Yes, the physical therapists caring for the patient should be able to make sure that the patient doesn’t fall while doing the trials. They should also be able to gauge if doing the test is something the patient can do.
Functional Reach Test
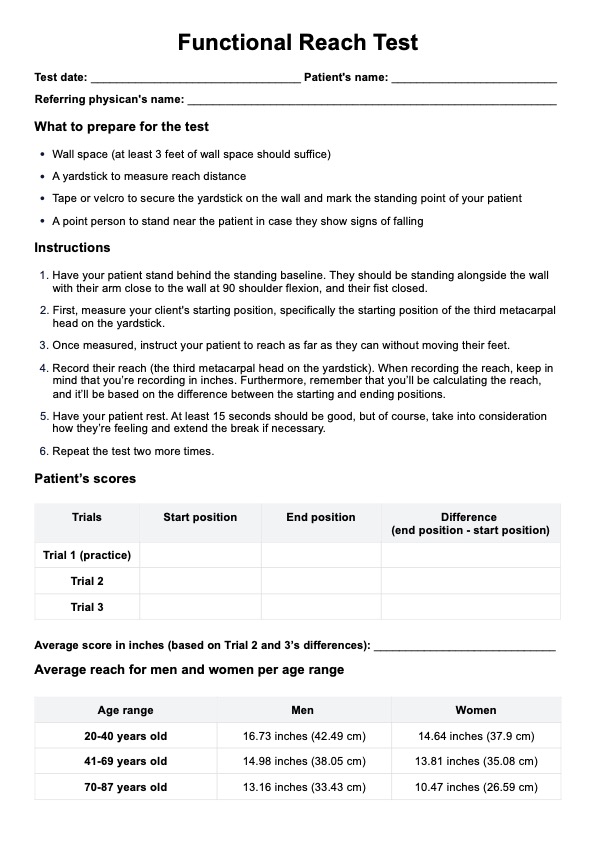
Use the Functional Reach Test to assess dynamic balance —especially in the elderly—to determine their risk of falling.
Functional Reach Test Template
Commonly asked questions
Yes. The Functional Reach Test has a modified version that caters to sitting patients. You can still fall even while sitting down, so if the patient can’t stand, they can opt for the modified test.
Yes. The Functional Reach Test is not only easy to do, but it’s reliable and valid because you’re working with numbers. You’re looking at how far they can extend their reach and calculate the average based on the three trials. There are assigned designations for reach ranges to assess the risk of falling.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











