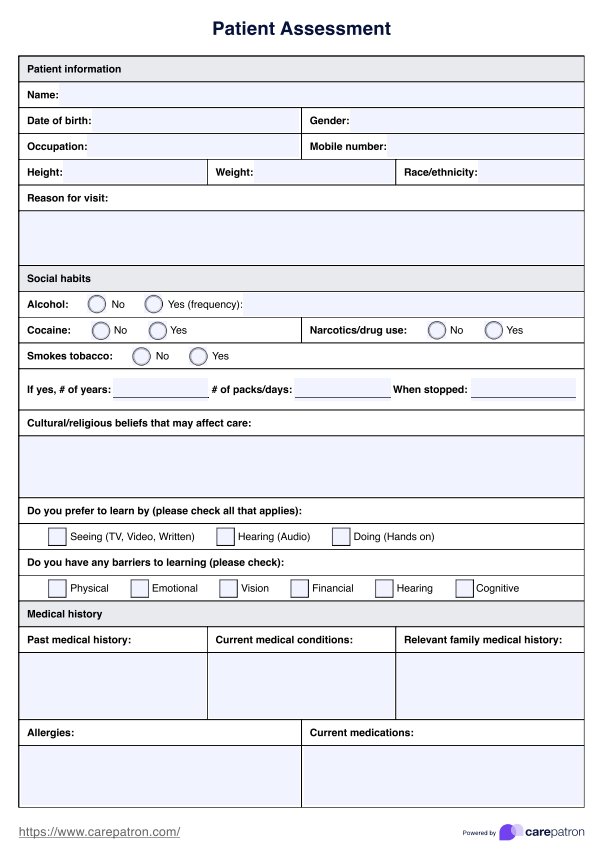
Step 2: Assess the patient
Conduct a thorough patient assessment by recording subjective and objective findings, such as respiratory patterns, oxygen levels, and lung sounds. Document these in the appropriate fields on the template, which ensures all relevant information is captured for diagnosis and planning.
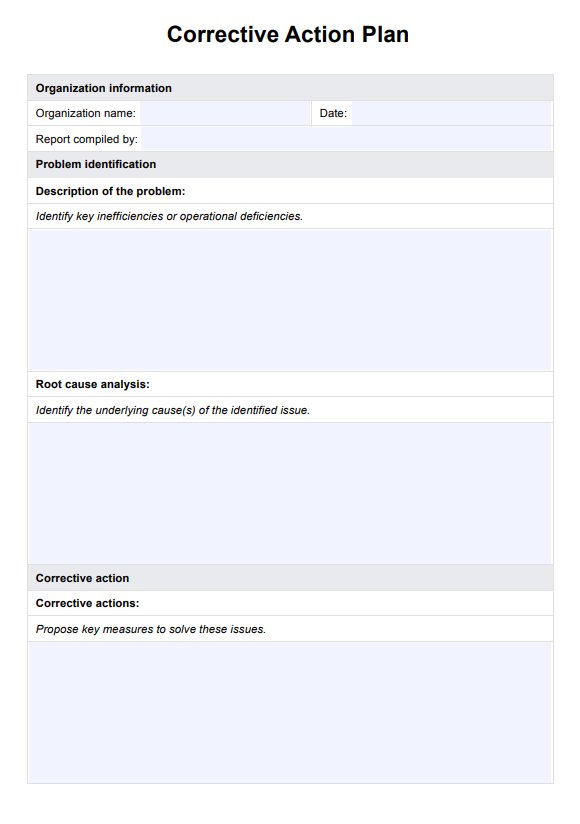
Step 3: Develop and implement interventions
Use the nursing interventions section to outline the care plan. Tailor interventions based on the patient’s condition, setting both short-term and long-term goals. Implement treatments such as thoracentesis, medication management, or therapeutic chest tube insertion as necessary.
Step 4: Discuss the plan and teach the patient
Share the care plan with the patient and their caregivers. Teach them how to follow through with necessary treatments, such as performing deep breathing exercises to prevent respiratory compromise. Empower the patient to take an active role in their recovery and monitor signs of worsening symptoms.
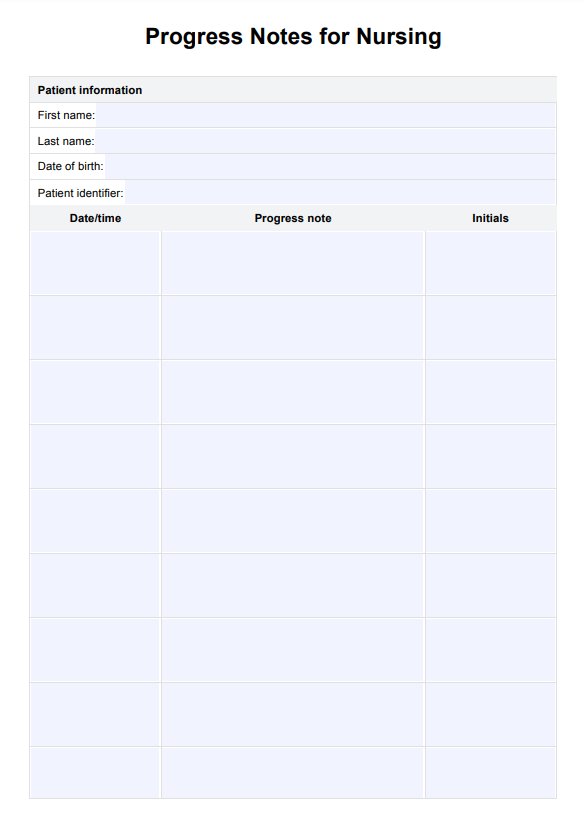
Step 5: Monitor progress and document outcomes
Evaluate the patient’s response to interventions, monitoring symptom relief, fluid levels, and respiratory function. Use the evaluation field to record progress or adjust the care plan. Secure the plan within Carepatron’s HIPAA-compliant system for easy access and collaboration among care team members.
When would you use this template?
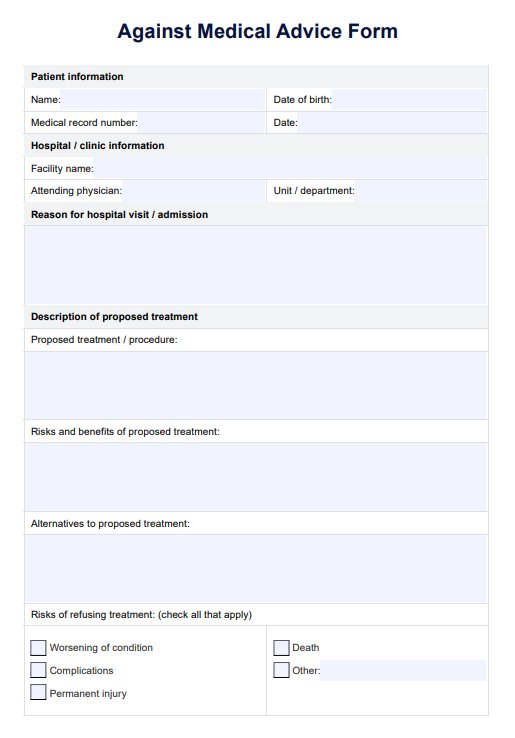
The Pleural Effusion Nursing Care Plan template is essential across various scenarios to ensure effective patient care. It supports newly diagnosed patients by providing education on their condition, helps hospitalized patients by guiding respiratory management and monitoring drainage systems, and assists with chronic or recurrent cases by enabling long-term symptom management. This template is also valuable for post-procedure care following thoracentesis or chest tube insertion, ensuring proper follow-up and minimizing complications. Additionally, it aids in managing coexisting conditions, such as heart failure or lung cancer, which often contribute to pleural effusion. In palliative care, it focuses on improving patient comfort and quality of life, while also offering educational resources to caregivers to enhance their involvement and care effectiveness.
Nursing interventions for pleural effusion
Managing pleural effusion requires targeted interventions to relieve symptoms, address the underlying cause, and prevent complications. Nursing interventions focus on improving respiratory function, reducing chest pain, and monitoring fluid levels to promote patient well-being and recovery. Below are key interventions that you can implement:
- Treat the underlying cause: Identify and manage the primary condition, such as heart failure, infection, or lung cancer, which may contribute to fluid buildup in the pleural space.
- Drainage through thoracentesis or chest tube insertion: Therapeutic thoracentesis helps remove fluid and relieve chest pain or shortness of breath. Chest tubes are often placed for continuous drainage in severe or recurrent cases.
- Antibiotics or antifungal treatment: Administer medications to treat infections causing exudative pleural effusions, such as bacterial pneumonia or tuberculosis.
- Tunneled pleural catheters: These catheters provide long-term drainage solutions for patients with malignant or chronic pleural effusions, improving comfort and reducing hospital visits.
- Surgical treatments: Interventions like pleurodesis, pleuroperitoneal shunts, or diaphragm defect repair may be necessary for complex or recurrent effusions that do not respond to less invasive methods.
- Dietary modifications: Instruct patients to reduce dietary fat intake in cases of chylothorax, a lymphatic leak causing fluid accumulation in the pleural space.
- Encourage deep breathing exercises: These exercises help prevent respiratory compromise and promote better lung expansion, reducing the risk of complications such as atelectasis.
- Monitor for signs of respiratory distress and infection: Regular assessments ensure early detection of complications like pleural thickening or empyema, allowing for timely medical intervention.
Research & evidence
Pleural effusion presents a broad spectrum of potential causes, with common culprits including congestive heart failure, cancer, pneumonia, and pulmonary embolism. A delayed diagnosis of its root cause can significantly elevate both morbidity and mortality rates, exemplified by instances where a parapneumonic effusion progresses to pulmonary empyema.
Non-malignant pleural effusions frequently signal a poor prognosis in patients dealing with cardiac, renal, or hepatic failure, with respective one-year mortality rates of 50%, 46%, and 25% (Walker et al., 2017).
Additionally, several rare diseases, mostly exudative in nature, are associated with pleural effusion. For instance, systemic lupus erythematosus sees a 30–50% prevalence of pleural effusion, termed "polyserositis," while diseases like granulomatosis with polyangiitis, rheumatoid arthritis, and Langerhans-cell granulomatosis also commonly present with pleural effusion (Anevlavis et al., 2012). A substantial portion (21.1%) of idiopathic and familial pulmonary hypertension cases exhibit pleural effusion, primarily unilateral (Tang et al., 2009).
Pulmonary embolism serves as a frequent yet unexplained cause of pleural effusion, present in 20–55% of cases. The severity of the embolism and the occurrence of pulmonary infarction align with the frequency of pleural effusion in these instances. Despite the relatively small effusion volume, patients often experience severe dyspnea (Choi et al., 2017). The importance of a multifaceted nursing care plan that covers multiple conditions at once to provide a clear overview is key.
References
Anevlavis, S., Tzouvelekis, A., & Bouros, D. (2012). Mechanisms of pleural involvement in orphan diseases. Respiration, 83(1), 5–12. https://doi.org/10.1159/000335128
Choi, S. H., Cha, S.-I., Shin, K.-M., Lim, J.-K., Yoo, S.-S., Lee, S.-Y., Lee, J., Kim, C.-H., Park, J.-Y., & Lee, D. H. (2017). Clinical relevance of pleural effusion in patients with pulmonary embolism. Respiration, 93(4), 271–278. https://doi.org/10.1159/000457132
Tang, K., Robbins, I. M., & Light, R. W. (2009). Incidence of pleural effusions in idiopathic and familial pulmonary arterial hypertension patients. Chest, 136(3), 688–693. https://doi.org/10.1378/chest.08-0659
Walker, S. P., Morley, A. J., Stadon, L., De Fonseka, D., Arnold, D. T., Medford, A. R. L., & Maskell, N. A. (2017). Nonmalignant pleural effusions. Chest, 151(5), 1099–1105. https://doi.org/10.1016/j.chest.2016.12.014
Commonly asked questions
Nursing interventions focus on treating the underlying cause, draining excess fluid through thoracentesis or chest tube insertion, and administering antibiotics if infection is present. Other treatments include tunneled pleural catheters for chronic effusions, pleurodesis or surgery for recurrent cases, and dietary changes for chylothorax. Nurses also teach patients breathing exercises and monitor for signs of respiratory compromise and infection.
Teach patients to perform deep breathing exercises to enhance lung expansion and prevent respiratory compromise. Educate them about recognizing early signs of fluid accumulation, infection, and complications, ensuring medication adherence, and understanding how to manage drainage systems if required.
Related NANDA-approved diagnoses include impaired gas exchange, excess fluid volume, and ineffective breathing pattern. Nurses can also incorporate diagnoses like anxiety and knowledge deficit if the patient experiences distress or lacks information about managing the condition.