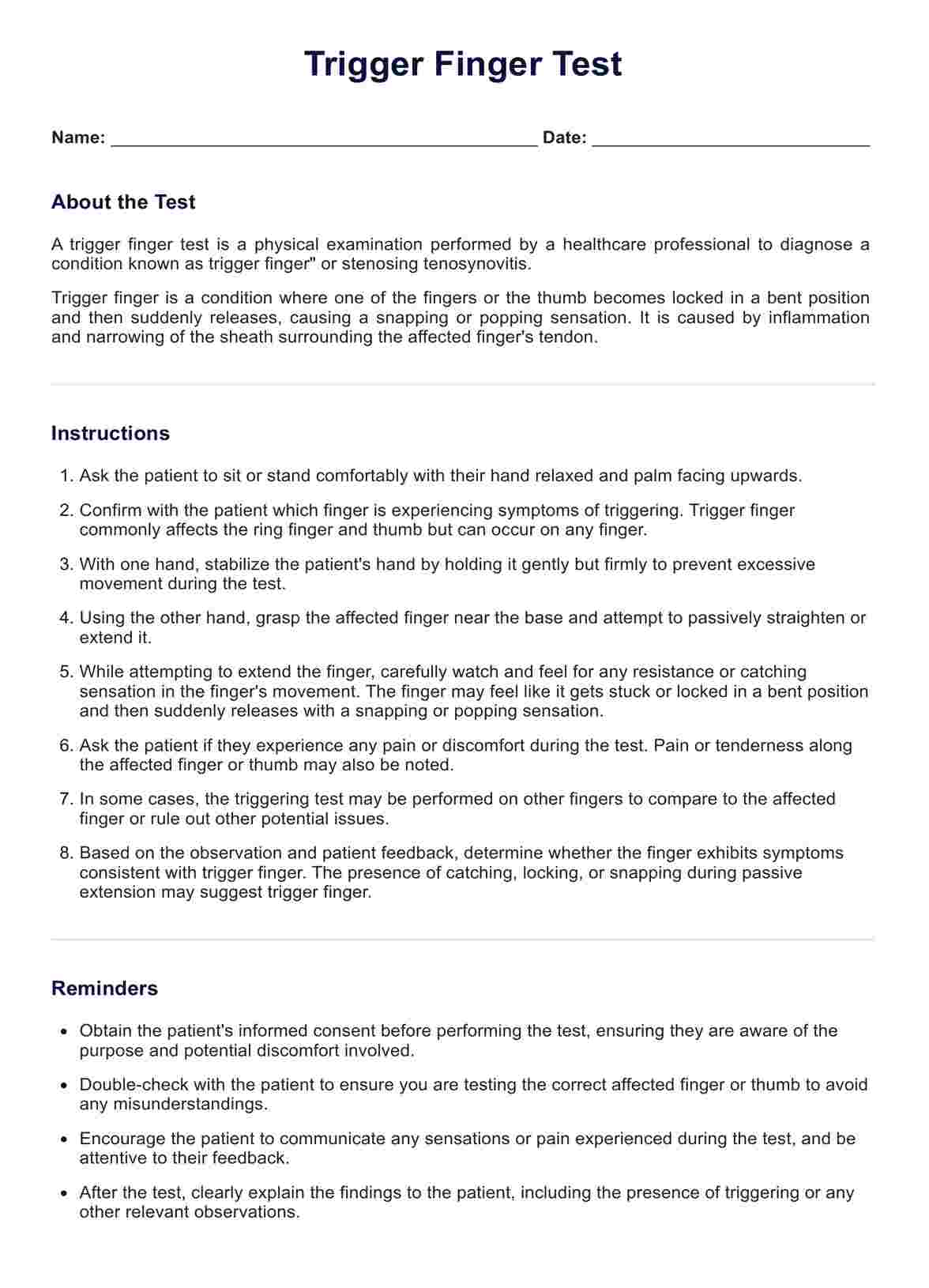
The trigger finger test is a diagnostic procedure used by healthcare professionals, typically orthopaedic surgeons or hand therapists, to identify trigger finger or trigger thumb. During this test, the patient is asked to flex and extend the affected finger or thumb. The doctor looks for symptoms like pain, finger locking in a bent position, difficulty in straightening the finger, and a clicking or snapping sound. This test helps in observing the movement of the flexor tendons through the tendon sheaths and identifying any hindrance due to swollen tendons or narrowed sheaths.
Trigger Finger Tests
Learn about the Trigger Finger Test, a quick assessment for identifying trigger finger. Download our free PDF template to conduct the exam easily.
Trigger Finger Tests Template
Commonly asked questions
Common symptoms of trigger finger include stiffness, especially in the morning, a clicking or popping sensation when moving the finger, pain at the base of the finger or thumb, and the finger locking in a bent position before snapping straight. These symptoms can affect any digit, including the ring finger or thumb, with the thumb condition often referred to as 'trigger thumb'. The intensity of symptoms might vary based on the affected digit and severity of the condition.
Risk factors for developing trigger finger include repetitive gripping activities, certain medical conditions like diabetes and rheumatoid arthritis, and occupations or hobbies that strain the fingers (e.g., playing racket sports).
Age is also a factor, with most patients being between 40 and 60 years old. Trigger finger can affect multiple digits, and it's more common in the ring finger and thumb. In some cases, more than one finger is affected, known as trigger fingers.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











