Post-Op Nursing Assessment
Optimize recovery through this efficient post-operative nursing assessment for comprehensive patient care and better health outcomes.


What is a Post-Op Nursing Assessment?
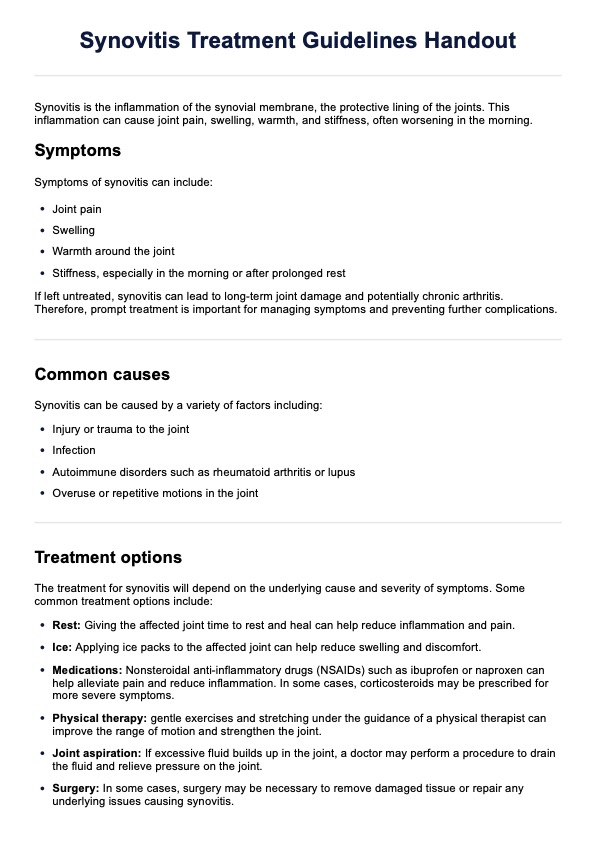
A post-operative assessment is a comprehensive evaluation of a patient's condition and recovery progress following surgery. The primary goals of this postoperative phase assessment are to identify potential complications, monitor the patient's response to treatment, and implement appropriate interventions to promote healing and prevent adverse outcomes.
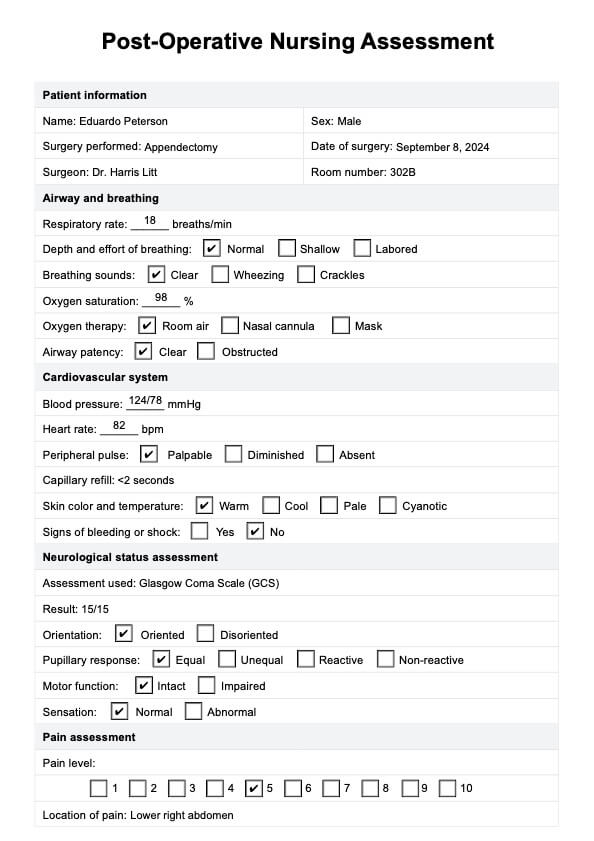
Initially, the assessment focuses on airway and breathing, where the nurse monitors the respiratory rate, depth, and effort, assesses breath sounds, and checks oxygen saturation to ensure adequate ventilation and oxygenation. Next, the cardiovascular system is evaluated by monitoring vital signs, particularly blood pressure and heart rate, while also assessing peripheral pulses, skin color, temperature, and capillary refill to detect any signs of bleeding or shock.
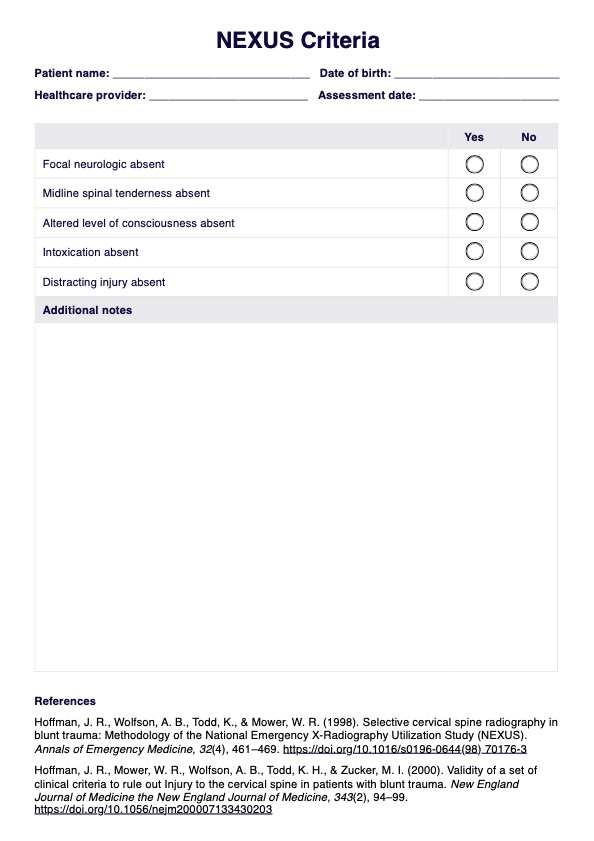
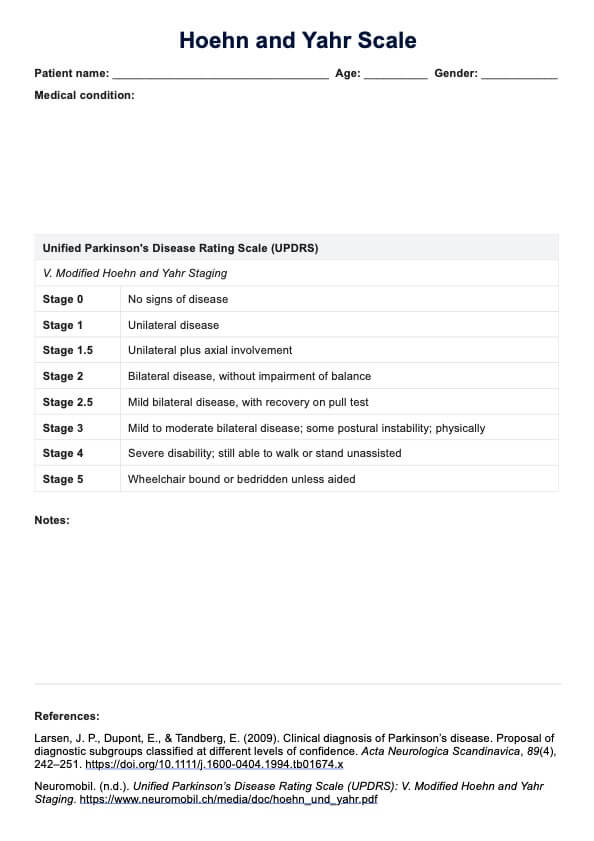
The neurological assessment involves evaluating the patient's level of consciousness and neurologic status using tools like the AVPU scale or the Glasgow Coma Scale, along with assessing pupillary response, motor function, and sensation to monitor for any neurological complications. Pain assessment is also crucial during the immediate postoperative phase, where the nurse evaluates the patient's pain intensity using a standardized pain scale, assesses the effectiveness of pain management interventions, and adjusts medications as necessary to maintain comfort.
Wound assessment is another critical component of a post-operative assessment checklist, where the nurse inspects the incision site for signs of infection, bleeding, or dehiscence, monitors drainage, and ensures that dressings are intact while providing appropriate postoperative care. Additionally, monitoring fluid and electrolyte balance is essential; this includes tracking intake and output, assessing for signs of fluid overload or deficit, and monitoring electrolyte levels to provide replacements as needed.
The assessment also considers the patient's activity and mobility, evaluating their ability to perform self-care activities and assisting with early mobilization to prevent complications. Providing assistive devices as needed is also part of this evaluation. Lastly, a psychosocial assessment is conducted to evaluate the patient’s emotional state and coping mechanisms during the immediate postoperative period, offering emotional support and addressing any concerns while involving family members in the ongoing care process as appropriate.
Overall, the Post-Op Nursing Assessment an ongoing observation and postoperative phase process that continues throughout the patient's recovery, requiring frequent monitoring, documentation, and effective communication with the healthcare team to ensure optimal outcomes.
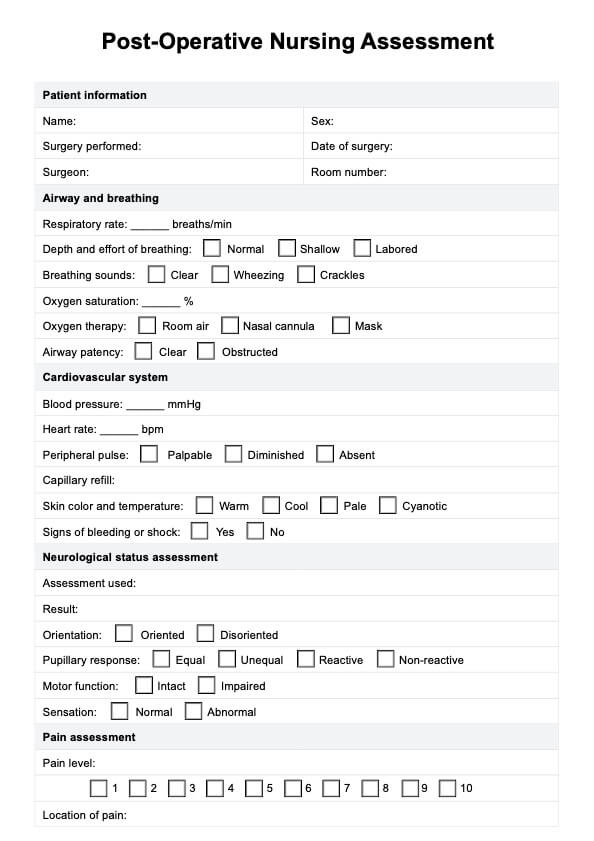
Post-Op Nursing Assessment Template
Post-Op Nursing Assessment Example
How does it work?
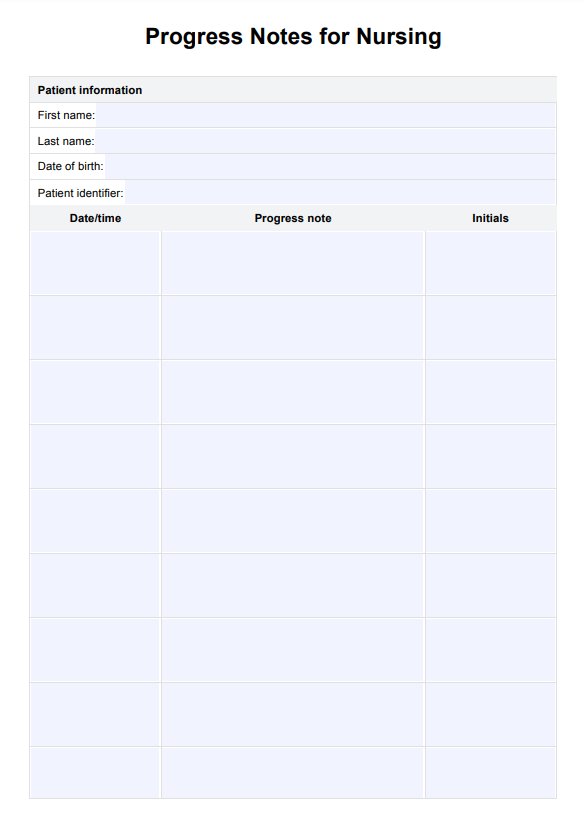
A Post-Op Nursing Assessment checklist serves as a structured tool to guide nurses in evaluating a patient's condition after surgery. This template is designed to ensure that all critical aspects of postoperative period care are systematically addressed, promoting patient safety and recovery. Here is how it works for medical professionals:
Step 1: Gather your resource
Post-nursing assessments are a valuable resource and essential to keep on hand. Make sure that you have a copy of the free printable PDF when the need arises by either clicking the “Download Template” or “Use Template” button or by searching “Post-Op Nursing Assessment” on Carepatron's template library's search bar on the website or app.
Step 2: Collate essential information
Once the patient has been operated on, utilizing the Post-Op Nursing Assessment template to ensure all goals of care are met is seamless and easily accessible to relevant parties via Carepatron's centralized workspace.
Step 3: Assess the patient
Begin the assessment by systematically evaluating the patient's readiness using the template. Each section prompts the nurse to document findings, ensuring no critical area is overlooked.
Step 4: Document findings
As you assess the patient, it's crucial to document all findings accurately in the template. This documentation serves multiple purposes: it provides a clear record of the patient's condition at the time of assessment or during the immediate postoperative period, facilitates communication among the healthcare team, and supports the development of an individualized care plan. Be sure to note any changes in the patient's status and any interventions that were implemented.
When would you use this template?
Following surgical procedures, a post-operative nursing assessment template is typically utilized in various healthcare settings. Here are some instances and scenarios where using a Post-Op Nursing Assessment template proves beneficial:
Standardized protocol
Hospitals and healthcare facilities often have standardized protocols or templates for post-operative assessments. These templates ensure that all necessary aspects of the assessment are covered uniformly for every patient, maintaining consistency in care and documentation.
Complex surgeries
After complex surgeries or procedures involving higher risks or specific recovery protocols, a standardized template ensures that nurses thoroughly evaluate various critical parameters related to the surgery, minimizing the chances of missing crucial details.
High patient volume
In busy healthcare environments where nurses handle multiple post-operative patients simultaneously, having a structured template streamlines the assessment process, enabling efficient and comprehensive evaluations within a limited time frame.
Post-Op Nursing Assessments and interventions
Post-Op Nursing Assessments and interventions are crucial elements in ensuring a patient's recovery from surgery. These assessments are multifaceted and involve various aspects of nursing care during the postoperative phase. Let's explore some key assessments and corresponding interventions along with their rationales:
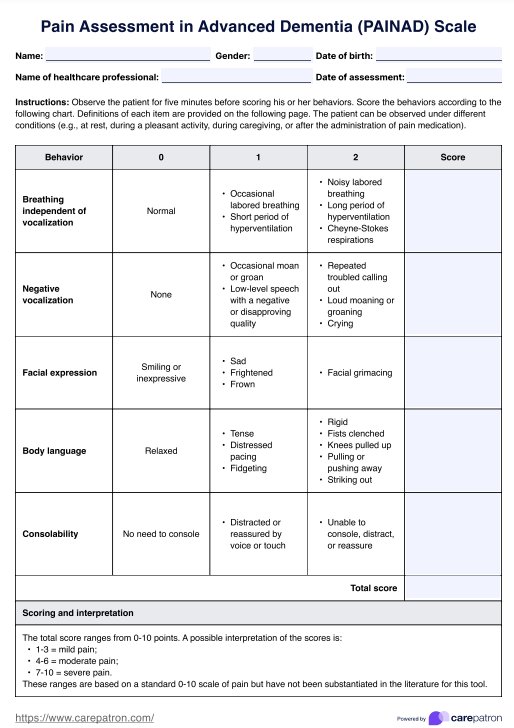
Vital signs monitoring
The template typically includes items for regular monitoring of vital signs such as blood pressure, heart rate, respiratory rate, temperature, and oxygen saturation. Abnormal readings can indicate other complications like bleeding or infection, prompting immediate intervention such as addressing any abnormalities by notifying the healthcare provider, administering medications as prescribed, and implementing supportive measures such as IV fluids or oxygen therapy to stabilize the patient's condition.
Surgical site assessment
Nurses use the template to inspect the surgical site for signs of inflammation, drainage, or other abnormalities. This helps detect potential infections or healing issues early, ensuring timely management. Interventions include promptly addressing any abnormalities by notifying the healthcare provider, administering medications as prescribed, and implementing supportive measures such as IV fluids or oxygen therapy to stabilize the patient's condition.
Fluid balance monitoring
Nurses assess fluid intake and output to evaluate hydration status and kidney function. The checklist helps track these metrics to prevent dehydration or fluid overload complications. Interventions include administering IV fluids as prescribed, encouraging oral fluid intake when appropriate, and monitoring urine output closely to ensure adequate kidney function.
Mobility and respiratory assessment
The Post-Op Nursing Assessment checklist prompts evaluation of the patient's ability to move and breathe effectively. Encouraging early ambulation and deep breathing exercises is essential to prevent respiratory complications, and the checklist ensures these activities are not overlooked. Interventions involve assisting the patient with ambulation as soon as they are stable, encouraging deep breathing and coughing exercises to promote lung expansion, and using incentive spirometry to enhance respiratory function.
Psychosocial patient assessment
Addressing the emotional and psychological well-being of the patient is included in the template. This ensures that nurses provide necessary support and address any concerns the patient may have during recovery. Interventions may include providing reassurance and emotional support, facilitating communication with family members, and referring the patient to counseling services if needed.
Commonly asked questions
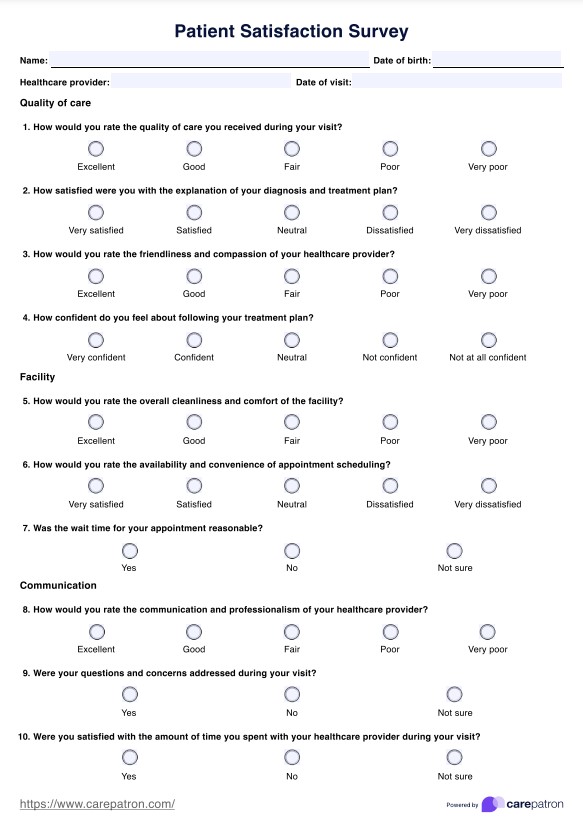
Monitoring vital signs post-surgery is crucial as it helps detect any early signs of complications. Changes in blood pressure, heart rate, respiratory rate, temperature, and oxygen saturation can indicate bleeding, shock, infections, or adverse reactions to anesthesia.
Signs of infection at a surgical site include redness, swelling, increased warmth, drainage (particularly if it's purulent or foul-smelling), and increased pain or tenderness. Regular surgical site assessment is critical to identify and address these signs promptly.
Adequate pain relief and management after a major surgery is vital for various reasons. It helps improve patient comfort, promotes early mobility, facilitates effective breathing, and aids overall recovery. Uncontrolled pain can hinder movement, increase the risk of complications such as blood clots or pneumonia, and delay the healing process of surgical patients.