Blood Test for Depression
Learn about blood tests for depression and download Carepatron's free example in PDF format to understand the process better.


What is depression?
Depression, a prevalent mental health condition, extends beyond occasional feelings of sadness or low energy. It is a complex disorder that significantly impacts one's thoughts, emotions, and daily functioning. Major Depressive Disorder (MDD) is a common form of depression, characterized by persistent feelings of hopelessness and a lack of interest in activities. Individuals experiencing significant depression often face challenges in maintaining relationships, work, and overall life satisfaction.
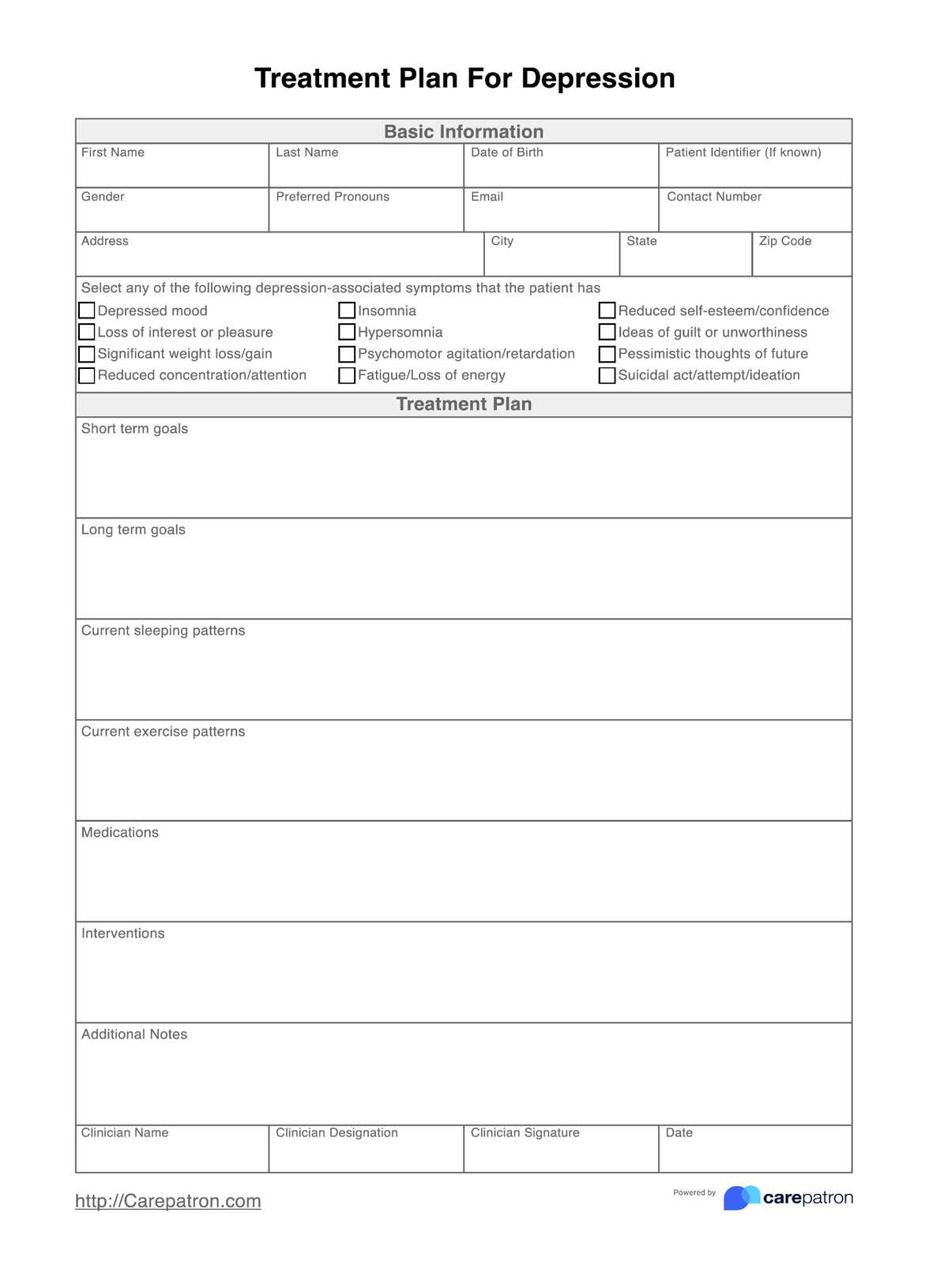
Understanding depression is crucial in fostering a proactive approach towards mental well-being. Mental health providers play a pivotal role in diagnosing and treating depression. They provide treatment plans for depression after identifying presenting symptoms and outlining intervention methods.
Depression falls under the broader category of mood disorders and mental health problems, affecting millions of people globally. It is not merely a temporary state of mind but a severe mental illness that requires attention and care. Addressing depression through depression screening involves a multifaceted approach, combining psychological interventions, lifestyle changes, and sometimes medication.
In mental health terms, diagnosing depression is a nuanced process. Mental health professionals employ various methods, including comprehensive assessments and interviews, to understand the individual's emotional state. Lab tests are not typically used for diagnosing depression, but they may be employed to rule out other underlying health issues.
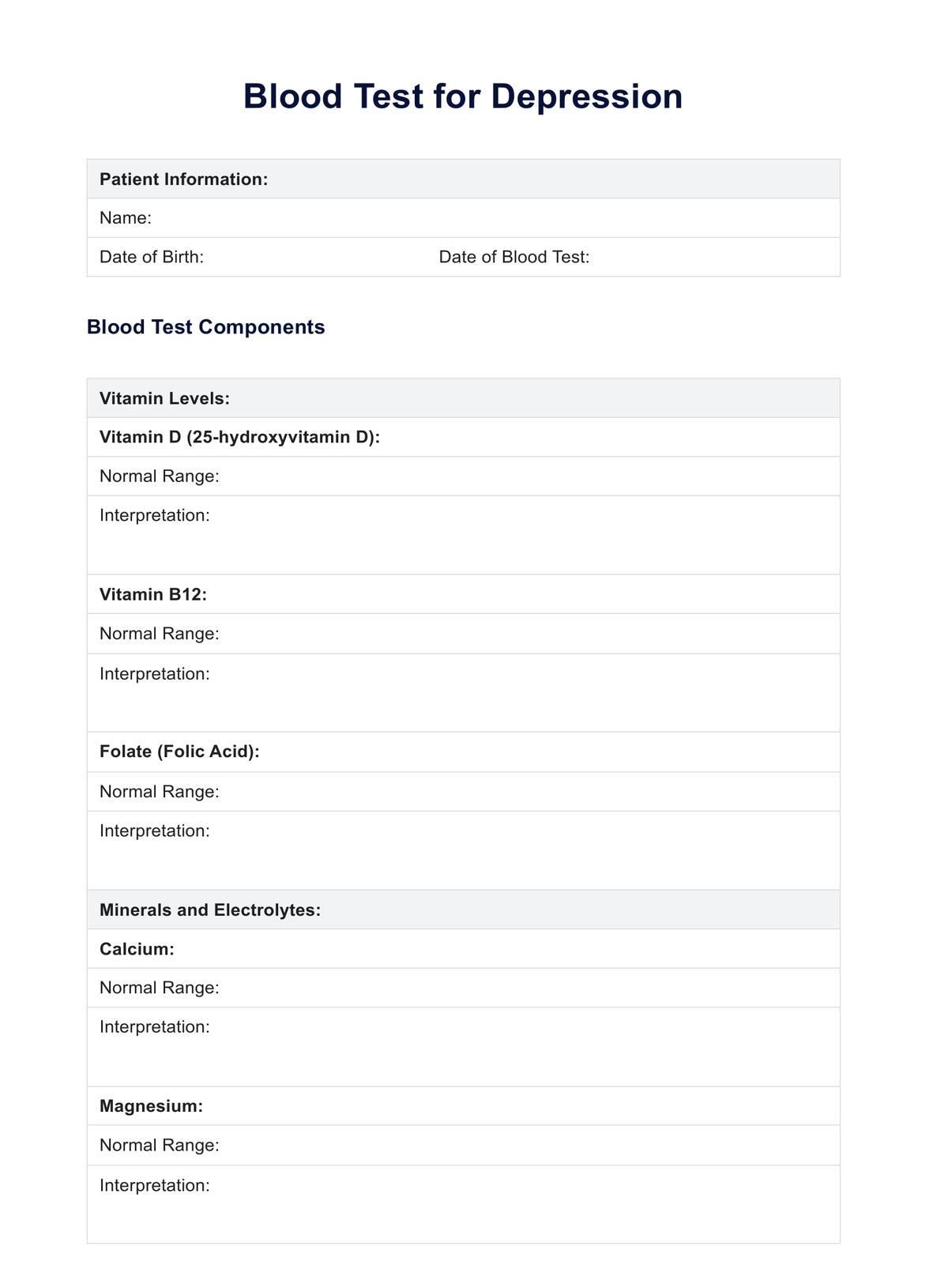
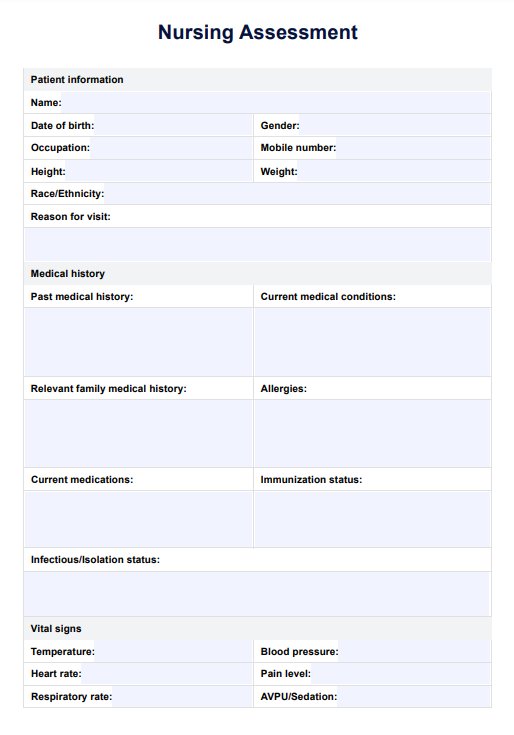
Blood Test for Depression Template
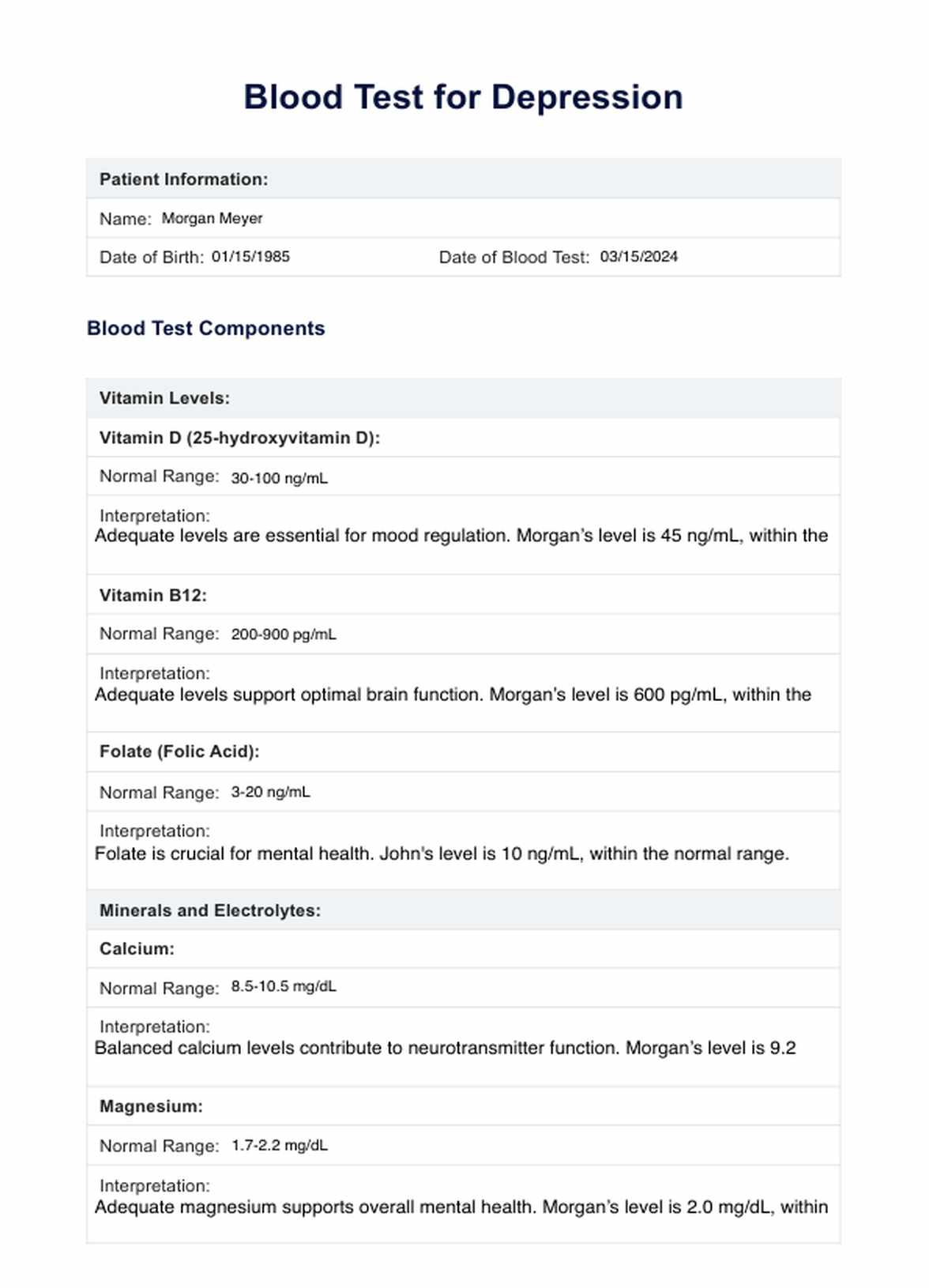
Blood Test for Depression Example
Symptoms of depression
Depression manifests through a range of emotional, cognitive, and physical symptoms that collectively contribute to the overall impact on an individual's well-being. Recognizing these symptoms is crucial for early intervention to treat depression and seeking support from a mental health provider.
Here, we'll explore key symptoms associated with properly diagnosing depression:
Persistent sadness and hopelessness
Individuals with major depression often experience a prolonged sense of sadness and hopelessness that persists for most of the day, nearly every day.
Loss of interest or pleasure
A hallmark symptom is the diminished interest or pleasure in once enjoyable activities. Hobbies and social engagements may lose their appeal.
Changes in sleep patterns
Depression can disrupt sleep, leading to insomnia or, conversely, excessive sleeping. Changes in sleep patterns often contribute to fatigue and decreased energy levels.
Appetite and weight changes
Significant changes in appetite, resulting in weight loss or gain, are common in major depression. These alterations are unrelated to intentional dietary modifications.
Fatigue and decreased energy
Individuals with depression frequently report persistent fatigue, even after adequate rest, making daily tasks challenging to manage.
Difficulty concentrating
Cognitive symptoms include difficulty concentrating, making decisions, and a noticeable decline in overall cognitive function.
Feelings of worthlessness or guilt
Individuals with depression may harbor irrational feelings of worthlessness or excessive guilt, irrespective of their actual circumstances.
Physical aches and pains
Depression can manifest as physical symptoms, such as headaches, stomachaches, or general bodily discomfort, without apparent medical cause.
Agitation or restlessness
Some individuals experience increased irritability, restlessness, or feelings of being on edge, often associated with the internal turmoil of depression.
Suicidal thoughts
In severe cases, depression may lead to thoughts of death or suicide. It is crucial to seek immediate help if these thoughts arise.
While these symptoms provide a general overview, it's important to note that individuals may experience depression differently. Diagnosing depression involves a comprehensive assessment by a mental health professional, often excluding other conditions like bipolar disorder.
Blood tests, although not a primary tool for diagnosis, may contribute to a holistic understanding of an individual's mental health.
How to diagnose depression
Diagnosing depression is a nuanced process that requires the expertise of mental health professionals. Let's explore the key steps involved in diagnosing depression:
Initial assessment by a mental health professional
The diagnostic journey often begins with a comprehensive assessment by a mental health professional, such as a psychologist, psychiatrist, or clinical social worker. This involves discussing the individual's symptoms, personal history, and any contributing factors.
Rule out other medical conditions
It's crucial to rule out medical conditions that may mimic or contribute to symptoms of depression. A thorough physical examination and, in some cases, blood tests can help identify or exclude any underlying health issues.
Diagnostic criteria for major depressive disorder (MDD)
Mental health professionals refer to established diagnostic criteria, such as those outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), to determine if an individual meets the criteria for Major Depressive Disorder (MDD).
Assessment of mood disorders
Depression often coexists with other mood disorders, such as bipolar disorder. Mental health professionals carefully assess the individual's mood patterns to differentiate between various mental health conditions.
Evaluation of mental health history
Understanding the individual's mental health history is essential for accurate diagnosis. This includes exploring past episodes of depression, response to previous treatments, and any family history of mental health conditions.
Ongoing monitoring and refinement of diagnosis
Diagnosing depression is an evolving process. Mental health professionals may continually monitor the individual's symptoms and response to treatment and adjust the diagnosis or treatment plan as needed.
Common blood tests for depression
Understanding the physiological aspects of depression involves exploring various blood tests that can provide valuable insights into an individual's mental health. While lab tests are not standalone diagnostic tools for depression, they contribute to a more comprehensive assessment.
Let's delve into some standard blood tests and their relevance in the context of depression:
Folate and Vitamin B12 Levels
Low levels of folate (B9) and vitamin B12 are associated with an increased risk of depression. These essential vitamins play a crucial role in brain function and the synthesis of neurotransmitters. A deficiency in folate or vitamin B12 may contribute to depressive symptoms. Lab tests measuring these levels can guide mental health providers in recommending appropriate supplementation to support overall mental well-being.
Vitamin D - 25(OH)D
Vitamin D, often called the "sunshine vitamin," is linked to mood regulation. Research suggests a correlation between low vitamin D levels and an elevated risk of depression. The 25-hydroxyvitamin D blood test assesses the body's vitamin D status. Adequate vitamin D levels are essential for mental health, and addressing deficiencies may be a part of the comprehensive approach to treating depression.
Calcium and Magnesium Levels
Calcium and magnesium are minerals that affect neurotransmitter regulation and overall brain function. Imbalances in these minerals may contribute to mood disorders, including depression. Blood tests measuring calcium and magnesium levels can help identify potential deficiencies or excesses, allowing mental health providers to recommend appropriate dietary adjustments or supplements.
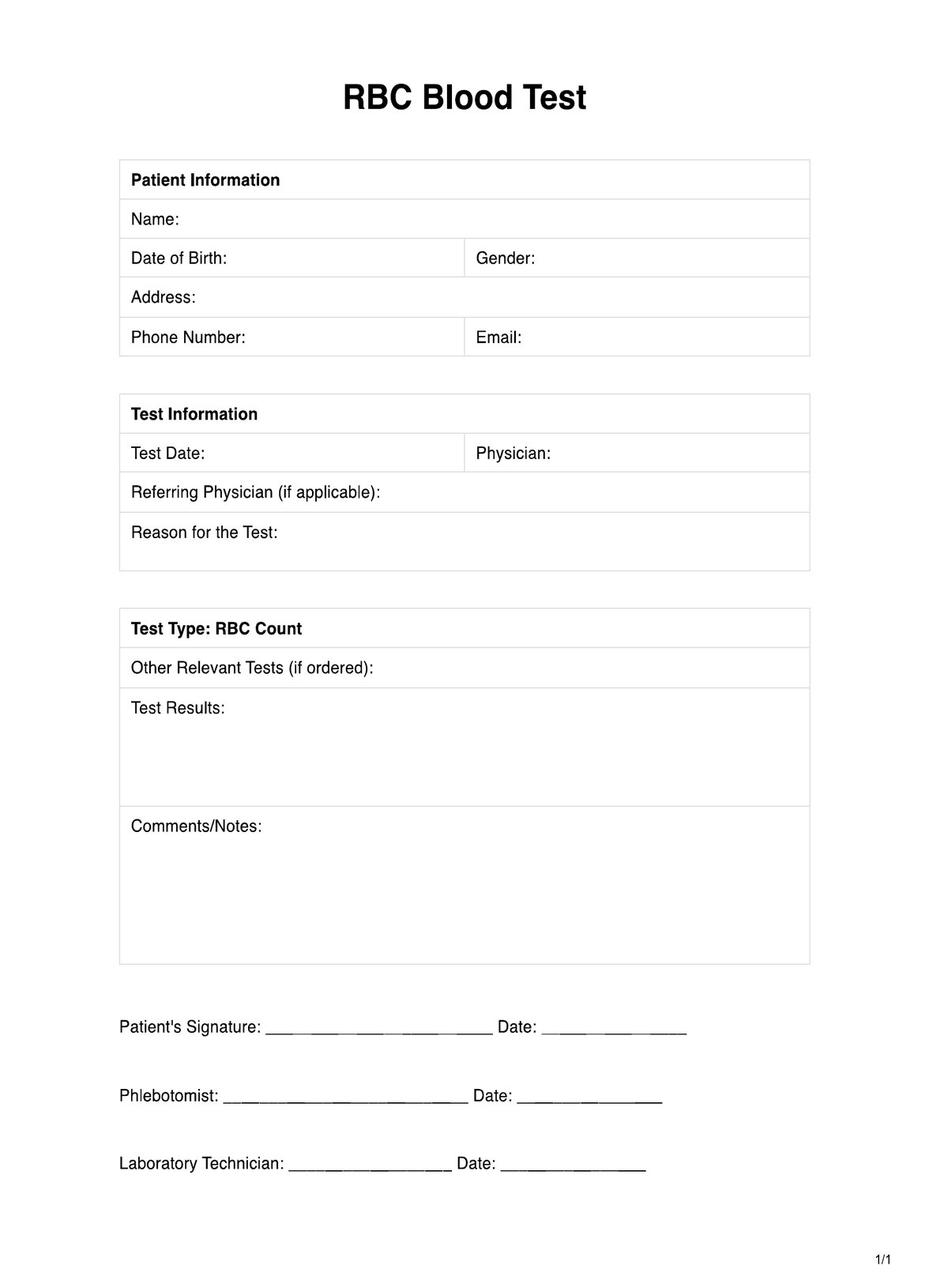
Creatinine and Blood Urea Nitrogen (BUN)
The kidneys play a vital role in filtering waste products from the blood. Creatinine and Blood Urea Nitrogen (BUN) are markers used to assess kidney function. Kidney dysfunction can lead to the accumulation of toxins in the body, impacting mental health. Checking creatinine and BUN levels ensures that the physiological factors contributing to depression symptoms are thoroughly examined.
Why conduct a Blood Test for Depression?
Understanding the role of blood tests in the context of severe depression is crucial for a comprehensive mental health assessment. While not a standalone diagnostic tool, these tests can provide valuable insights when used with clinical evaluations for any seasonal affective disorder.
Let's explore the reasons why conducting a blood test for depression is essential:
Comprehensive assessment for correct diagnosis
When combined with other diagnostic methods, a blood test contributes to a more thorough evaluation. This comprehensive approach aids health care professionals in achieving an accurate diagnosis, ensuring individuals receive appropriate and targeted treatment.
Identifying vitamin D deficiency
Low levels of vitamin D have been linked to an increased risk of depression. Blood tests can reveal deficiency in vitamin D, allowing for targeted interventions and supplementation as part of the treatment plan.
Supporting clinical depression evaluation
Blood tests serve as additional tools in the assessment of clinical depression. The National Institute of Mental Health recommends a multifaceted approach to diagnosing depression, incorporating clinical evaluations and, when necessary, laboratory tests.
Informing treatment planning
Results from blood tests provide valuable information for health care professionals to tailor treatment plans effectively. This personalized approach ensures that interventions address specific factors contributing to an individual's depression, promoting more successful outcomes.
Aligning with clinical practice guidelines
Clinical practice guidelines, such as the Hamilton Depression Rating Scale, emphasize the importance of a thorough assessment in depression diagnosis. Blood tests contribute to meeting these guidelines by providing additional data for a holistic understanding of an individual's mental health.
What blood test results mean
After undergoing a blood test for depression, understanding the interpretation of results is essential. Here are potential interpretations of results for depression:
Optimal vitamin levels
Adequate levels of essential vitamins, such as vitamin D, B12, and folate, suggest a healthy nutritional status. This can positively contribute to overall well-being and may indicate that dietary factors are not significantly contributing to depressive symptoms.
Vitamin D deficiency
Low levels of vitamin D may be indicative of a deficiency, potentially linked to an increased risk of depression. Addressing this deficiency through supplementation, lifestyle changes, or increased exposure to sunlight can be a crucial aspect of the treatment plan.
Normal calcium and magnesium levels
Calcium and magnesium levels support neurotransmitter function and overall mental health within the normal range. Imbalances in these minerals could be addressed through dietary changes or supplements if needed.
Healthy kidney function
Normal creatinine and Blood Urea Nitrogen (BUN) levels suggest healthy kidney function. This is particularly important as some medications used to treat depression can impact renal health.
Integrated approach to treatment
When considered alongside clinical evaluations, results contribute to a more holistic understanding of an individual's mental health. This integrated approach allows health care professionals to develop personalized treatment plans addressing both physiological and psychological aspects of depression.
Commonly asked questions
While there is no specific blood test for diagnosing depression, certain blood tests can provide valuable information. Assessing vitamin levels, thyroid function, and ruling out other medical conditions through blood tests can contribute to a comprehensive mental health assessment.
The gold standard for diagnosing depression is a thorough clinical assessment by a mental health professional. Tools like the Hamilton Depression Rating Scale are commonly used, complemented by discussions about symptoms, medical history, and potential contributing factors.
Conditions often associated with depression include anxiety disorders, chronic pain conditions, and other mood disorders like bipolar disorder. Addressing these coexisting conditions is crucial for comprehensive depression management.