Sepsis Nursing Care Plan
Use this in-depth guide on sepsis management and care plans to deliver unparalleled care for this life-threatening condition.


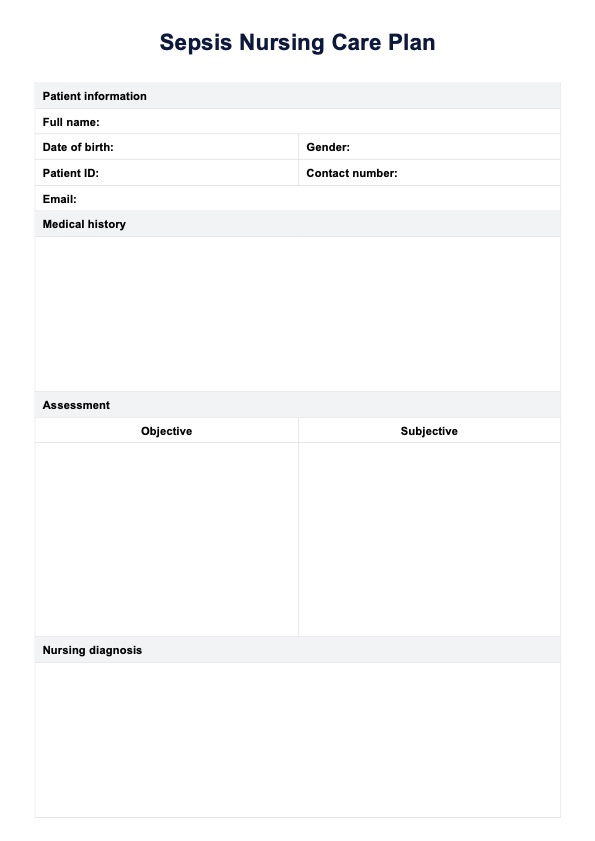
What is a Sepsis Nursing Care Plan Template?
A Sepsis Nursing Care Plan Template is a structured tool for healthcare professionals managing sepsis, severe sepsis, and septic shock patients. It incorporates evidence-based practices from sources like the Surviving Sepsis Campaign guidelines to address systemic inflammatory response syndrome and prevent organ failure. The template typically includes sections for assessing vital signs, implementing nursing interventions, and monitoring expected outcomes.
This comprehensive plan guides nurses in the early identification of sepsis, emphasizing critical assessments such as blood pressure, mean arterial pressure, and laboratory values, including complete blood count and lactic acid levels. It outlines key interventions like aggressive fluid resuscitation, administering broad-spectrum antibiotics, and maintaining adequate oxygenation. The template also addresses potential complications, such as acute respiratory distress syndrome and impaired gas exchange, while promoting infection control measures to support the body's immune system in combating the underlying infection.
Sepsis Nursing Care Plan Template
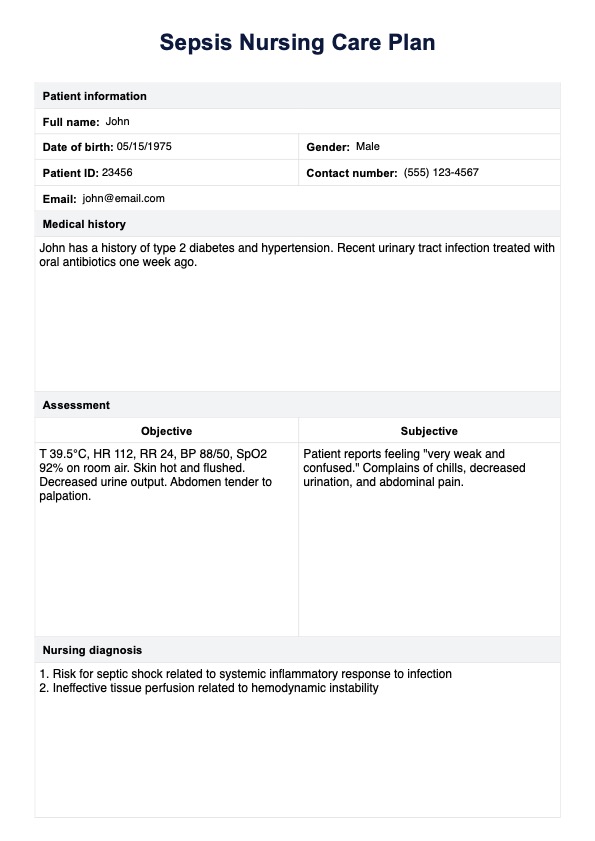
Sepsis Nursing Care Plan Example
How does it work?
A Sepsis Nursing Care Plan Template is a critical tool for managing patients with systemic inflammatory response syndrome, sepsis, and septic shock. It guides healthcare professionals, especially nurses, through a structured process to ensure comprehensive care and early identification of sepsis-related complications.
Step 1: Assessment
Conduct a thorough evaluation of the patient's vital signs, including blood pressure, respiratory rate, and body temperature. Monitor for clinical indicators of sepsis, such as altered mental status, rapid breathing, and signs of organ dysfunction. For the subjective assessment, collect a detailed patient history, including recent infections, surgeries, or any known risk factors for sepsis, such as immunosuppression or chronic diseases.
Step 2: Nursing diagnosis and goals
Formulate nursing diagnoses based on the assessment findings. Common diagnoses may include deficient fluid volume, decreased cardiac output, and risk for infection. These diagnoses help prioritize care and guide the selection of appropriate nursing interventions. Make sure to also include goals and expected outcomes for the care plan.
Step 3: Planning and interventions
Develop a care plan that addresses the identified nursing diagnoses. Key interventions may include aggressive fluid resuscitation, administering broad-spectrum antibiotics, maintaining adequate oxygenation, and implementing infection control measures. For each intervention, write a rationale explaining its possible impact.
Step 4: Evaluation
Continuously assess the patient's response to interventions and adjust the care plan as needed. Monitor for expected outcomes such as improved tissue perfusion, stabilized vital signs, and reduced signs of systemic inflammation. Regularly reassess clinical indicators and laboratory values to track progress and identify any developing complications.
When would you use this template?
A Sepsis Nursing Care Plan Template is a critical tool in clinical practice for managing patients with suspected or confirmed sepsis, severe sepsis, or septic shock. It is essential for guiding healthcare professionals through the complex process of early identification, assessment, and management of sepsis, ensuring adherence to evidence-based practices such as the Surviving Sepsis Campaign guidelines.
Early signs and symptoms
Use this template when patients present with early signs of systemic inflammatory response syndrome (SIRS) or sepsis. These may include elevated body temperature, rapid breathing, altered mental status, or changes in vital signs such as increased heart and respiratory rates. Early identification is crucial for initiating timely interventions and preventing progression to severe sepsis or septic shock.
Confirmed sepsis diagnosis
Implement the care plan when sepsis is diagnosed based on clinical indicators and laboratory values. This includes abnormal white blood cell count, elevated C-reactive protein, positive blood cultures, or signs of organ dysfunction. The template guides critical care nursing interventions for managing sepsis-induced complications such as impaired gas exchange, deficient fluid volume, and decreased cardiac output.
Monitoring and management
Utilize the template for ongoing monitoring of critically ill patients with sepsis. It helps track vital signs, mean arterial pressure, central venous pressure, and urine output. The plan also guides interventions like aggressive fluid resuscitation, administering broad-spectrum antibiotics, and maintaining adequate oxygenation to prevent organ failure and manage septic shock.
Complications and advanced care
Apply the template when managing sepsis-related complications such as acute respiratory distress syndrome, disseminated intravascular coagulation, or lactic acidosis. It provides a framework for advanced interventions, including mechanical ventilation, red blood cell transfusion, and severe sepsis and septic shock management in critical care medicine settings.
Patient education and discharge planning
Use the template to guide patient and family education about sepsis, infection control measures, and early signs of developing sepsis. It also aids in planning for discharge and follow-up care, addressing potential risk factors for recurrence, and emphasizing the importance of supporting the body's immune system in preventing future infections.
Commonly asked questions
Nurses should watch for signs of infection, altered mental status, rapid breathing, low blood pressure, decreased cardiac output, and elevated heart rate. Other critical indicators include abnormal body temperature, reduced urine output, and signs of organ dysfunction. Early recognition of these symptoms is crucial for timely intervention and preventing progression to severe sepsis or septic shock.
Adequate fluid resuscitation is critical in sepsis management. It helps maintain blood pressure, improve cardiac output, and enhance tissue perfusion. It also supports the body's immune system response to infection and helps prevent organ failure. Nurses should closely monitor fluid balance, urine output, and hemodynamic parameters to ensure adequate fluid management in patients developing sepsis.
Blood cultures are essential for identifying the causative organism in sepsis and guiding appropriate antibiotic therapy. They help confirm the diagnosis of sepsis and inform the nursing diagnosis process. Positive blood cultures can influence nursing interventions, such as implementing specific infection control measures and administering targeted antimicrobial therapy, which are crucial components of sepsis and septic shock management.