It can take between 15 to 30 minutes. Since you'll likely assess children with functional balance problems, it might take longer than that.
Pediatric Balance Scale
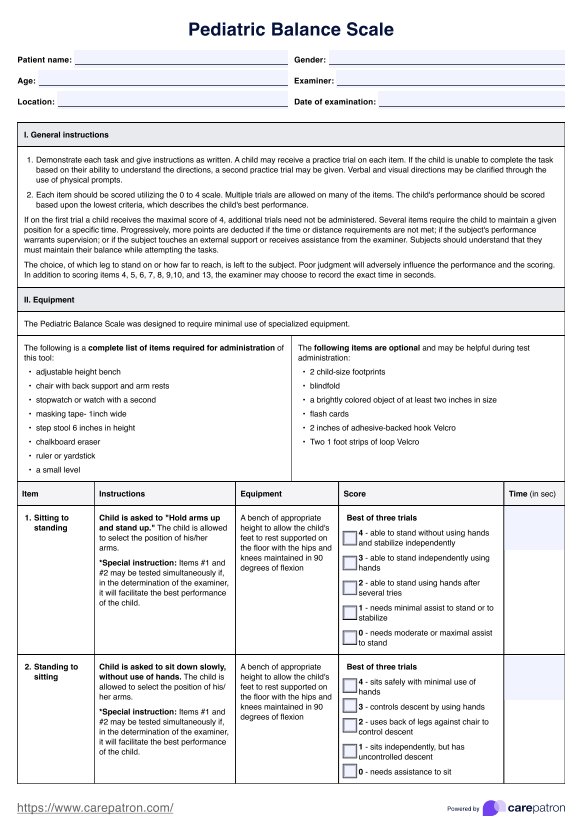
Get the Pediatric Balance Scale template to assess children's balance skills. Track progress and support better motor development with this easy-to-use tool!
Use Template
Pediatric Balance Scale Template
Commonly asked questions
Since the Pediatric Balance Scale is composed of several balance exercises, there is a risk of falling. Having someone other than yourself who can provide support and immediately catch the child if they show signs of decreasing is essential.
The pilot testing of the scale involved children between the ages of five and fifteen, so fifteen can be your limit. For those older than fifteen, you can use the Berg Balance Scale.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











