Nursing Assessment
Comprehensive nursing assessments: gather patient data, assess vital signs, perform physical examinations, and develop individualized care plans.


What is a Nursing Assessment?
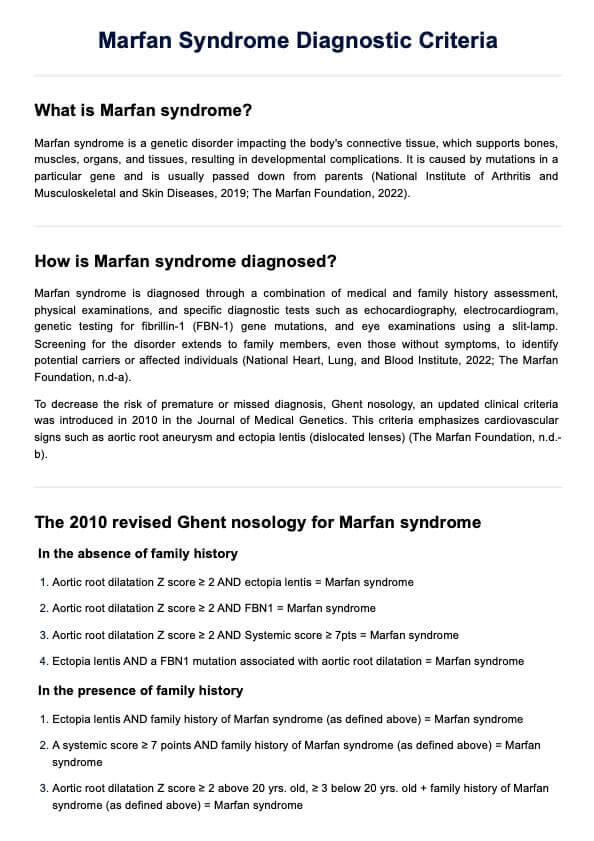
A Nursing Assessment involves collecting comprehensive information about a patient's physical, psychological, and social health to develop a personalized care plan. This assessment is crucial for ensuring patient safety and guiding the healthcare team.
During a head-to-toe assessment, nurses gather both subjective and objective data. Subjective data refers to what the patient shares, such as symptoms or pain levels. Objective data comes from measurable findings during a physical assessment, such as vital signs, including blood pressure, pulse, and respiratory assessment. Nurses may also listen for bowel sounds and assess the patient's overall condition.
Nursing Assessments happen during various stages, such as admission assessments, routine check-ups, or when there's a change in the patient's status. These assessments may be comprehensive or focused assessments targeting specific areas of concern. During this nursing process, nurses use the gathered data to make informed clinical judgments and create a nursing diagnosis.
By conducting thorough assessments, nurses help identify health issues early, prevent complications, and ensure the patient receives the best possible care. These assessments also improve communication between nurses and other health professionals, contributing to effective collaboration within the health care team.
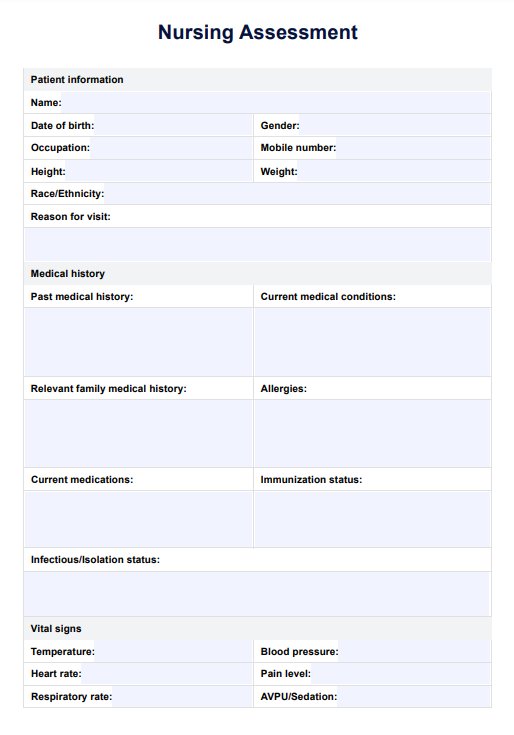
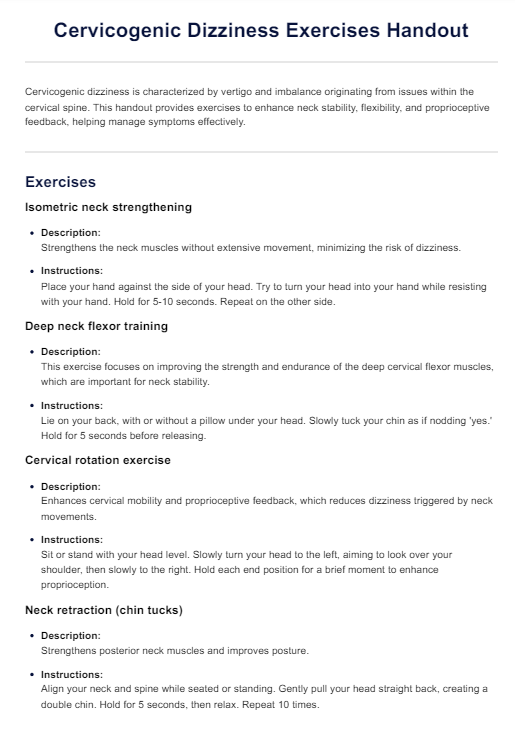
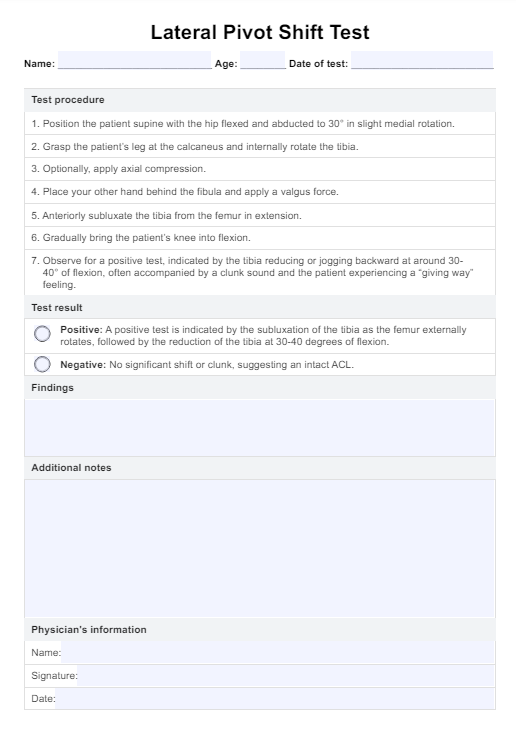
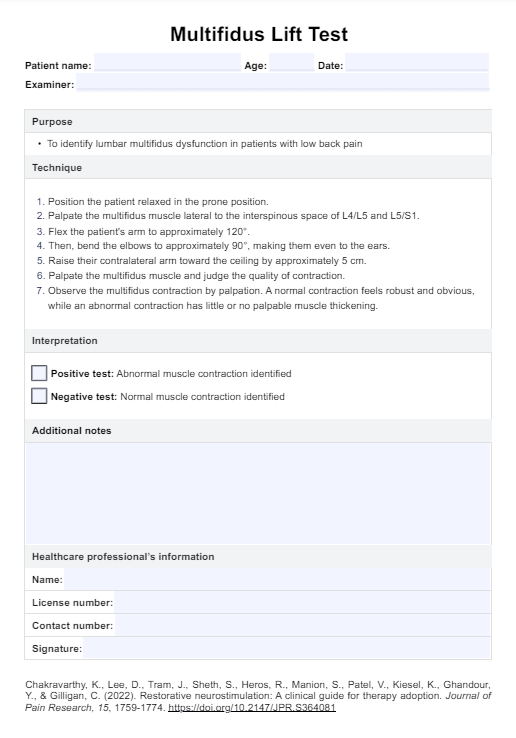
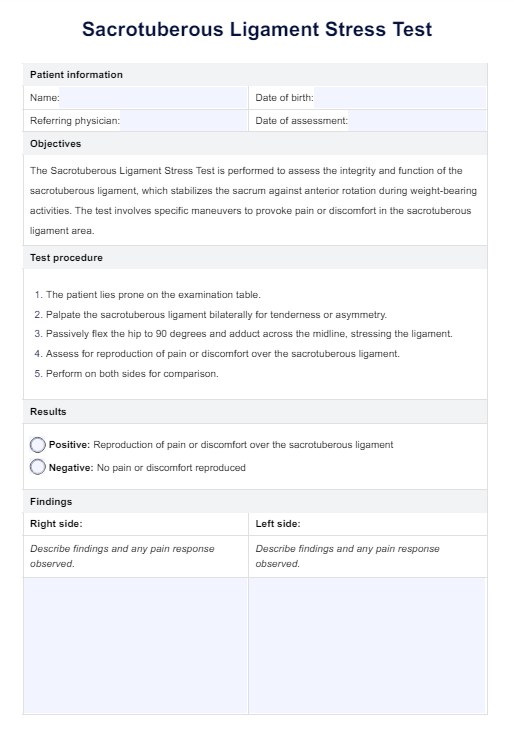
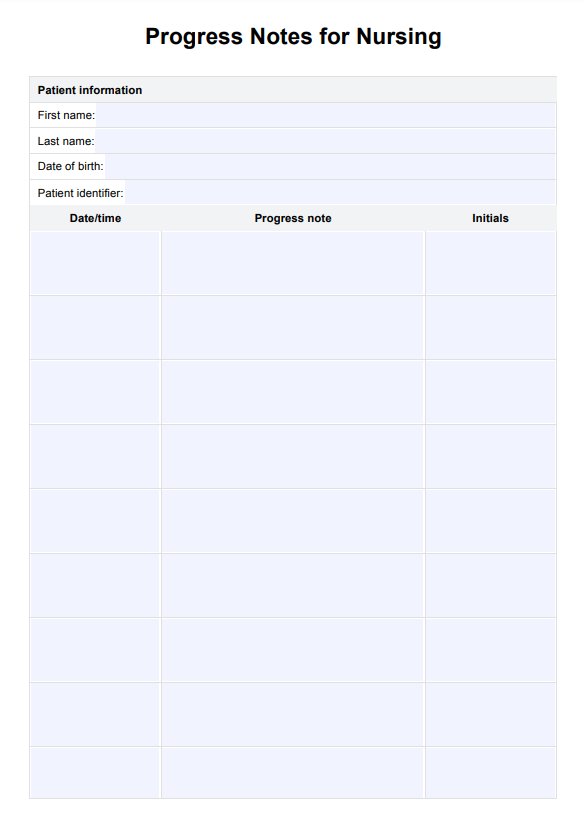
Nursing Assessment Template
Nursing Assessment Example
How does it work?
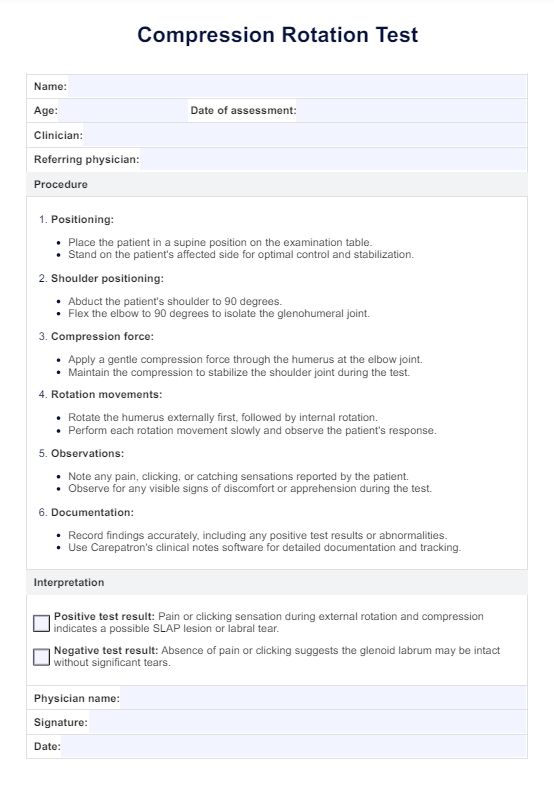
Here are some steps involved in using our Nursing Assessment template effectively:
Download the template
Start by downloading the Nursing Assessment template by clicking "Use Template". Choose "Download" for a PDF copy.
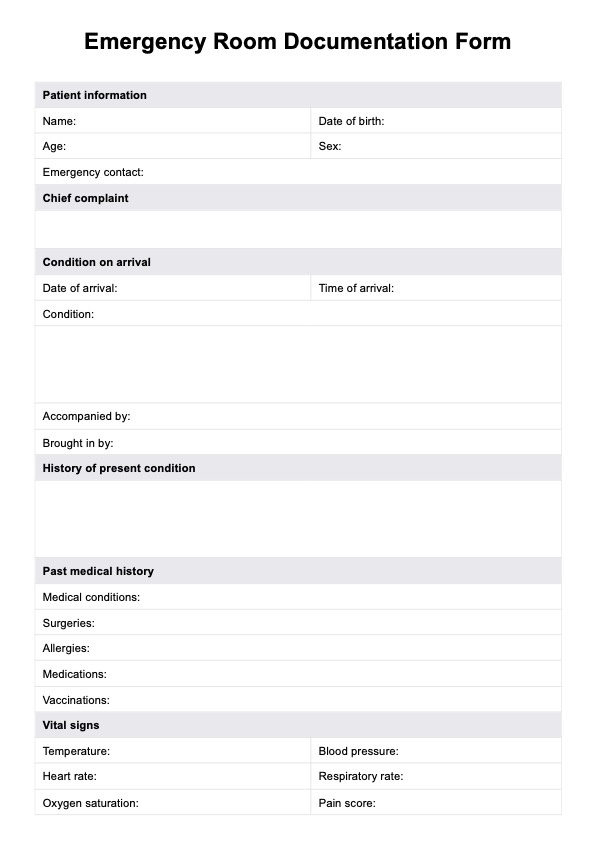
Patient identification
Record essential patient information, including the patient's full name, age, gender, and contact details. This step is crucial for accurately identifying the patient and ensuring that all assessments and care plans are correctly attributed.
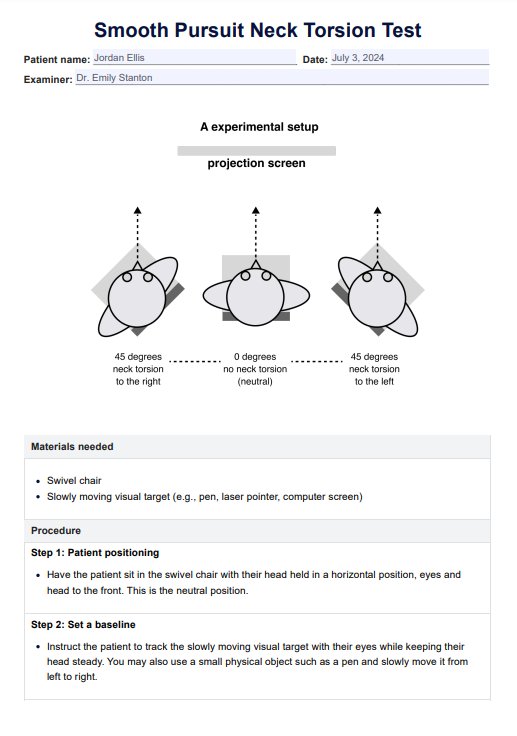
Subjective and objective assessments
Gather subjective data by conducting interviews with the patient. Ask about their current symptoms, medical history, allergies, and medications. Also, explore psychosocial aspects, such as their perception of health and pain levels. Following this, perform a thorough objective assessment that includes measuring vital signs and conducting a physical examination.
Review diagnostic tests
Collect and document results from any relevant diagnostic tests and laboratory investigations. This may include blood tests, imaging studies, and other assessments that provide valuable insights into the patient’s health status. Reviewing this data helps identify underlying health issues that may need to be addressed in the care plan.
When would you use this template?
The Nursing Assessment template is valuable for various scenarios in nursing practice, providing a structured approach to patient evaluations. Here are some situations where this template would be particularly beneficial:
Initial patient assessment
Upon admitting a patient to a healthcare facility, registered nurses can utilize the template to perform a complete health assessment. This comprehensive evaluation includes gathering crucial information about the patient's health status, medical history, and current needs. By employing a head-to-toe approach, nurses can ensure that all body systems are examined, enhancing their clinical judgment and supporting accurate nursing diagnoses.
Routine check-ups
The template serves as a guide for conducting thorough physical assessments during regular check-ups or follow-up visits. It helps monitor changes in the patient's condition, detect early signs of deterioration, and maintain continuity of care. This structured method reinforces the assessment process, allowing nurses to collect vital assessment data consistently.
Shift handovers
The template is useful for documenting and communicating essential patient information during shift handovers. By organizing relevant assessment data, nurses can ensure a seamless transition of care between shifts. This practice is crucial for maintaining patient safety and ensuring that critical details are not overlooked.
Change in patient condition
If a patient experiences a change in condition, such as new symptoms or a decline in vital signs, the template aids in conducting a focused assessment. This allows nurses to gather pertinent information quickly, facilitating prompt intervention and appropriate escalation of care. This tool enhances the nurse's clinical judgment, ensuring that nursing diagnoses are accurately determined based on the latest assessment findings.
Home healthcare
Nurses delivering home healthcare services can effectively use the template to assess patients in their home environment. This approach enables monitoring health status, identifying emerging issues, and planning appropriate interventions tailored to the patient's needs. Utilizing this structured format in home settings aligns with nursing education principles, enhancing the overall quality of care.
Collaborative care
The Nursing Assessment template is a standardized tool for collecting and organizing patient data, promoting effective communication and collaboration among healthcare providers. This ensures that all healthcare team members can make informed decisions and deliver coordinated care based on a shared understanding of the patient’s health history and current condition.
Benefits of using our Nursing Assessment template
Utilizing the Nursing Assessment template offers numerous advantages for healthcare professionals, including registered nurses and advanced practice nurses. Here are some key benefits:
Streamlined and comprehensive assessment
The template provides a structured framework for conducting Nursing Assessments, addressing all essential areas. It guides registered nurses and other healthcare providers in gathering comprehensive subjective and objective data. This holistic approach leads to a better understanding of the patient's health history and current status, which is critical for effective nursing care.
Time-saving and efficiency
The template saves time by offering predefined sections and fields and eliminates the need to create a new assessment form from scratch. Healthcare professionals can focus on gathering and documenting data efficiently, reducing duplication of effort and improving workflow.
Improved communication and collaboration
The template facilitates effective communication among healthcare team members by providing a common language and structure for documenting assessment findings. It enables seamless information sharing during shift handovers, interdisciplinary meetings, and consultations, improving collaboration and continuity of care.
Enhanced patient safety and outcomes
By utilizing the template, healthcare professionals can more effectively identify potential health risks and deviations from normal functioning. Thorough assessments contribute to the early detection of complications, timely intervention, and improved patient safety and outcomes.
Documentation and legal compliance
The template ensures proper and organized documentation of assessment findings, nursing diagnoses, and care plans. It helps healthcare professionals meet legal and regulatory requirements for accurate and complete patient records, which is vital in maintaining high standards of nursing practice.
Commonly asked questions
The frequency of Nursing Assessment varies based on the patient's condition, healthcare setting, and facility protocols. Generally, assessments are conducted upon admission, during shifts, with changes in patient status, and before significant interventions or procedures.
Yes, Nursing Assessments are performed in a variety of healthcare settings, including hospitals, clinics, long-term care facilities, home healthcare, and community health centers.
Documentation in Nursing Assessments is vital for accurate record-keeping, communication among healthcare providers, legal documentation, and maintaining a comprehensive and up-to-date patient health record. Proper documentation also aids in objective data collection.