The diagnosis of liver cirrhosis is typically confirmed through a combination of liver function tests (LFTs), imaging studies such as ultrasound or CT scans, and a liver biopsy. These methods help assess the extent of liver damage, fibrosis, and the presence of complications like portal hypertension.
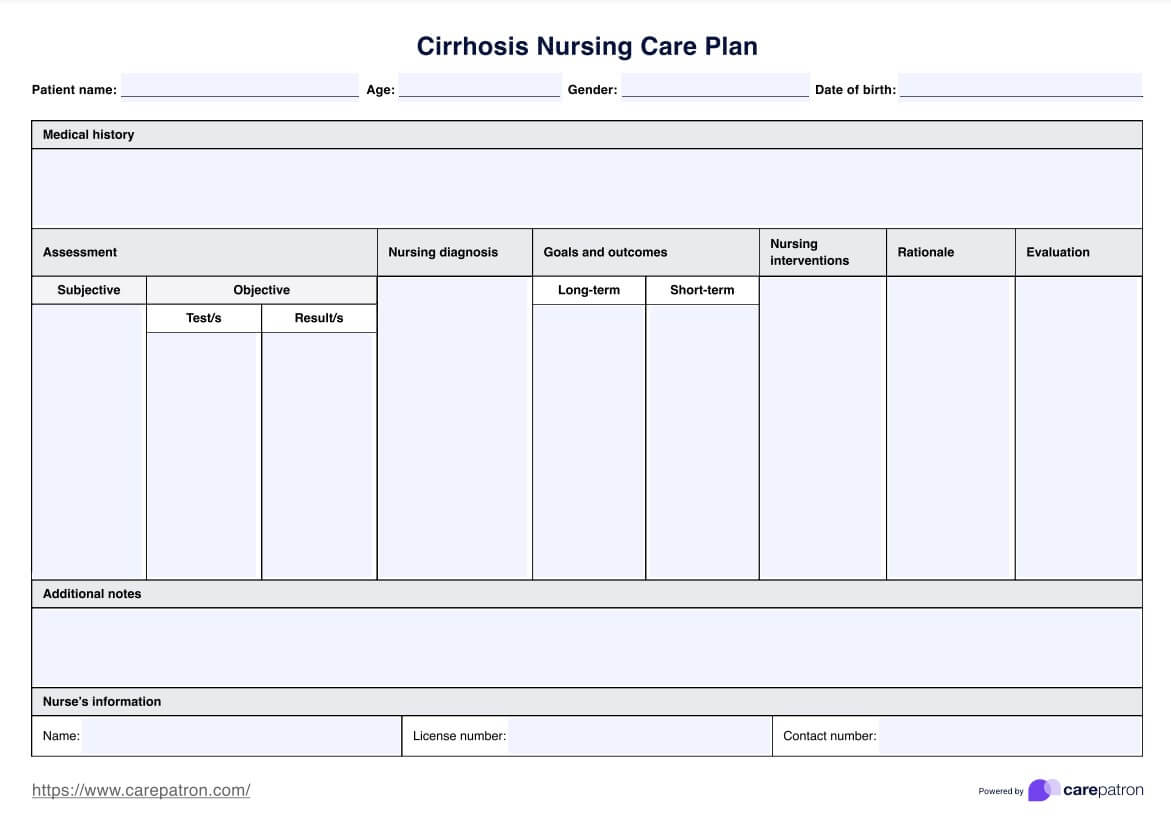
Cirrhosis Nursing Care Plan
Take care of your patients confidently and use Carepatron's free comprehensive nursing diagnosis for cirrhosis PDF for expert guidance and support.
Use Template
Cirrhosis Nursing Care Plan Template
Commonly asked questions
Nursing care for cirrhosis should prioritize rest, nutrition, skin care, injury prevention, and managing complications.
An essential nursing function when caring for a patient with cirrhosis is to assess and monitor the patient's liver function, fluid balance, and mental status regularly, as these are critical indicators of disease progression and complications.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











