Head and Neck Assessment
Access our free comprehensive Head and Neck Assessment template and effectively support clinical evaluations and improve diagnostic accuracy.


What is a Head and Neck Assessment?
A Head and Neck Assessment is a focused physical examination performed by healthcare professionals to identify signs of disease or abnormalities in the head and neck (Ernstmeyer & Christman, 2021). This physical assessment involves systematically observing, palpating, and sometimes auscultating specific regions, including the lymph nodes, thyroid gland, facial skin, and temporal artery.
The assessment provides valuable information about potential causes of symptoms such as neck pain or swelling. Practitioners also evaluate facial features, facial expressions, and facial nerve function, particularly cranial nerve VII, to detect neurological deficits. An examination of the oral cavity may reveal issues like loose teeth or lesions.
Findings related to the posterior cervical lymph nodes, trachea, or thyroid can indicate infections or other conditions requiring further investigation. Documented assessment findings support clinical decision-making and treatment planning. This evaluation is often recorded under the head, eyes, ears, nose, and throat (HEENT) section in medical records and is essential for identifying systemic and localized health issues.
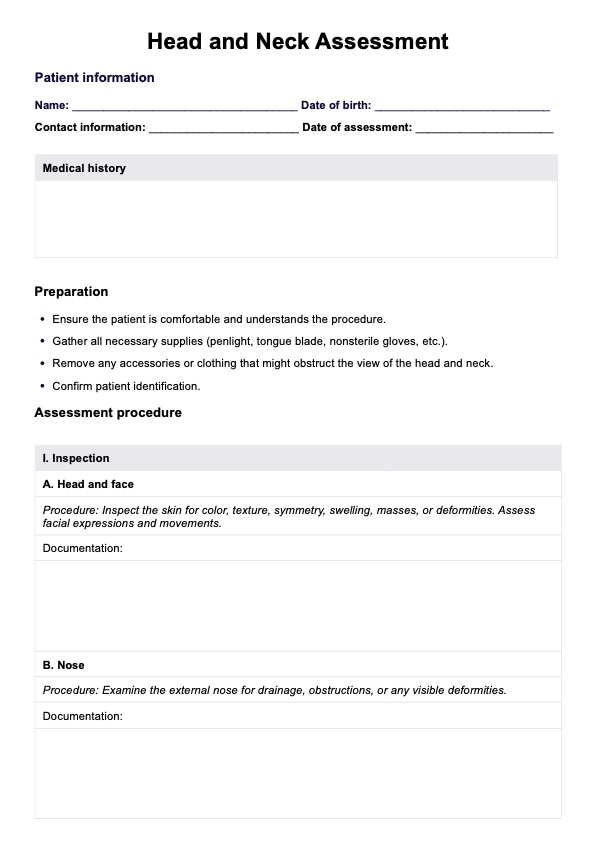
Head and Neck Assessment Template
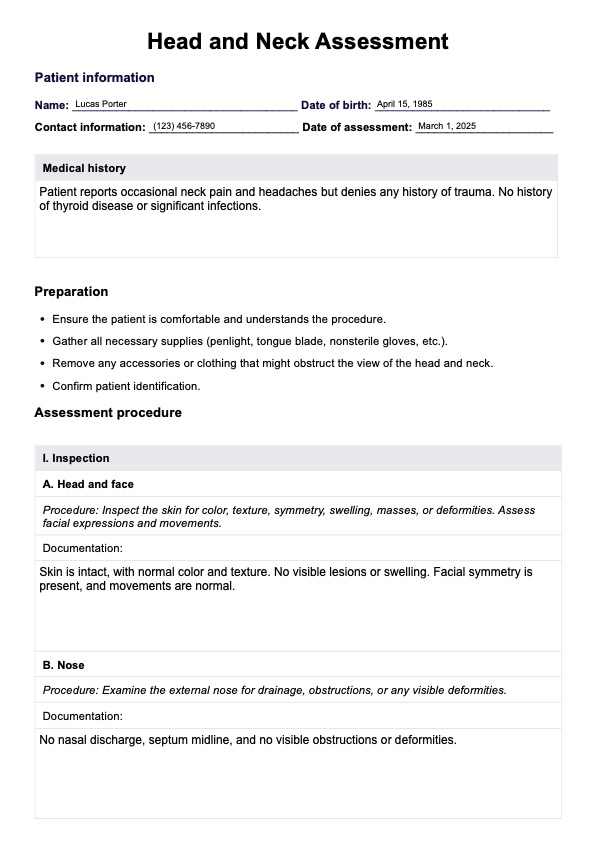
Head and Neck Assessment Example
Key components of a Head and Neck Assessment
A Head and Neck Assessment involves a structured evaluation of critical anatomical structures to identify abnormalities, assess function, and aid in diagnosis. This assessment consists of three main components: inspection, palpation, and additional assessments. Each step provides essential clinical findings that support accurate diagnosis and treatment planning.
Inspection
Inspection is the first step, requiring visual observation of the head, face, nose, oral cavity, and neck. The examiner assesses skin color, texture, symmetry, swelling, deformities, and facial expressions to detect abnormalities. The nose is checked for obstructions or drainage, while the oral cavity is examined for lesions, tongue position, uvula movement, and tonsil enlargement. Neck inspection focuses on tracheal deviation, asymmetry, masses, or visible swelling, which may indicate thyroid disorders or lymphadenopathy.
Palpation
Palpation is used to assess tissue consistency, tenderness, and abnormalities in the cranium, lymph nodes, and cervical spine. The scalp and skull are checked for masses, indentations, or skin breakdown. Lymph nodes, including submandibular, anterior cervical, posterior cervical, and preauricular nodes, are palpated for size, tenderness, and irregularities. The cervical spine and surrounding muscles are examined for pain, spasms, or asymmetry, which may indicate musculoskeletal or neurological conditions.
Additional assessments
Additional assessments offer deeper insight into neurological, speech, and motor function. A cranial nerve evaluation, particularly assessing cranial nerve VII, tests facial sensation and motor responses (Reese et al., 2023). Swallowing assessments help identify dysphagia or neuromuscular dysfunction, while speech clarity and articulation are evaluated for any deficits. To assess mobility, the cervical spine’s range of motion is tested through flexion, extension, lateral bending, and rotation. Additionally, the ears may be examined for discharge, deformities, or abnormalities that could indicate infections or structural concerns.
How does this Head and Neck Assessment documentation work?
The template makes clinical evaluations easier by offering a clear structure for documentation. It helps you examine important body structures, record findings, and make well-informed decisions. Follow these steps to access, use, and understand assessment results effectively in your practice.
Step 1: Access the assessment template
Start by clicking the "Use template" button to instantly access the Head and Neck Assessment within Carepatron’s platform. You’ll be directed to download the Carepatron app, where the template is ready for use. This digital tool simplifies documentation and ensures a structured approach to patient evaluations. If you want a fillable PDF version, just click "Download."
Step 2: Use the template in patient assessment
Once opened, the template guides you through the inspection, palpation, and additional assessments necessary for a thorough head and neck examination. It provides dedicated fields for structured note-taking, ensuring all critical components are accurately recorded for clinical reference.
Step 3: Gather and interpret findings
As you complete the Head and Neck Assessment, the template allows you to document abnormalities, compare bilateral structures, and assess potential pathology. Findings related to neck pain, lymph node swelling, or facial nerve dysfunction can be analyzed systematically, helping you formulate a diagnosis or determine the need for further medical evaluation.
Step 4: Provide patient education and next steps
Based on the assessment findings, you can outline recommended interventions, referrals, or follow-up care. The documentation helps ensure accurate reporting, allowing for clear communication with other healthcare professionals. Whether managing a routine evaluation or identifying serious conditions, the template enhances efficiency and supports evidence-based decision-making.
Benefits of using this assessment
The Head and Neck Assessment improves clinical efficiency by providing a clear, structured way to examine key anatomical structures. It ensures consistency in identifying issues like swollen lymph nodes, asymmetry, or deformities, which may signal underlying medical conditions. This assessment is commonly performed during routine check-ups or when patients report symptoms such as pain, swelling, or difficulty swallowing.
Using a standardized template makes it easier to document unexpected findings and track changes over time. It also helps identify problems with the temporomandibular joint, facial nerves, and cervical spine, allowing for early intervention and timely referrals. By systematically addressing all critical aspects, the template streamlines workflow, reduces the risk of missing important details, and improves communication with other healthcare professionals.
References
Ernstmeyer, K., & Christman, E. (2021). Chapter 7: Head and neck assessment. Chippewa Valley Technical College. https://www.ncbi.nlm.nih.gov/books/NBK593205/
Reese, V., Das, J. M., & Khalili, Y. A. (2023). Cranial nerve testing. Statpearls. https://www.ncbi.nlm.nih.gov/books/NBK585066/
Commonly asked questions
A Head and Neck Assessment includes inspection, palpation, and additional evaluations to examine the head, face, eyes, ears, nose, oral cavity, neck, lymph nodes, thyroid gland, and cranial nerves. It focuses on identifying abnormalities, structural irregularities, neurological deficits, and signs of underlying medical conditions.
Normal findings include symmetrical facial features, even skin tone, intact cranial nerve function, clear oral mucosa, midline trachea, non-palpable lymph nodes, and full range of motion in the cervical spine. The temporomandibular joint moves smoothly without pain, the thyroid is non-enlarged, and there are no visible or palpable abnormalities.
Observations include facial symmetry, skin integrity, swelling, abnormal movements, cranial nerve function, lymph node enlargement, and tracheal position. Clinicians also evaluate speech clarity, swallowing ability, and musculoskeletal alignment to detect any neurological or structural abnormalities.