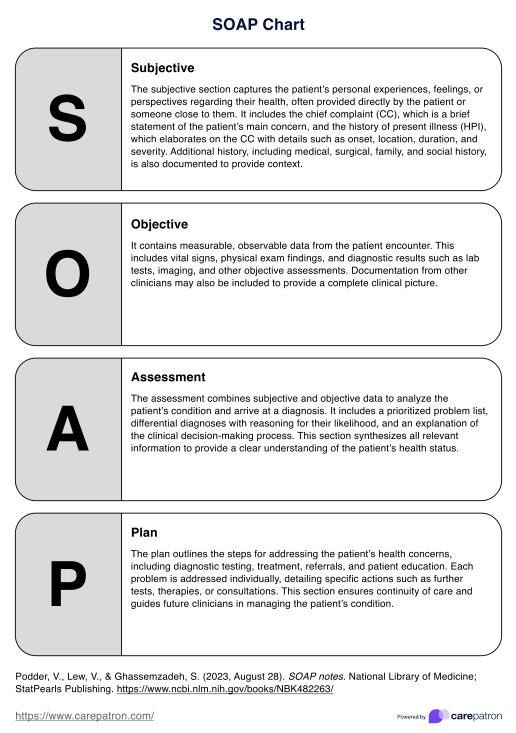
Soap Chart
Write SOAP notes with ease! Access this quick-reference SOAP Chart to know what to include and streamline your patient documentation efficiently.


What is a SOAP Chart?
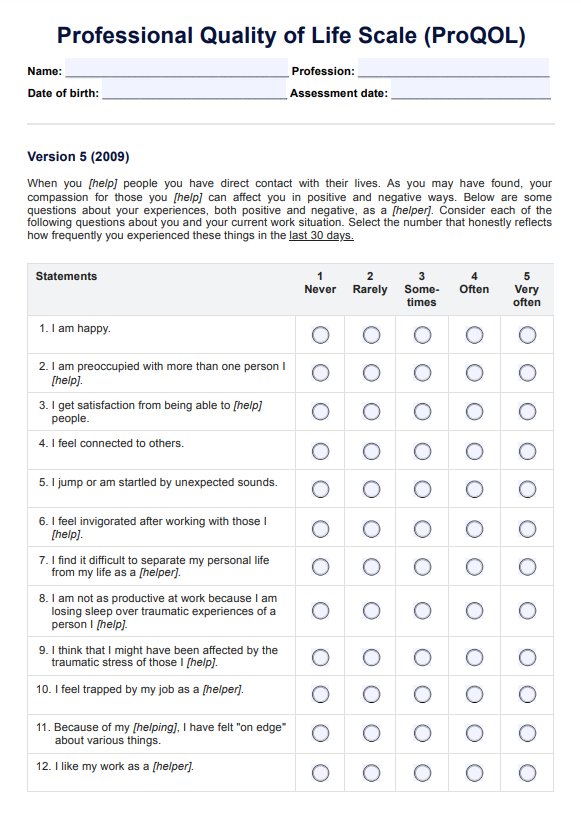
A SOAP Chart is a helpful reference tool for healthcare professionals when writing patient notes. The SOAP note format is organized into four sections: Subjective, Objective, Assessment, and Plan.
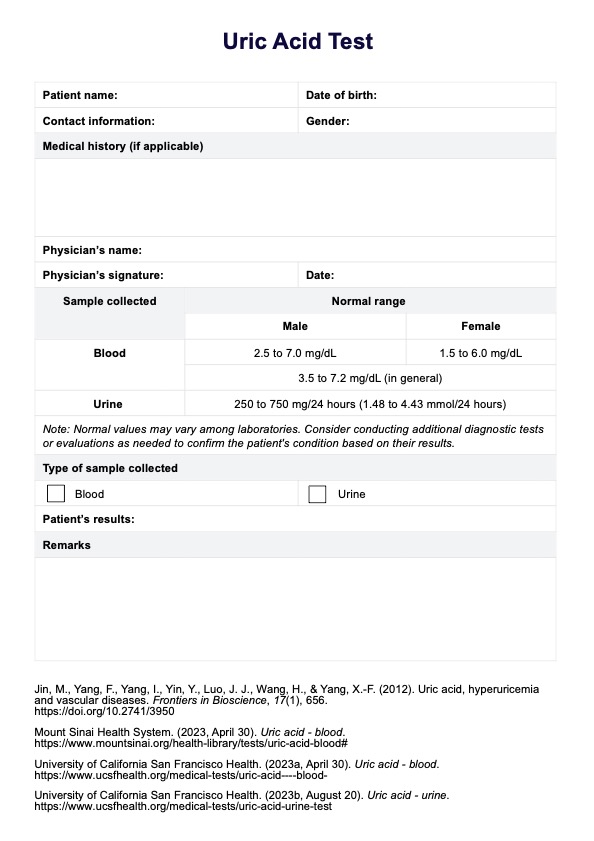
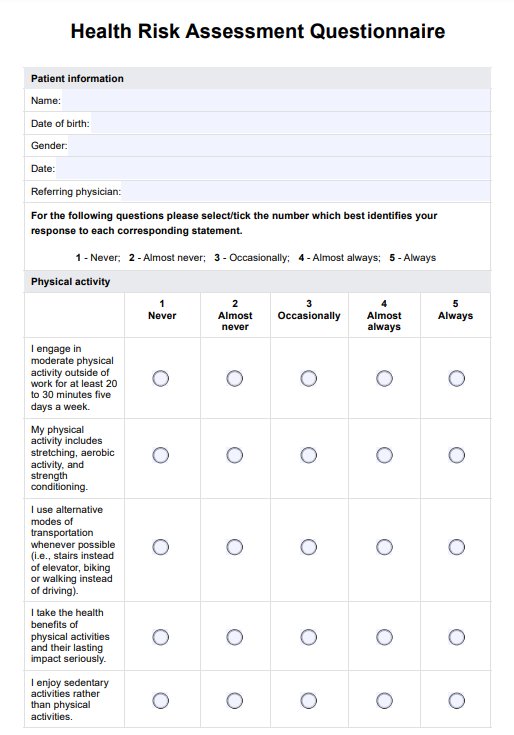
The Subjective section captures the patient’s personal experiences, including the client's chief complaint (CC), the history of present illness (HPI), and relevant medical, social, and family history. The Objective section documents measurable data like vital signs, physical exam findings, and other diagnostic data. Recognition and input from clinicians or other healthcare professionals may also be included. The Assessment synthesizes subjective and objective sections to form a diagnosis, including a prioritized problem list and differential diagnosis. The Plan outlines the steps for addressing the patient’s concerns, such as diagnostic testing, treatment, referrals, and education. This section ensures continuity of care and guides future treatment decisions.
Together, these components create a comprehensive view of the patient’s health. It’s perfect for mastering SOAP documentation and as a quick guide during busy workdays. With this chart, you can write accurate, professional notes efficiently every time.
Soap Chart Template
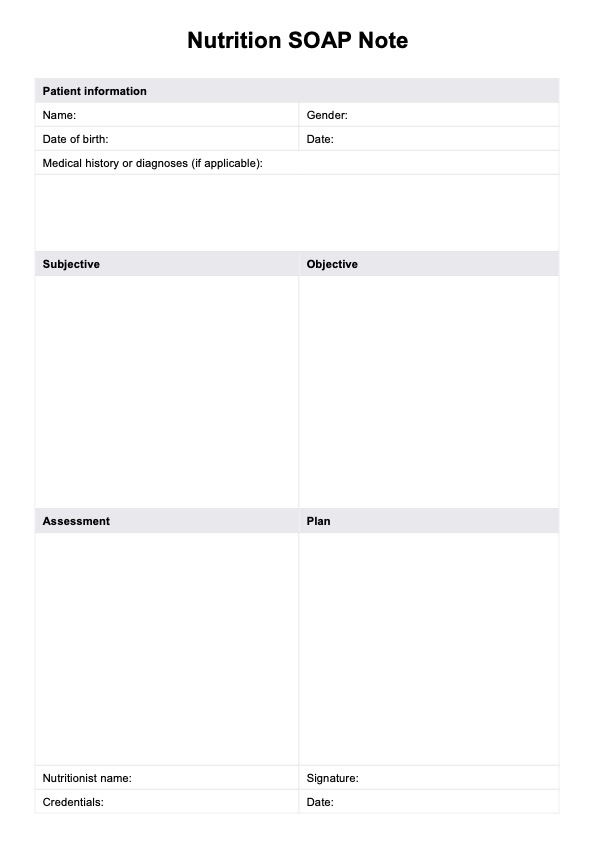
Soap Chart Example
How does it work?
Using the SOAP Chart, you’ll ensure all essential details are covered in your records during a patient encounter. Follow these easy steps to make the most of the reference tool.
Step 1: Open the chart
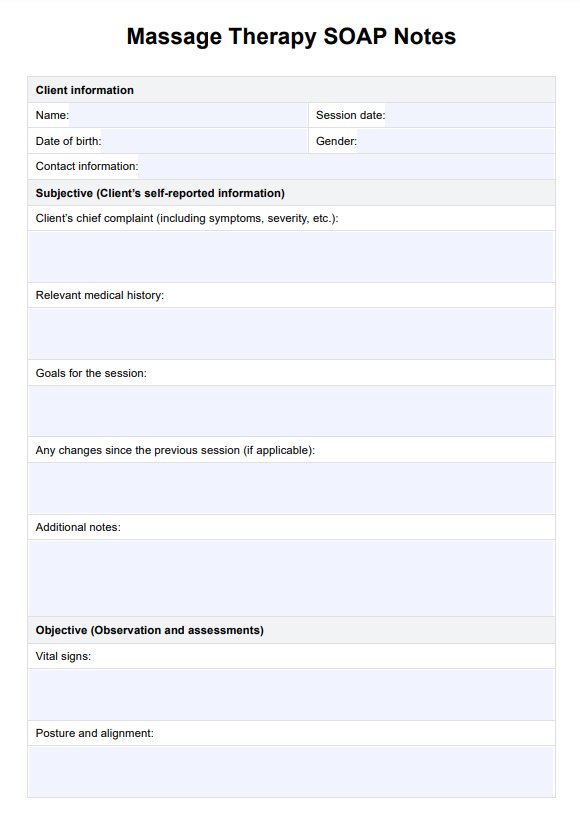
You can select "Use template" from this guide to access it directly through the Carepatron platform. In our templates library, you'll also find a range of SOAP templates for speech therapy, physical therapy, and social work, along with helpful SOAP note examples. If you'd prefer a PDF copy of this chart, simply click "Download."
Step 2: Use the reference alongside your SOAP note template
During SOAP note writing, refer to the chart. This can be used alongside a SOAP notes template to ensure you include all key details and maintain clear, organized records. Our chart is also ideal for reviewing or studying, ensuring you understand what to include in each section.
Step 3: Review your notes for completeness
After writing SOAP notes, review them for accuracy. This will help you ensure each section is thorough and clear, supporting organized and high-quality patient care.
When would you use this chart?
The SOAP Chart can be used in various situations. Here are some instances where it proves particularly helpful:
In healthcare documentation
Whether you’re a doctor, nurse, therapist, or other healthcare professional, the SOAP Chart ensures your documentation is thorough and well-organized. It provides a structure so you don’t miss critical details when documenting patient care.
In clinical teaching or training
For those learning or teaching SOAP notes, the reference chart serves as a practical guide. It helps new learners understand the structure and ensures all necessary information is included in their notes.
When reviewing patient records
The SOAP Chart is a useful reference when reviewing unorganized patient records. It helps you quickly identify the key sections and ensure nothing important is overlooked during assessments or follow-up care.
Benefits of using a SOAP Chart
The SOAP Chart offers several benefits that make patient documentation easier and more efficient. Here are three key advantages:
Easy to use
The SOAP Chart is simple to follow, making it convenient for healthcare providers like you to use. You can also display it in your office or clinic so that it will be easily visible.
Saves time
With the SOAP Chart, you don’t need to spend time remembering or looking up what should go into your notes. It is a quick reference, helping you document faster and more accurately.
Available in digital and printable formats
You can access the SOAP Chart in digital and printable formats, allowing you to choose what works best for you. Whether on the go or working at your desk, it's easy to use wherever needed.
Commonly asked questions
Mental health and medical history should be included in the Subjective section. This is where you document the patient's words about their past conditions and concerns.
Medications and allergies can be documented in either the Subjective or Objective sections. Be sure to include essential details for each medication, such as its name, dosage, route, and frequency.
SOAP stands for Subjective, Objective, Assessment, and Plan. It’s a format healthcare professionals use to document patient information, ensuring clear and organized notes.