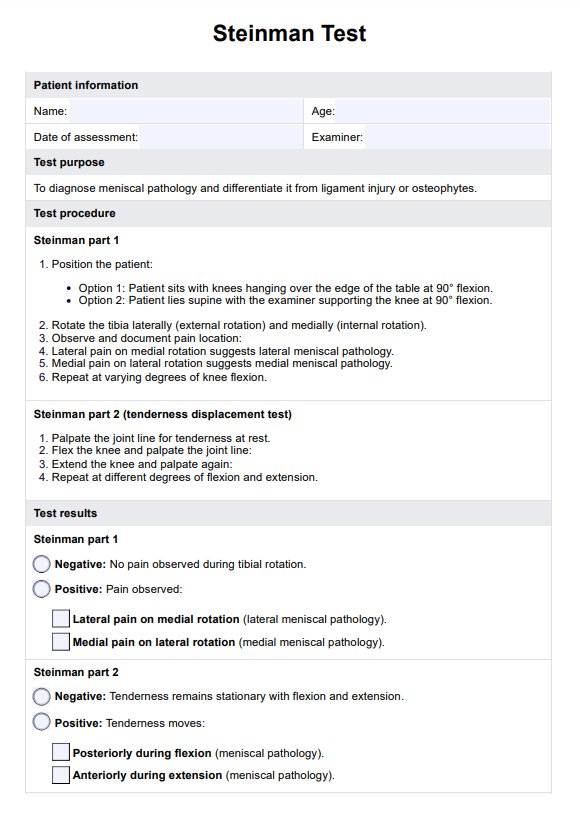
The Steinman Test is a knee orthopaedic test used to diagnose meniscal pathology by assessing pain during specific rotational movements of the tibia. Based on the location of pain, it helps identify medial or lateral meniscus injuries.
Steinman Test
Learn all about the Steinman Test and its use in diagnosing meniscal injuries. Use our template to conduct the test accurately and effectively.
Steinman Test Template
Commonly asked questions
While the Steinman Test is highly effective, the combination of clinical tests such as the McMurray Test and advanced imaging like MRI provides the most accurate diagnosis for a torn meniscus. These methods complement each other to confirm meniscal injuries.
A positive Steinman Test occurs when lateral pain is felt during medial rotation or medial pain during lateral rotation, indicating meniscus injury. Shifting joint line tenderness during knee flexion also signifies a positive result for meniscal pathology.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











