Massage Therapy Soap Notes
Efficiently manage client care with comprehensive Massage Therapy Soap Notes. Streamline records for enhanced massage sessions.


What is a Massage Therapy Soap Note?
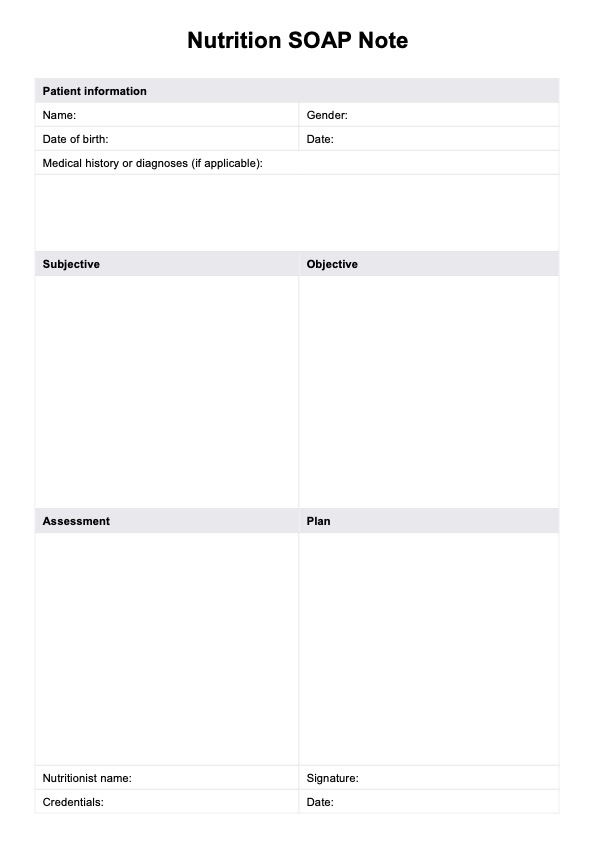
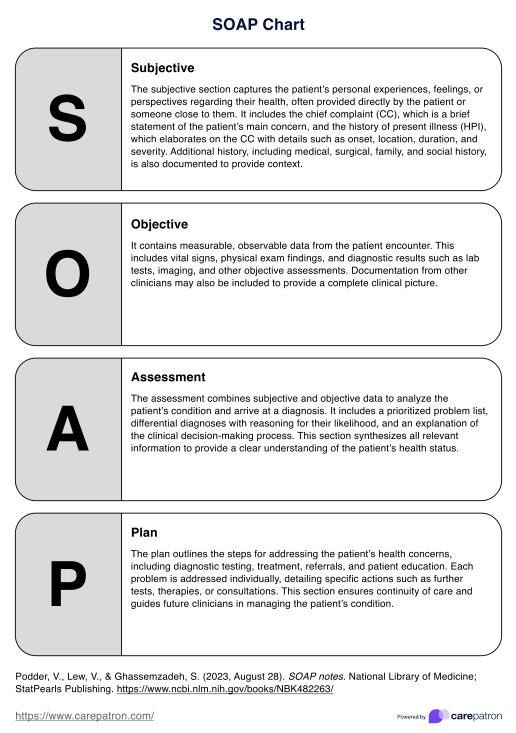
A SOAP note for massage therapy is a vital and structured documentation tool massage therapists use to effectively record and track their clients’ treatment progress. The acronym “SOAP” stands for Subjective, Objective, Assessment, and Plan, representing the note’s four critical components.
In the Subjective section, therapists document the client’s self-reported information, such as their presenting concerns, symptoms, and goals for the session. This provides valuable insights into the client’s perspective and helps the therapist tailor the treatment accordingly.
The Objective section comprises the therapist’s objective observations during the session. This includes the therapist’s assessment of the client’s physical condition, range of motion, muscle tension, and noteworthy findings. Objective data is crucial for tracking changes over time and evaluating the effectiveness of the treatment.
The Assessment component involves the therapist’s professional analysis of the client’s condition based on both subjective and objective information. It helps identify patterns, progress, and potential areas needing further attention.
The Plan section outlines the therapist’s proposed plan for future sessions. This may involve specific techniques, focus areas, and self-care recommendations between sessions. It ensures continuity of care and enables the massage therapist to collaborate effectively with the client.
Massage Therapy SOAP Notes offer several benefits. They enhance communication between therapists and clients, ensuring that treatment goals are aligned and progress is tracked. These SOAP notes also facilitate collaboration among healthcare professionals if the client receives care from multiple sources.
Moreover, effective SOAP Notes assist in maintaining accurate and organized records, which is essential for legal and ethical reasons. They provide a comprehensive history of the client’s sessions, which can be helpful in case of insurance claims, audits, or legal disputes.
In general, Therapy SOAP Notes serve as a comprehensive record-keeping system that helps therapists provide high-quality, individualized care to their clients. By capturing relevant information and facilitating informed decision-making, SOAP Notes contribute to the overall success of massage therapy treatments and promote clients’ well-being.
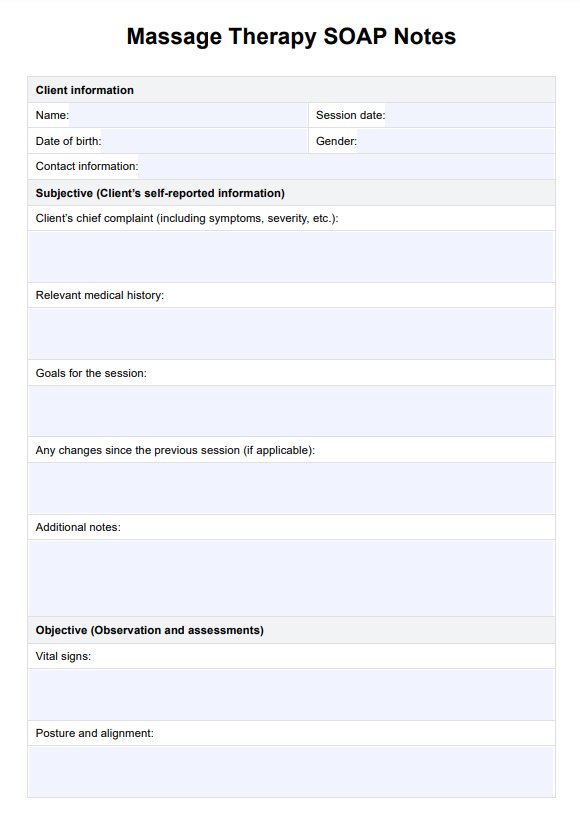
Massage Therapy Soap Notes Template
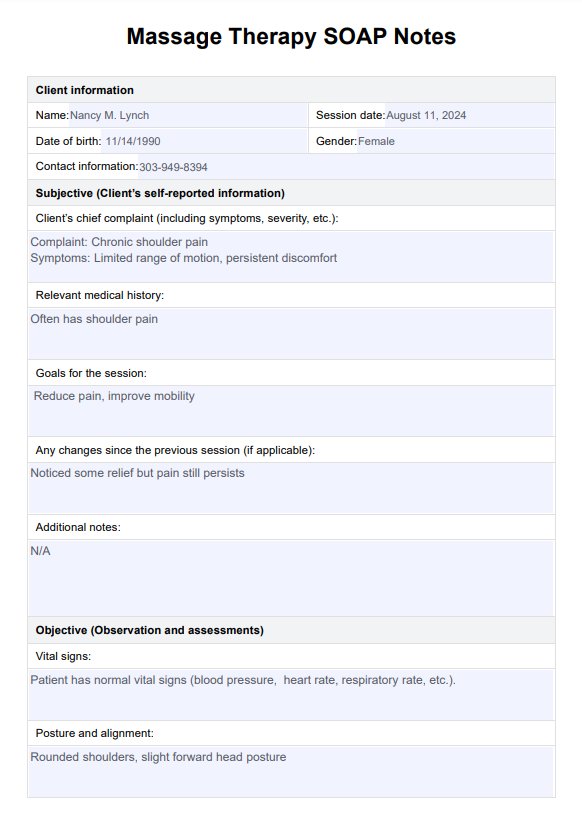
Massage Therapy Soap Notes Example
How does our Massage Therapy SOAP Notes work?
Massage Therapy SOAP Notes are structured forms that streamline the documentation process for massage therapists. These massage SOAP notes facilitate effective communication, continuity of care, and tracking of client progress. Here's how they work:
Step 1: Gather client information
The therapist collects essential details from their massage therapy clients, such as name, birth date, gender, and contact information, to ensure accurate record-keeping and easy identification.
Step 2: Record session details
The session date and the therapist's name are documented for reference and organization. This helps in tracking the timeline of treatments and the therapist responsible.
Step 3: Subjective information
Clients provide self-reported information about their chief complaints, presenting symptoms, and massage session goals. This insight helps therapists tailor treatments to the client's specific needs.
Step 4: Objective observations
During the session, the therapist objectively observes and records aspects like posture, muscle tension, range of motion, and other relevant physical findings. These observations provide a baseline for assessment.
Step 5: Professional assessment
The therapist analyzes the subjective and objective data to assess the client's progress, areas of improvement, and factors influencing their condition. This step guides future treatment planning.
Step 6: Creating a plan
Based on the assessment, the therapist proposes a trailored treatment plan for upcoming sessions. This includes detailing techniques, areas to focus on, self-care recommendations, and session frequency.
Step 7: Client feedback
Clients share their perceptions of the session, suggestions, concerns, and adherence to self-care recommendations. The client's response and feedback helps therapists adjust treatment plans and address any client needs.
Step 8: Signature and date
The client and therapist sign the note, indicating their agreement on the recorded information. The date serves as a reference point for when the note was completed.
When would you use this template?
Massage Therapy SOAP Notes are a versatile resource that is a fundamental tool for various healthcare practitioners involved in massage therapy or who have a massage therapy practice. Here are scenarios in which this resource proves invaluable:
Massage therapists
Massage therapists or massage therapy professionals use SOAP notes for documenting massage therapy sessions, tracking progress, and tailoring treatments. They record clients’ self-reported information, assess physical conditions, and plan future sessions based on individual needs.
Physical therapists
For physical therapists incorporating massage therapy, SOAP notes help monitor changes in muscle tension, range of motion, and pain levels. These notes contribute to holistic treatment plans and better communication with clients.
Chiropractors
Chiropractors can utilize SOAP notes to document massage therapy sessions as part of their patient care approach. This aids in evaluating the effectiveness of chiropractic adjustments and massages for spinal health.
Integrative healthcare providers
Healthcare practitioners offering integrative approaches benefit from SOAP notes to maintain a comprehensive overview of clients' treatments, combining massage therapy with other therapies for optimal wellness.
Sports rehabilitation specialists
In sports rehabilitation, SOAP notes track improvements in muscle recovery, flexibility, and injury healing through massage therapy. These notes guide tailored recovery plans for athletes.
Pain management specialists
SOAP Notes assist pain management specialists by documenting the impact of massage therapy on pain levels, helping to adjust treatments, and offering a multidisciplinary pain management approach.
Holistic practitioners
For holistic practitioners, SOAP notes support the holistic approach to healing, capturing physical and emotional responses to massage therapy and aligning with their comprehensive treatment strategies.
Wellness centers and spas
Wellness centers and spas use SOAP notes to maintain client records, offer consistent care, and customize experiences by referring to previous sessions' notes.
Benefits of using our Massage Therapy SOAP Notes template
Using these free SOAP Notes benefits therapists and clients by promoting effective treatment planning, informed decision-making, and ultimately improving client outcomes and satisfaction.
Efficient documentation
Free Massage Therapy SOAP Notes provide a structured framework for therapists to efficiently record client information, observations, assessments, and treatment plans, ensuring organized and comprehensive documentation. Writing SOAP notes clearly and concisely is crucial for efficient documentation, as it helps avoid common mistakes and enhances overall documentation skills.
Enhanced communication
These notes foster effective communication between therapists and clients by capturing goals, progress, and feedback. Clients can actively participate in their care plans, promoting a collaborative therapeutic relationship.
Progress tracking
Free SOAP Notes facilitate tracking client progress over multiple sessions, enabling therapists to adapt massage treatments based on documented changes in symptoms, range of motion, and pain levels. By recording subjective and objective information, therapists can offer more personalized and holistic care, considering physical aspects, emotional well-being, and goals.
Legal and ethical compliance
Free SOAP Notes ensure therapists adhere to legal and ethical standards by maintaining accurate and organized records, essential for potential insurance claims, audits, or legal inquiries.
Continuity of care
These notes enable seamless transitions between therapists or healthcare providers, ensuring consistent care delivery and a comprehensive understanding of the client's history.
Commonly asked questions
SOAP Notes are crucial for effective communication, continuity of care, and evidence-based decision-making. They help therapists tailor treatments, monitor progress, collaborate with other healthcare professionals, and maintain accurate legal and ethical compliance records.
Yes, SOAP Notes are widely used in various healthcare disciplines. While initially designed for medical fields, their adaptability makes them suitable for massage therapy, physical therapy, chiropractic care, and more.
Yes, software and apps like Carepatron are designed to streamline the process by providing more than SOAP notes for massage therapy SOAP notes and templates for digital soap notes. Carepatron has digital tools offer templates, customization, accessibility across devices, progress tracking, and secure data storage.





















-template.jpg)
















































































