To collect comprehensive data about a patient's medical history and current health status, guiding diagnostic and treatment decisions.
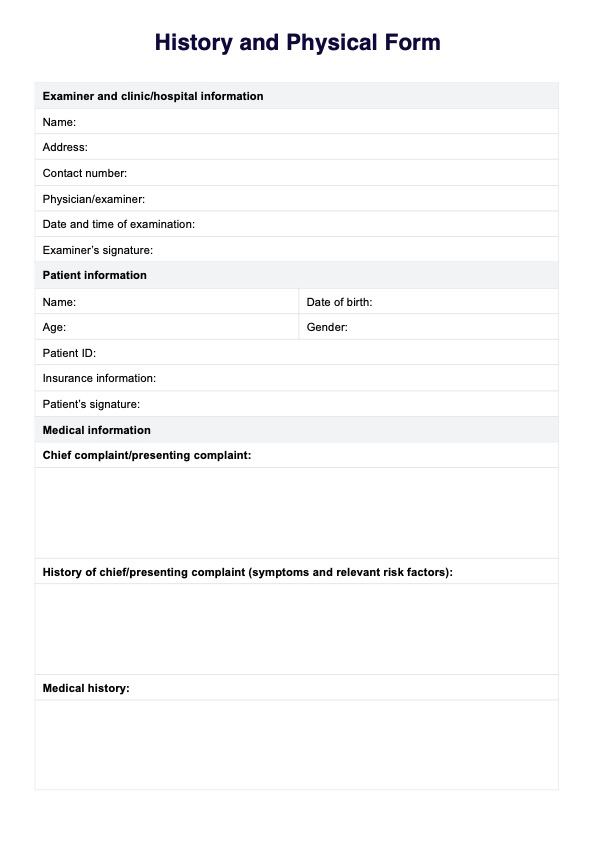
Streamline patient assessments with our History and Physical Form for accurate diagnosis and effective care management.
To collect comprehensive data about a patient's medical history and current health status, guiding diagnostic and treatment decisions.
It refers to the medical terminology and processes involved in taking a patient's medical history and conducting a physical examination.
It includes patient demographics, medical, family, and social history, a review of systems, and physical examination findings.
EHR and practice management software
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments