Head Injury Assessment
Experienced a head injury? Make sure you complete our Head Injury Assessment for early diagnosis for effective management.


What is a Head Injury Assessment?
Head injuries are common and can manifest in many different ways. Whether through sporting contests, motor vehicle accidents, or a simple fall, it is essential that these injuries be assessed early to determine the extent and effects of the injury. This information is critical to early intervention and developing effective treatment programs to protect the individual from further harm.
Completing a thorough injury assessment promotes accurate diagnosis of the level of trauma, can help prevent secondary injuries, and reduces risk factors of functional impairments related to brain injuries and skull fractures. Using our Head Injury Assessment, healthcare professionals have an invaluable resource to check a patient's condition following head trauma.
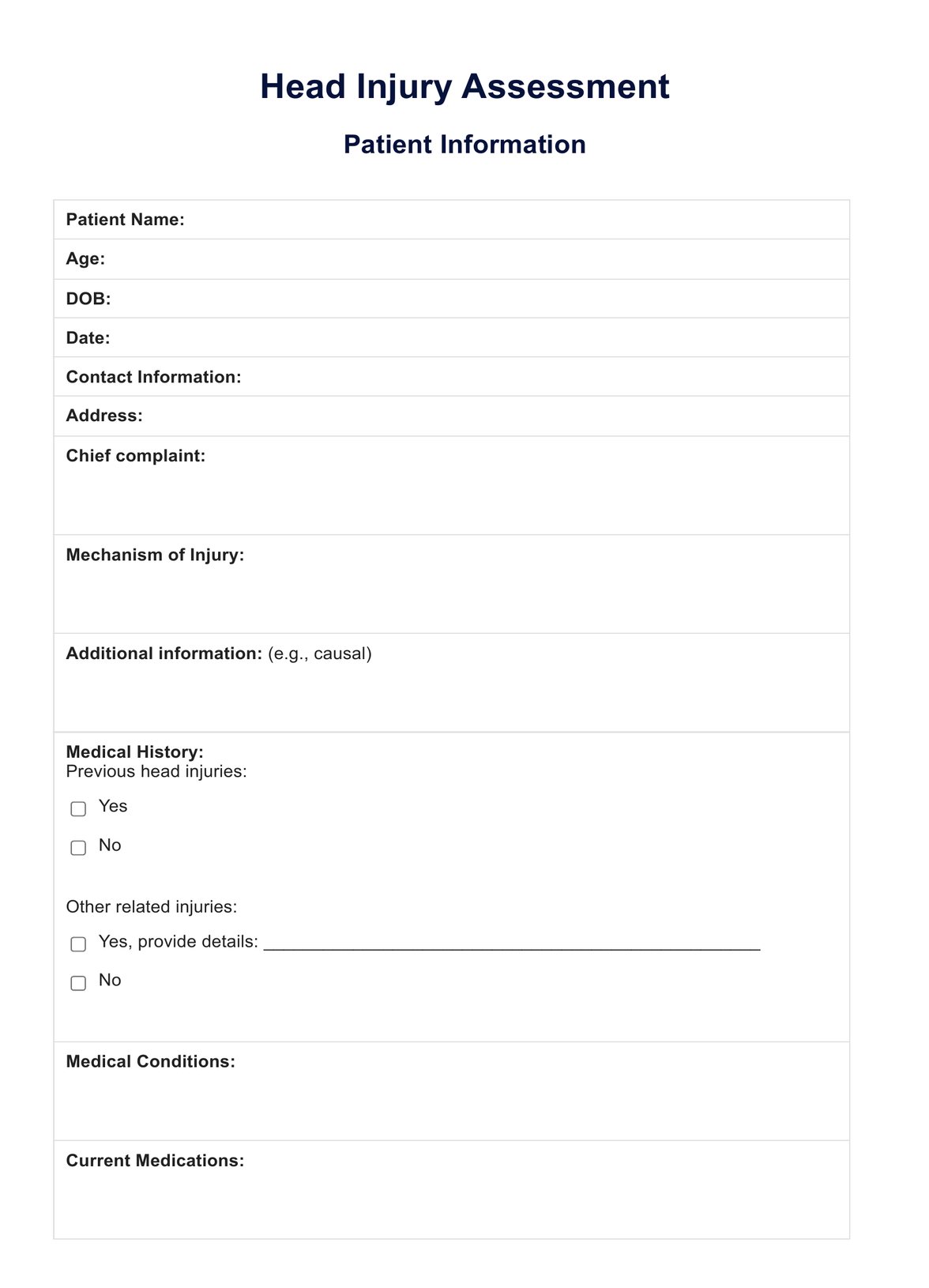
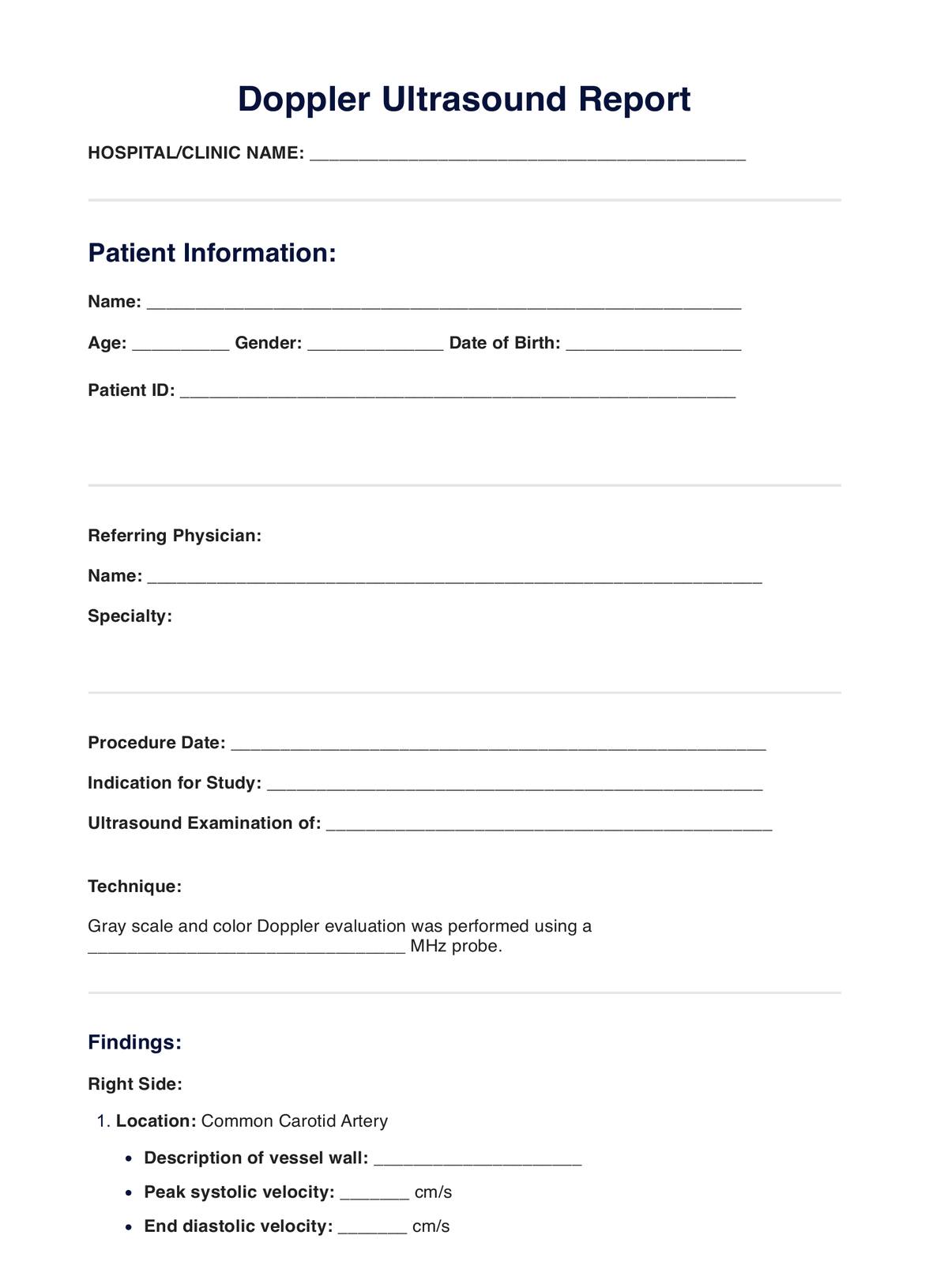
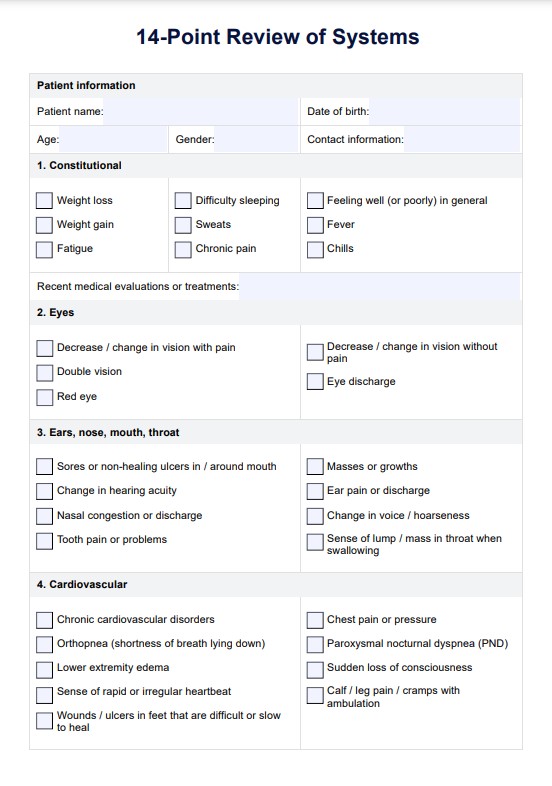
The assessment begins by collecting patient information, current medications, and medical history to provide context to the injury, which is critical for an accurate diagnosis. Professionals then complete an initial assessment of the following:
- Completing a Glasgow Coma Scale (GCS) score - patients are assessed for their eye, verbal, and motor responses. These are scored at the beginning and every 30 to 60 minutes of admission.
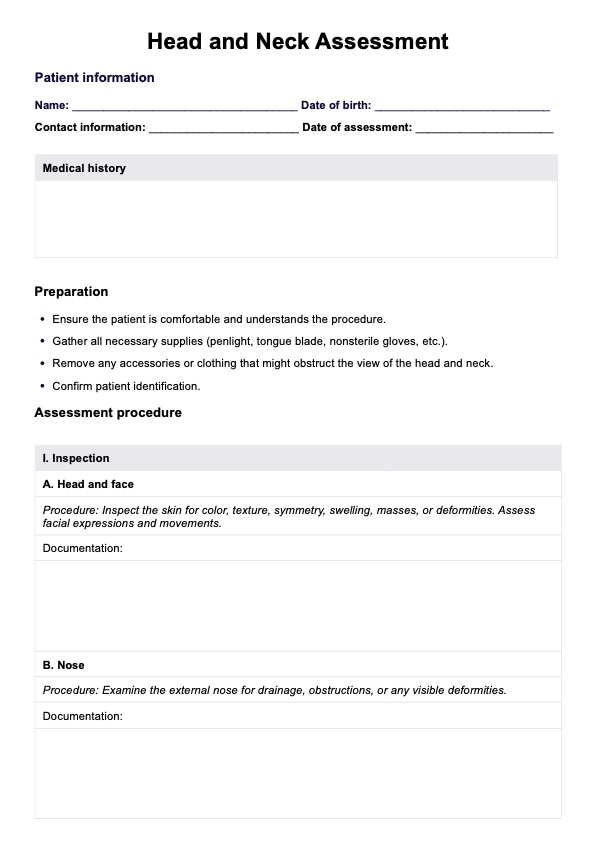
- Cervical spine - assess if there is any spinal injury or need for immobilization.
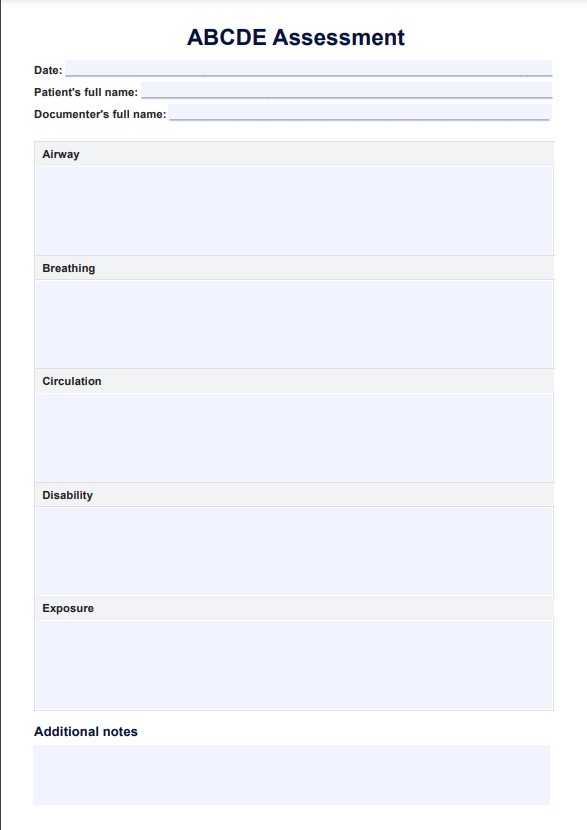
- Airways - appraising whether the patient can sustain their airway or requires an anesthetic team.
- Breathing - ensuring the patient has adequate ventilation and oxygenation.
- Circulation - ensuring accurate tissue perfusion, using resuscitation and fluids where appropriate.
- Disability and neurological examination - assess the patient's GCS, blood glucose, pupils, and a complete neurological examination for a focal neurological deficit.
- Exposure - examining whether the patient has any basal skull fracture, open or depressed skull fractures, lacerations, facial fractures, or penetrating injuries.
These are followed by imaging tests, documentation of the injury history, and a direct referral to neurosurgery if required.
As an essential resource, healthcare centers, such as emergency departments and intensive care units, can quickly implement this template into their protocols, allowing for optimal health and care for their patients.
Head Injury Assessment Template
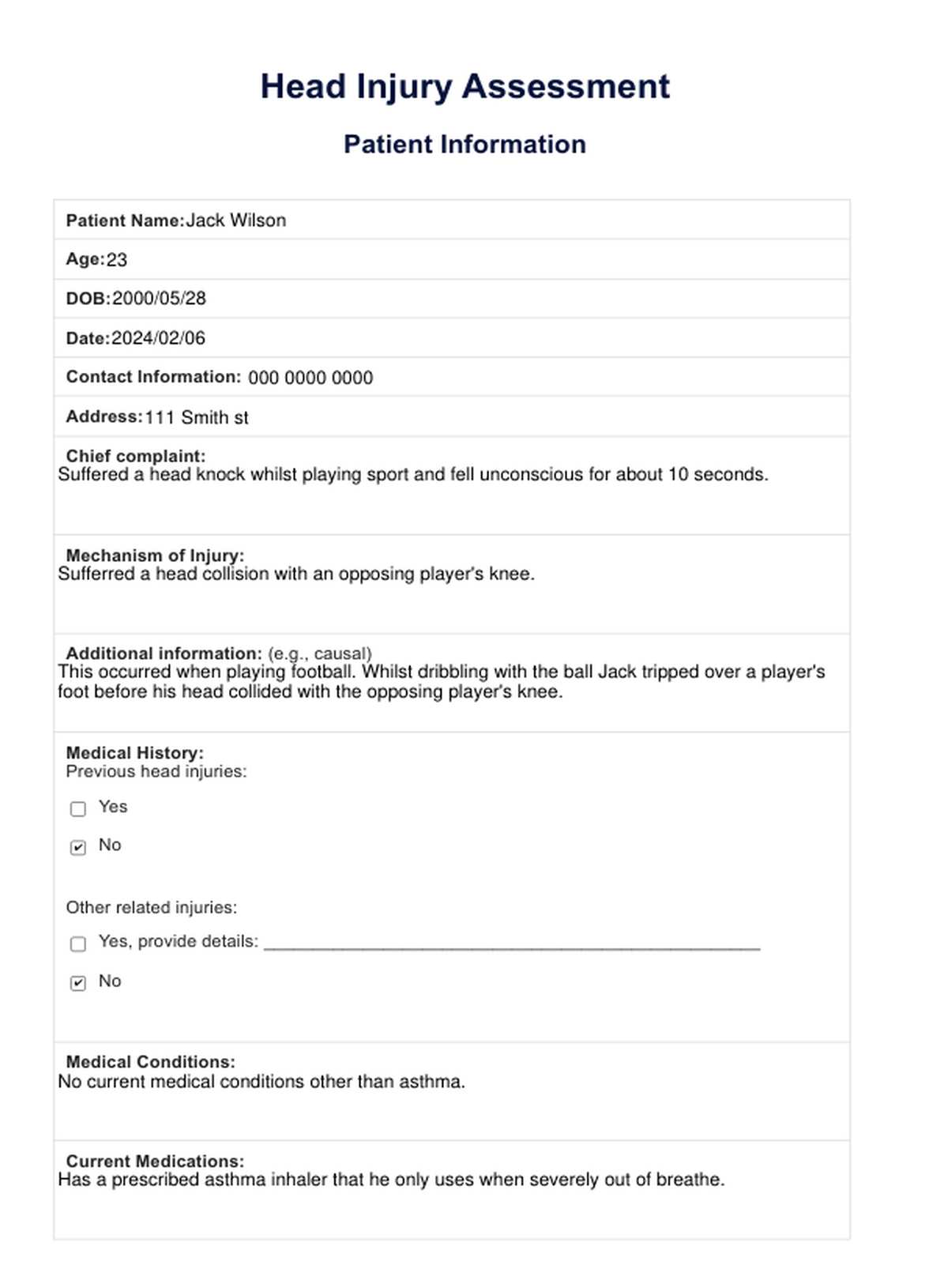
Head Injury Assessment Example
How does it work?
Our free Health Injury Assessment provides a structure that can be seamlessly integrated into practice protocols. To show you how this assessment works in practice, we have broken down the process into the following steps:
Step 1: Access the resource
You can find the resource here or download the PDF version to print a physical copy by using the link below:
Download the free Head Injury Assessment PDF here.
Step 2: Patient admission
Patients should be assessed within 15 minutes of their arrival, and any patients who present any signs in the 'take immediate action' section should be given immediate medical attention.
Step 3: Generate a Glasgow Coma Scale (GCS) score
Using the table in the resource, generate the patient's GCS score upon admission and continue updating the score every 30 to 60 minutes following admission.
Step 4: Initial assessment
Following the guidelines of the initial assessment, complete procedures for the cervical spine, airways, breathing, circulation, disability and neurological examination, and exposure responses.
Step 5: Complete imaging
If required, complete imaging procedures such as a CT scan to detect any brain bleeding disorders, skull fractures, or other injuries. Within this process, it may also be beneficial to complete other diagnostic testing, such as assessments for concussion symptoms and brain function.
Step 6: Document injury information
Complete the patient's injury information and update their medical history when appropriate. This is crucial to inform future injury assessments, treatment procedures, and diagnoses.
Step 7: Referrals and next steps
Using the guidelines in the resource, determine whether the patient requires an MRI scan or a referral for neurosurgery and develop a treatment and recovery plan.
Step 8: Ongoing monitoring
Assessing the patient's health status, including their injury status and brain function, is essential. Following discharge, provide discharge advice and schedule appointments to continue monitoring.
Results of a Head Injury Assessment
Given that head injuries can manifest in different ways, results from our free Head Injury Assessment can differ amongst patients by several individual factors. These include the level of intracranial pressure, level of head injury, if there were other injuries, or whether there was drug or alcohol intoxication involved.
Although this assessment is not a proper diagnostic procedure, it can provide a preliminary diagnosis and results for the following:
- Mild head injury: Individuals may have a mild head injury that causes headaches, fatigue, or pain. While these are mild, it is still essential to receive health advice from a registered professional to mitigate symptoms and reduce risk factors for further injury.
- Mild traumatic brain injury (TBI): Patients may be pre-diagnosed with a mild TBI that may cause temporary pain and changes in the brain cells or brain tissue. These injuries may require further assessment through a CT scan to determine the full extent of the injury, as there may be underlying issues.
- Potential skull fracture: Individuals may have a basal skull fracture or other skull injury following a severe head injury. Patients with this level of head injury may require further assessment to appraise the level of the fracture and require care from intensive care unit professionals or primary trauma services.
- Focal neurological deficit: During the disability and neurological examination portion of the initial assessment, health practitioners may find the patient has a focal neurological deficit. This may result from a brain tissue, nerve, or spinal injury.
When should an assessment be conducted?
Following a head injury
, Whether a penetrating head injury or following head trauma, it is essential to conduct a Head Injury Assessment. Doing so can provide assessment and early management of further injury related to brain function or the skull itself, such as traumatic brain injuries or skull fractures.
Following loss of consciousness
If a patient has experienced loss of consciousness following a brain injury, the patient must receive appropriate medical attention and an assessment as soon as it is appropriate to do so. Completing an assessment may assist in finding the cause of the episode and promote referrals for diagnostic tests and treatments.
Persistent symptoms
Individuals experiencing persistent headaches or migraines may require an assessment to assess for any traumatic brain injuries. It is essential to complete a head injury assessment alongside other diagnostic procedures, as symptoms may be a result of an underlying head or brain injury, such as brain blood clots. Furthermore, prolonged symptoms can risk scarring to brain tissue or further injury.
Behavior changes
Individuals experiencing changes in their behavior, for instance, in concentration levels, mood, or mental status. These may be a result of an unknown head injury, such as a mild head injury or severe traumatic brain injury (TBI).
Coma patients
When patients have entered a coma state, emergency departments, trauma units, and related individuals need to complete an assessment. This can help identify the source of the coma, such as a diffuse axonal injury, while also indicating brain function.
Who may use this assessment?
Our free Head Injury Assessment is an invaluable resource to guide accurate appraisal of the severity, symptoms, and type of injury. Given the broad applicability of this assessment, it can be used by various professionals involved in the appraisal of the injury. While the ability of professionals to conduct a complete evaluation depends on their access to specific equipment, initial appraisals such as GCS can be conducted from almost anywhere and at any time, depending on the individual's knowledge of the examination.
The following are some practitioners that typically use the assessment:
- Emergency department professionals: Individuals facing severe head injuries are usually admitted to the emergency department for further appraisal and immediate management. Emergency departments typically have all or most of the equipment required for an assessment, allowing for a thorough appraisal and management of the injury.
- Paramedics: Paramedics are usually one of the first on the scene of an accident and are often responsible for preliminary care and patient diagnoses. Depending on the patient's stability, paramedics may be able to conduct a full assessment, which they can then pass on to receiving health professionals.
- Major trauma centers: Patients who may have a significant traumatic brain injury may be assessed by major trauma centers. Professionals at these centers usually conduct a full assessment to determine the severity of the injury, alongside brain function tests.
- School nurses: A non-accidental injury at school can often lead to severe head injuries. The school nurse may initially assess a student to determine the type of care they require until emergency services arrive.
Commonly asked questions
A Head Injury Assessment is conducted following head trauma or symptoms that may be related to a head or brain injury. Typical instances in which this occurs include the following: loss of consciousness, behavior changes, head impact, or behavior changes.
Results following an assessment are multi-faceted and experienced differently depending on individual factors. Preliminary results from a Head Injury Assessment may include a mild brain injury, skull fractures, focal neurological deficit, or a severe head injury. These results are then defined with further diagnostic testing.
A registered health professional, such as an emergency department physician, paramedic, or nurse, typically conducts these assessments. Depending on the context of the injury, the patient's condition, and the available equipment, these professionals may only be able to complete a partial assessment until they have further assistance.