A progress note for a mental health patient is a detailed record of the patient's status, treatment, and progress during a therapy session or clinical encounter. It documents the patient's current mental state, any significant events or behaviors since the last session, the therapist's observations and clinical impressions, the interventions used, and the patient's response.
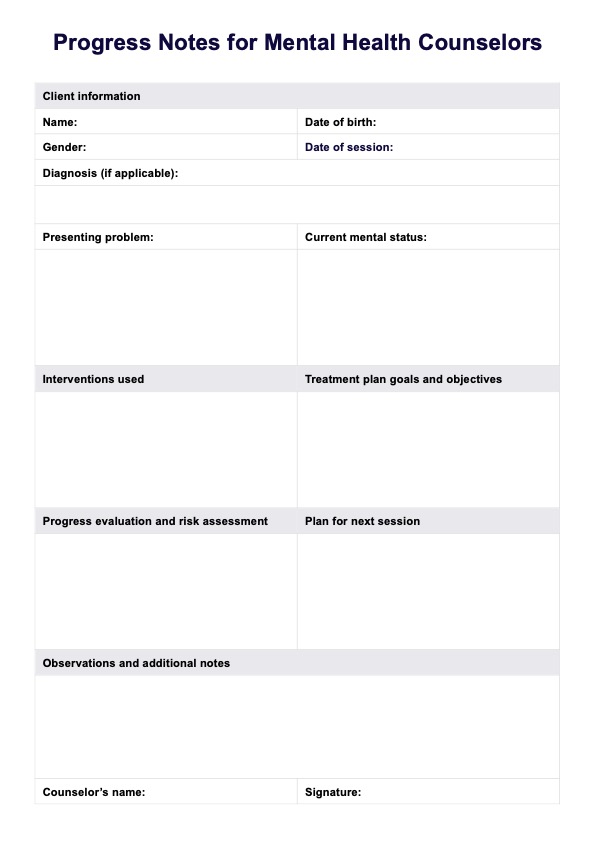
Progress Notes For Mental Health Counselors Template
Access our free template for Progress Notes for Mental Health Counselors and improve the accuracy and organization of your clinical documents.
Progress Notes For Mental Health Counselors Template Template
Commonly asked questions
Mental health notes should be clear, concise, and objective, focusing on observable facts rather than subjective interpretations. Notes should avoid jargon, use person-first language, and maintain patient confidentiality. Timely documentation, typically within 24 hours of the session, is important for accurate record-keeping.
The most common format for documenting relevant information in progress notes is the SOAP note format, which stands for Subjective, Objective, Assessment, and Plan.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











