Pulmonary Embolism Nursing Care Plan
Use our Pulmonary Embolism Nursing Care Plan Template for planning and managing the care of a patient with a pulmonary embolism.


What is a Pulmonary Embolism Nursing Care Plan Template?
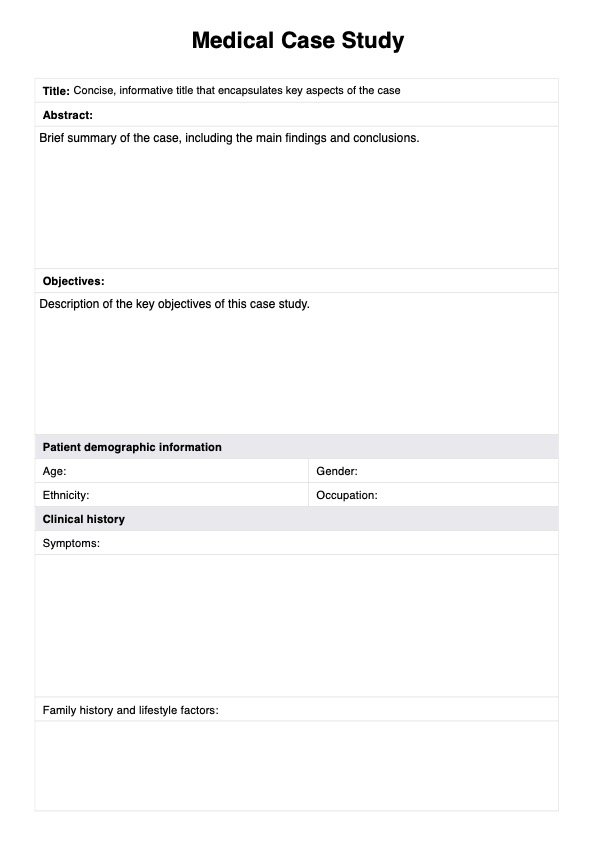
A pulmonary embolism (PE) occurs when a blood clot blocks at least a pulmonary artery or several of them in the lungs, impeding pulmonary arterial blood flow. This blockage, often originating from deep vein thrombosis (DVT), also known as deep venous thrombosis, poses a life-threatening risk, leading to symptoms such as chest pain, difficulty breathing, and altered blood pressure. Acute pulmonary embolism may cause pulmonary infarction, where lung tissue becomes damaged due to lack of oxygen.
The nursing care plan for PE serves as a structured guide for managing patients with this condition. It helps you develop individualized care plans, addressing symptoms and potential complications like bleeding risk and ventilation perfusion issues. The plan includes comprehensive assessments and interventions to improve pulmonary arterial blood flow and mitigate venous thromboembolism.
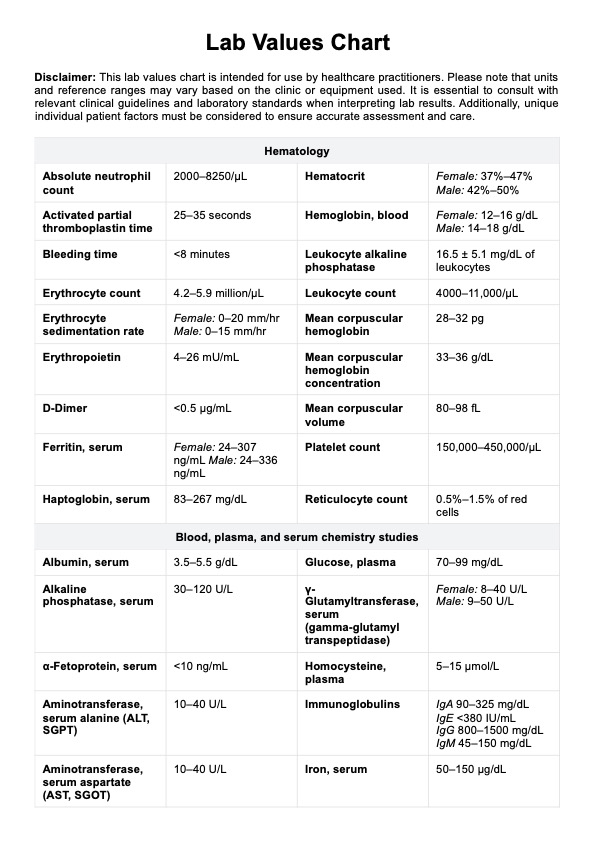
This template also facilitates early identification of increased risk factors for PE and helps monitor the patient's respiratory status. Nurses may use diagnostic tools and assessments, such as computed tomography, pulmonary angiography, or a ventilation-perfusion scan, to confirm PE and design targeted care plans. This ensures that you can have timely interventions to optimize patient outcomes and prevent complications.
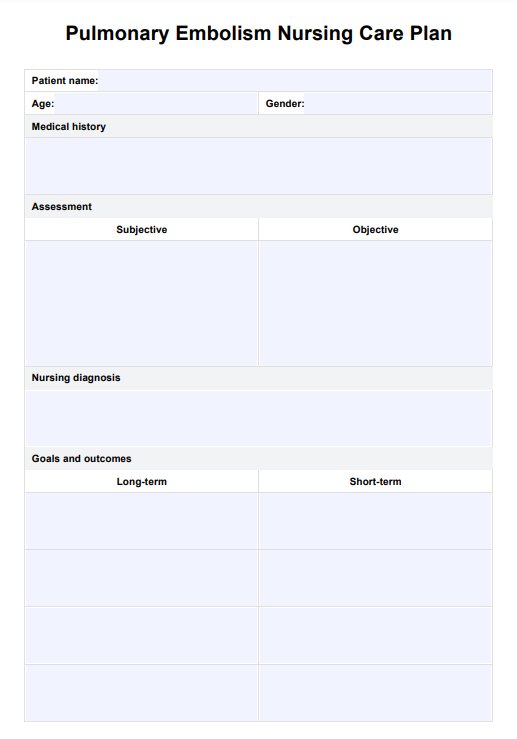
Pulmonary Embolism Nursing Care Plan Template
Pulmonary Embolism Nursing Care Plan Example
How to use our Pulmonary Embolism Nursing Care Plan Template
Our template offers healthcare professionals a comprehensive guide for planning personalized care. With sections for documenting assessments, interventions, and outcomes, it supports the coordinated management of pulmonary embolism (PE). Here’s how to use it effectively:
Step 1: Access the template
Click the “Use template” button in the Carepatron app to customize and fill out the document digitally. Alternatively, you can click “Download” for a non-customizable but fillable and printable PDF version.
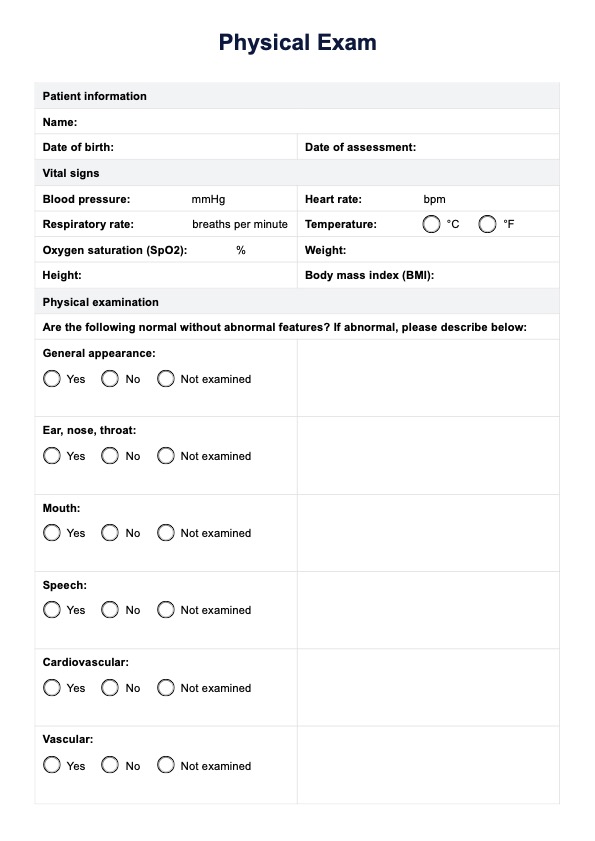
Step 2: Assess the patient
Begin by recording subjective and objective observations of the patient’s condition. Monitor symptoms such as difficulty breathing and chest pain while evaluating vital signs like blood pressure and respiratory status. Tools like computed tomography, pulmonary angiography, or a ventilation-perfusion scan can assist in diagnosing PE.
Step 3: Develop a care plan
Based on the assessment, create short-term and long-term goals. Address risk factors like deep vein thrombosis (DVT) and establish measurable interventions to manage symptoms and prevent complications. Document the selected treatments and educational efforts to reduce the patient's risk of recurrence.
Step 4: Engage the patient
Explain the care plan to the patient and their family, highlighting preventive measures and treatment strategies. Ensure they understand the importance of monitoring symptoms and following the care plan.
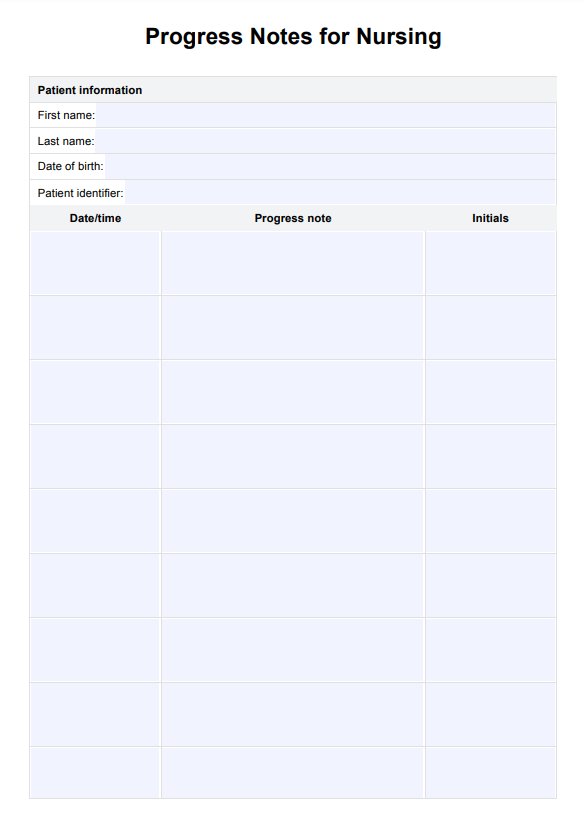
Step 5: Evaluate outcomes
Use the evaluation section to track progress over time, adjusting the care plan as necessary. This step allows healthcare professionals to assess the effectiveness of risk factor reduction strategies and treatments, ensuring improved patient outcomes.
Nursing diagnoses for pulmonary embolism
Nursing diagnoses are essential for identifying the needs and risks associated with pulmonary embolism (PE). These NANDA-approved diagnoses help healthcare professionals develop targeted care plans for optimal patient outcomes. Below are relevant diagnoses:
- Impaired gas exchange: Caused by blocked pulmonary arterial blood flow, reducing oxygenation.
- Ineffective breathing pattern: Related to difficulty breathing or hyperventilation due to anxiety or hypoxia.
- Decreased cardiac output: This results from ventricular failure or impaired circulation caused by the embolism.
- Risk for bleeding: Associated with anticoagulation therapy or thrombolytic therapy, which increases bleeding risk.
- Anxiety: Related to uncertainty about health and the life-threatening nature of the condition.
- Activity intolerance: Due to reduced blood pressure and oxygen supply affecting energy levels.
A nursing diagnosis for pulmonary embolism will form the foundation for patient-centered care, guiding interventions to improve pulmonary blood flow and overall respiratory status.
Nursing interventions for a pulmonary embolism patient
Nursing interventions for patients diagnosed with pulmonary embolism (PE) focus on improving respiratory function, restoring pulmonary blood flow, and preventing further blood clot formation. Below are essential interventions:
- Administer supplemental oxygen and oxygen therapy: Provide supplemental oxygen to improve blood oxygen levels and support respiration. Oxygen therapy ensures better oxygenation by compensating for impaired airflow through the pulmonary arteries.
- Monitor and support cardiac function: Assess for signs of ventricular failure by monitoring heart rate, blood pressure, and ECG readings. This ensures early detection and management of heart strain caused by blocked blood vessels in the lungs.
- Initiate anticoagulation therapy: Administer low molecular weight heparin or other anticoagulant therapy to prevent new blood clots from forming. This helps reduce the risk of further embolism and supports long-term management of the condition.
- Administer thrombolytic therapy for severe cases: In life-threatening cases, thrombolytic therapy may be used to dissolve existing clots within the pulmonary arteries. Close monitoring is necessary due to the increased bleeding risk associated with this treatment.
- Educate patients on medication and lifestyle changes: Teach patients about their prescribed anticoagulation therapy and necessary lifestyle adjustments to prevent clot recurrence. Encourage physical activity within safe limits to improve circulation and reduce the likelihood of future clots.
When combined, these interventions aim to restore pulmonary blood flow, enhance breathing, and prevent complications, improving the outcomes for patients with PE.
Commonly asked questions
Nurses play a crucial role in monitoring vital signs, administering medications like anticoagulation therapy, and providing oxygen therapy. They also educate patients on managing their condition, recognizing warning signs, and preventing further blood clot formation.
The primary focus is on stabilizing the patient's respiratory status, preventing additional blood clots, and maintaining pulmonary blood flow. Nurses also assess for potential complications, such as ventricular failure, and provide emotional support to reduce patient anxiety.
Nursing goals include restoring optimal oxygenation through supplemental oxygen, preventing the recurrence of PE with anticoagulant therapy, and ensuring the patient understands their treatment plan. Additional goals involve managing blood vessels' health and preventing ventricular failure for better long-term outcomes.