Nutrition SOAP Note
Download our free Nutrition SOAP Notes template now to optimize your nutrition practice with structured documentation to improve patient care.


What is a Nutrition SOAP Note?
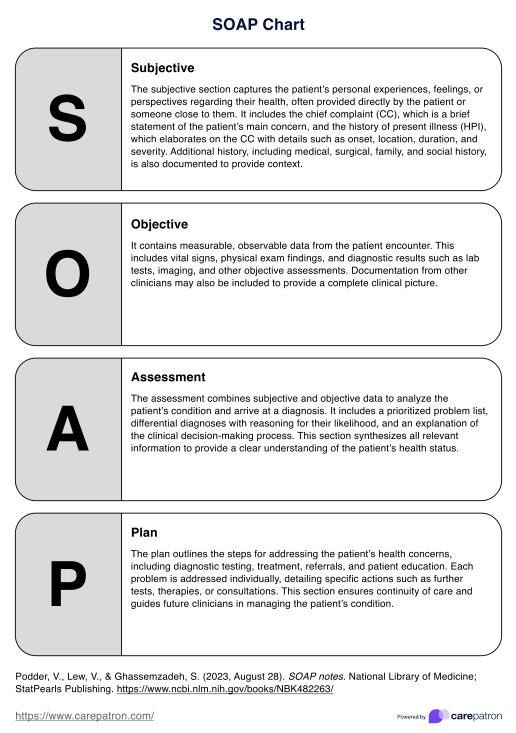
A Nutrition SOAP Note is a structured document used by healthcare professionals, particularly dietitians and nutritionists, to document patient encounters and assessments related to nutritional status, dietary habits, and medical nutrition therapy. This note follows the SOAP format for Subjective, Objective, Assessment, and Plan.
Here's how the SOAP note format applies to a Nutrition SOAP Note:
Subjective
This section includes information the patient or caregiver provides, such as chief complaint, medical history, present illness, current medications, dietary habits, food preferences, physical activity level, social history, and any subjective symptoms related to weight loss, nutrition, or nutritional concerns.
- Chief complaint: Reason for seeking nutrition counseling or intervention.
- Medical history: Any relevant medical conditions, surgeries, or chronic diseases affecting nutrition status.
- Present illness: Description of current symptoms or concerns related to nutrition.
- Dietary habits: Information about typical nutritional intake, meal patterns, preferences, and any recent changes in eating habits.
- Patient-reported symptoms: Subjective nutrition-related complaints, such as weight changes, appetite changes, digestive issues, or energy levels.
Objective
The healthcare provider records objective data obtained through measurements, observations, and assessments of criteria such as weight, height, body mass index (BMI), waist circumference, laboratory results, dietary intake, physical examination findings, and relevant medical test results.
- Anthropometric measurements: Height, weight, BMI, waist circumference, and other relevant measurements.
- Dietary intake: Detailed information about the patient's recent food and beverage consumption, including portion sizes and frequency of meals.
- Physical examination findings: Objective signs of malnutrition, such as muscle wasting, edema, or skin changes.
- Laboratory results: Relevant blood tests, such as lipid profile, fasting glucose, hemoglobin A1c, electrolytes, or micronutrient levels.
- Other objective data: Any additional assessments, such as dietary recalls, food diaries, or 24-hour urine collections.
Assessment
Healthcare providers analyze subjective and objective data to assess patients' nutritional status and related risk factors. Nutrition assessment identifies nutrition-related problems, evaluates various foods and their impact on health, and considers factors influencing dietary behaviors and readiness to change.
- Nutrition diagnosis: Identification of nutrition-related problems based on the subjective and objective data gathered. This may include malnutrition, obesity, inadequate nutrient intake, dyslipidemia, diabetes, hypertension, or other conditions.
- Risk factors: Factors contributing to the patient's nutrition-related problems, such as dietary behaviors, medical conditions, socioeconomic factors, or psychosocial issues.
- Interpretation of data: Analysis of the subjective and objective information to understand the patient's current nutritional status and its impact on health outcomes.
Plan
After the assessment, healthcare providers develop a personalized care plan that includes nutrition services, dietary adjustments, lifestyle changes, nutritional education, goal setting, discussing nutrition education topics, vital signs and nutrition monitoring, referrals, and follow-up visits. The aim is to address the primary nutrition concern and improve health outcomes.
- Medical nutrition therapy: Specific dietary recommendations, meal planning, nutrient goals, and dietary modifications tailored to the patient's nutrition diagnosis and goals.
- Interventions: Strategies for behavior change, giving educational materials on nutrition and healthy eating habits, counseling on portion control, meal timing, and food choices.
- Monitoring: Parameters to be monitored to evaluate progress include weight, body composition, blood pressure, blood glucose levels, lipid profiles, and dietary adherence.
- Follow-up: Plans for ongoing monitoring, follow-up appointments, referrals to other healthcare providers or specialists, and care coordination.
By following this SOAP note format, healthcare providers can effectively document nutritional assessments, disease diagnosis, interventions, and monitoring, ensuring comprehensive care and continuity of treatment for their patients. This documentation is crucial for evidence-based practice, interdisciplinary communication, and quality assurance in healthcare delivery.
For comprehensive management, developing a detailed health plan is crucial. Utilize our care plan template.
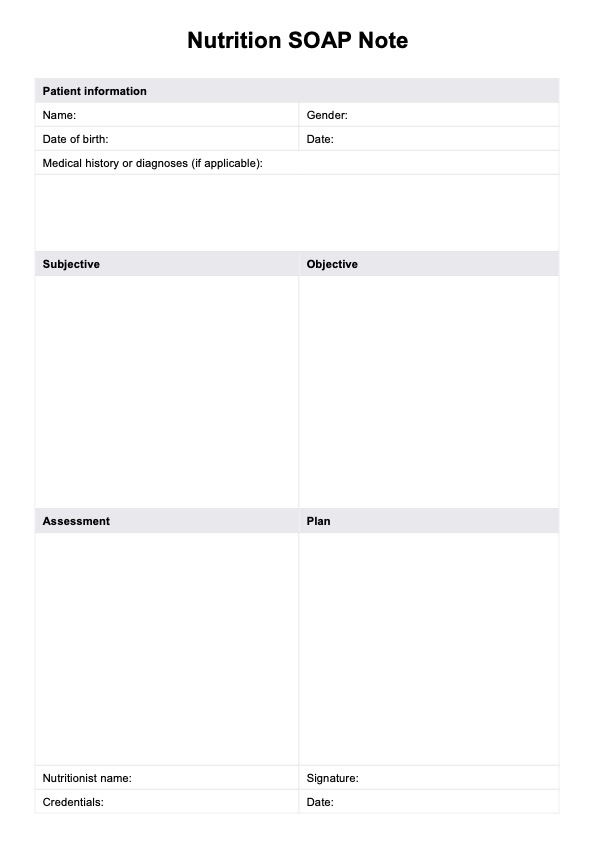
Nutrition SOAP Note Template
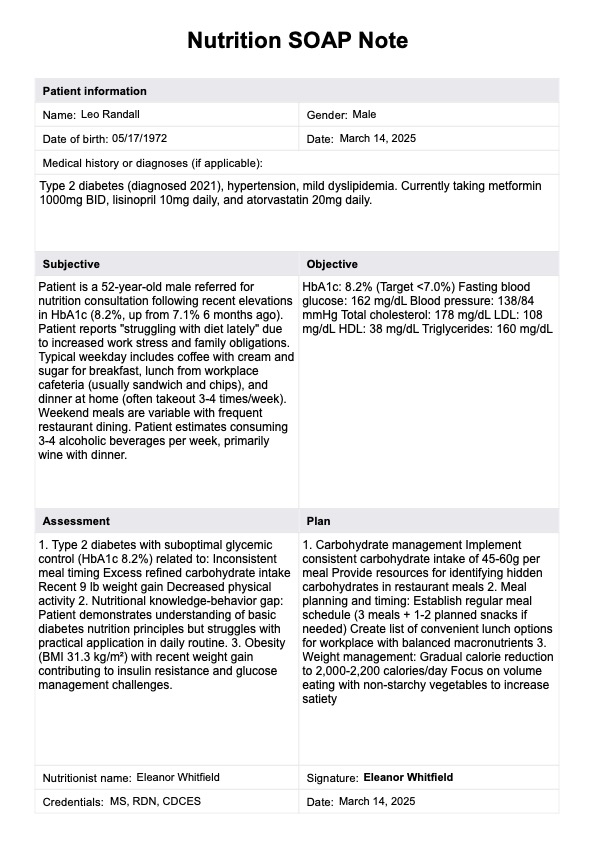
Nutrition SOAP Note Example
How do you use the Nutrition SOAP Notes template?
Using a Nutrition SOAP Notes template involves following a structured format to document patient encounters and assessments related to nutrition. Here's how you can use the template effectively:
Step 1: Access the template
Click "Download" to get a fillable PDF copy of the template, and click "Use template" to open and edit it within the Carepatron platform. You can print this out or use a digital copy.
Step 2: Fill out the SOAP template
Fill out each of the corresponding subjective and objective findings, assessment, and plan sections with the appropriate information for each.
Step 3: Save and store the template
After filling out the document by pen or digitally, you can store it in a secure physical location or within a HIPAA-compliant software for easier access.
Benefits of using a SOAP note for nutritional assessment
Using a SOAP note for the nutritional evaluation offers several benefits:
Structured documentation
The SOAP format provides a structured framework for documenting patient encounters, ensuring that all relevant aspects of the assessment are systematically recorded.
Comprehensive assessment
By including subjective, objective, assessment, and plan sections, SOAP notes facilitate a thorough evaluation of the patient's nutritional status, dietary habits, and medical nutrition therapy needs, including patient education. Utilize this SOAP notes template to support improving your practice and client results.
Interdisciplinary communication
SOAP notes enable effective communication between healthcare providers by providing a standardized format for conveying patient information, diagnoses, and treatment plans.
Continuity of care
With clear documentation of the patient's history, current status, and treatment plan, SOAP notes support continuity of care as multiple providers can easily understand the patient's needs and progress.
Commonly asked questions
A SOAP note in nutrition is a structured documentation format used by dietitians and nutritionists to record patient encounters, assessments, and treatment plans. It follows the SOAP framework: subjective (patient-reported information like dietary habits, symptoms, and medical history), objective (measurable data such as weight, lab results, and food intake records), assessment (analysis of nutritional issues or diagnoses), and plan (interventions, dietary recommendations, and follow-up plans).
An example of a Nutrition SOAP Note could include: Subjective: The patient reports poor appetite and a 4 kg weight loss over two months; Objective: The BMI is 18.5; lab results show low albumin levels. Assessment: The patient is at risk for malnutrition due to inadequate intake and weight loss. Plan: Recommend small, frequent meals with high-protein snacks; prescribe oral nutritional supplements; schedule follow-up in two weeks to monitor progress.
To document nutritional status effectively, gather subjective data (e.g., patient history, appetite, and food preferences) and objective data (e.g., weight, BMI, and lab results). Assess the findings to identify nutritional risks or deficiencies and create a plan with specific dietary adjustments or supplementation interventions. Ensure documentation is clear, systematic, and includes measurable outcomes to facilitate follow-up and interdisciplinary communication.