Peripheral Vascular Examination
Explore our comprehensive Peripheral Vascular Examination guide for detailed assessment and documentation of vascular health, including key tests and findings.


What is a Peripheral Vascular Examination?
A Peripheral Vascular Examination is a thorough assessment of the function of the peripheral vascular system (blood vessels outside the heart and brain). This evaluation aims to detect signs of vascular disease pathology in the upper and lower extremities and determine the efficiency of blood circulation.
Peripheral vascular assessment is essential for identifying and monitoring patients at risk of or suffering from conditions such as peripheral arterial disease (PAD), chronic venous insufficiency, deep vein thrombosis (DVT), and complications of diabetes mellitus.
Early and systematic review of the patient's condition (including assessing for any abnormalities in the peripheral vascular system) facilitates timely intervention, preventing disease progression and improving overall health. Interventions may include such as lifestyle changes, medication, or vascular surgery, to restore blood flow and pressure to the affected areas.
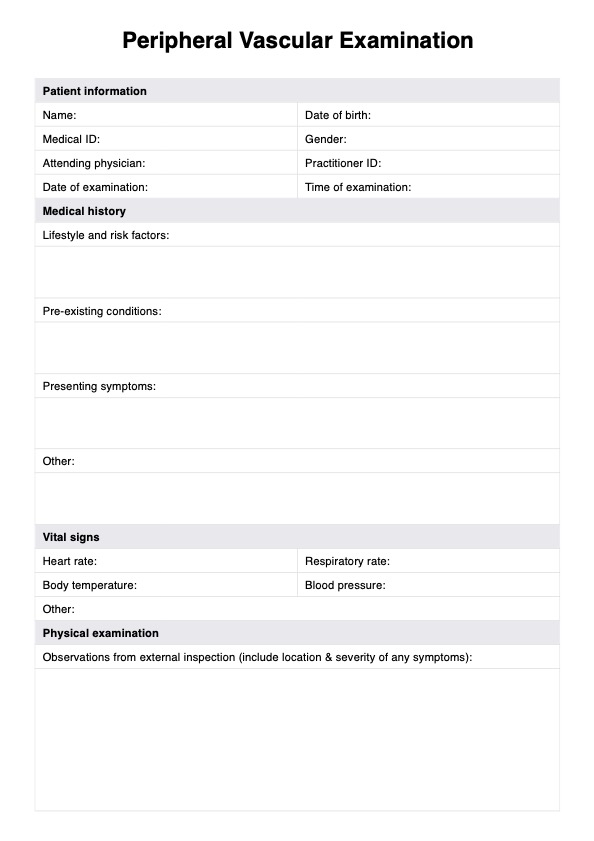
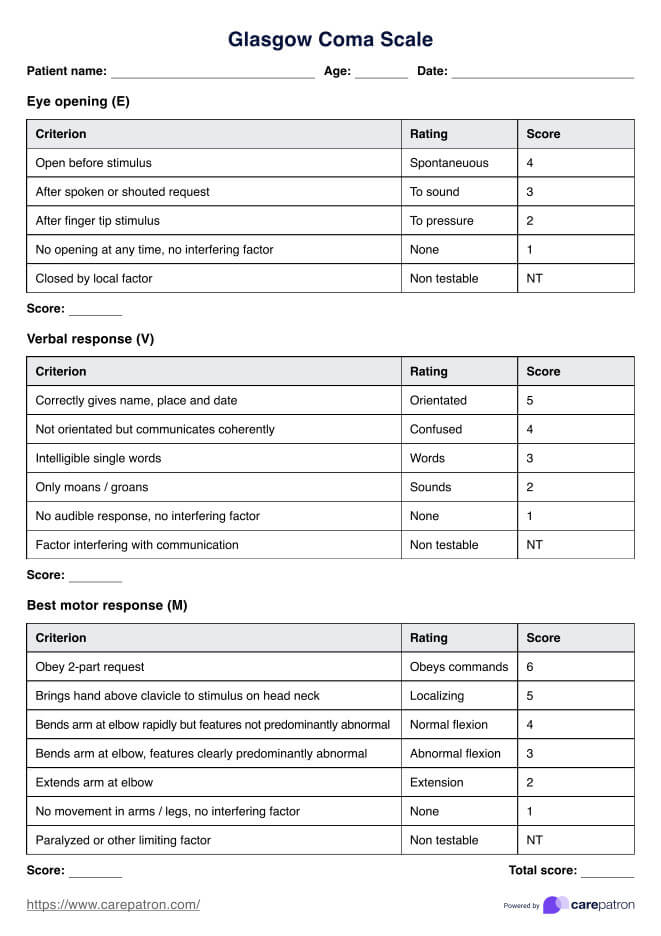
Peripheral Vascular Examination Template
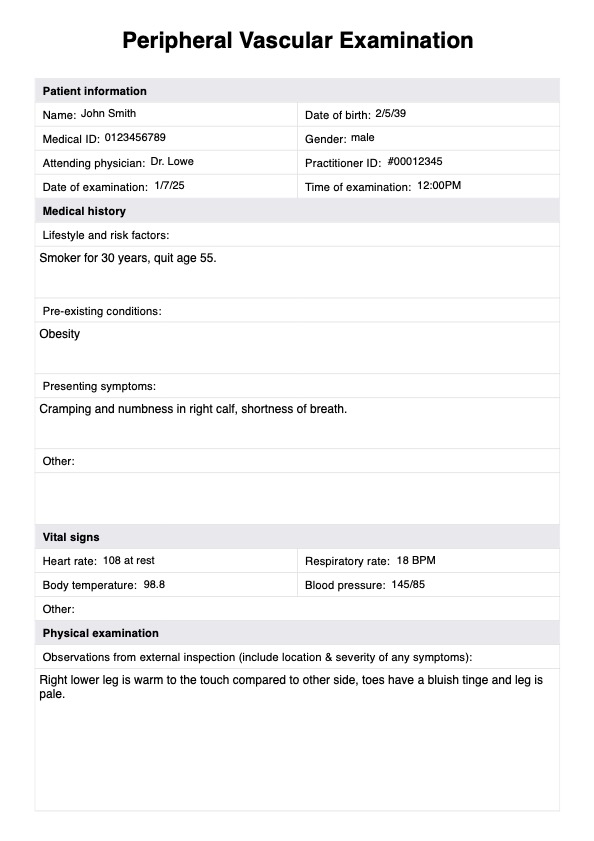
Peripheral Vascular Examination Example
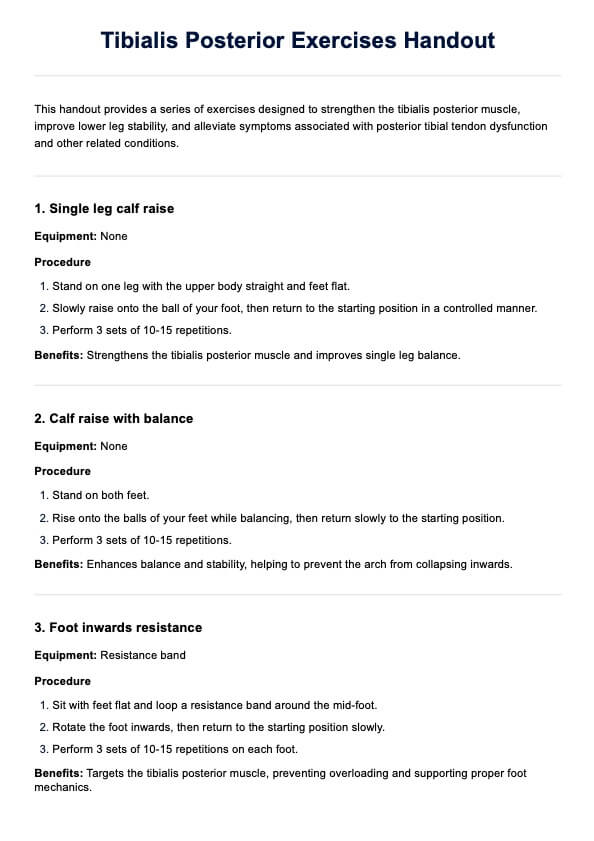
How to use the Peripheral Vascular Examination template
This template is a valuable guide to conducting a clinical evaluation of blood flow and blood pressure abnormalities. Follow these steps to properly assess signs of peripheral vascular disease or peripheral artery disease pathology:
Step 1: Access the template
Open the template by clicking the "Use template" button on this page, which opens the template in the Carepatron app. From there, you can customize the template before filling or printing it out.
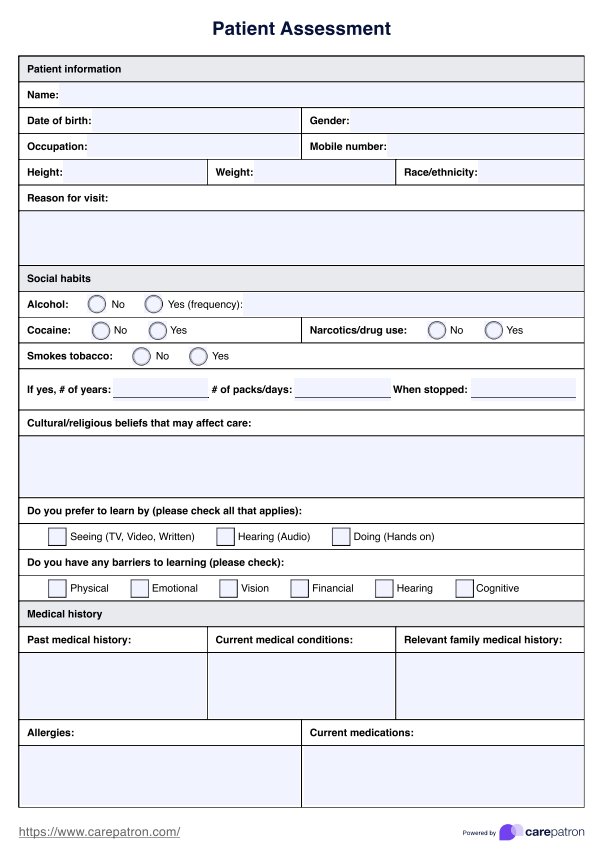
Step 2: Collect patient history
Input the patient's key demographic information at the top of the form. Collect relevant details around the patient's lifestyle, medical history, leg pain (which can indicate ischemia due to reduced blood flow), and any other symptoms. If the patient is diabetic, ask about their foot care and any history of foot ulcers.
Step 3: Vital signs and external examination
The initial stage of the physical assessment involves checking and recording the patient's vital signs. Examine the legs for signs of pitting edema, varicose veins, and venous ulcers that tend to appear on the medial aspect of the leg. If arterial ulcers are present (typically found on the foot or near the medial malleolus), record these also.
Step 4: Pulse examination
Next, palpate pulses in the legs (such as the radial pulse) and upper extremities to assess arterial flow. Absent pulses or diminished pulses may suggest artery disease or a blood clot. Also check and record capillary refill time.
Step 5: Blood pressure measurement
Perform the ankle brachial index (ABI) and record blood pressure readings of the arms and legs. A significant difference may indicate peripheral arterial pathology. In some cases it may also be appropriate to perform further tests such as the Doppler ultrasound to assess blood flow and blood pressure in the peripheral arteries. This identifies areas of reduced flow that might suggest the need for vascular surgery or stent placement. Record the results.
Step 6: Imaging tests
Detailed imaging of the arteries, including the renal arteries and the aorta, can identify specific areas of stenosis or blockages. If further imaging is performed, record the tests and their findings in the template.
Step 7: Diagnosis and treatment
Disclose the findings of the assessment (including any diagnoses, signs of disease progression, or identified risk factors) to the patient. If necessary, work with the patient to devise a treatment plan. This may include supervised exercise therapy, prescriptions, referrals, or advice on lifestyle changes to manage risk factors (such as smoking cessation, managing diabetes, and supervised exercise therapy).
Step 8: Monitoring and follow-up
Regular follow-up appointments are crucial for monitoring the disease's progression, evaluating the treatment plan's effectiveness, and making adjustments as needed. This may include repeat vascular testing and reassessment of cardiovascular risk factors.
What does our Peripheral Vascular Examination template contain?
Since a peripheral vascular assessment involves determining the presence, location, and severity of pathology and the risk of complications, our template contains fields for recording this information. These are all vital to form an appropriate treatment plan. Here's an overview of what results for each part of the examination may indicate:
Ankle-brachial index results:
- Normal: An ABI ratio of 1.0-1.4 indicates normal blood flow.
- Mild to moderate PAD: An ABI ratio of 0.7-0.99 suggests mild to moderate PAD.
- Severe PAD: An ABI ratio of less than 0.7 indicates severe PAD. This warrants further investigative measures. Potential interventions include stent placement or vascular surgery.
- Non-compressible arteries: An ABI ratio greater than 1.4 indicates non-compressible arteries, necessitating alternative imaging studies. This is common in diabetic patients.
Capillary refill test
Capillary refill time in the toes or fingers is measured to assess peripheral circulation. Delayed refill time indicates poor blood flow.
- Normal: A capillary refill time of less than two seconds is normal, indicating healthy blood flow.
- Delayed: A CRT greater than two seconds suggests compromised peripheral circulation, possibly due to PAD or arterial abnormalities.
Pulse examination
- Normal: Strong pulses at key sites (e.g., radial, brachial, femoral, popliteal, posterior tibial, and dorsalis pedis).
- Abnormal: Absent or weak pulses may indicate PAD, requiring further diagnostic evaluation.
Physical signs and symptoms
- Normal: Uniform blood flow, normal coloring, normal strength, and absence of significant plaques or blockages.
- Leg pain and claudication: Symptoms of pain, numbness or weakness that onset with activity and improve with rest are suggestive of PAD. The severity of PAD is often correlated with the distance a patient can walk without pain.
- Venous ulcers and skin changes: The presence of venous ulcers, varicose veins, and changes in skin color or texture on the legs indicate venous insufficiency or advanced PAD.
- Pitting edema: May indicate venous insufficiency or heart failure.
Doppler ultrasound and imaging tests:
- Normal: No blockages or narrowing of arteries, normal blood supply distribution and pressure to outer extremities.
- Abnormal: Presence of blockages or narrowing in the arteries, reduced blood flow, or signs of carotid stenosis or renal artery stenosis. These findings can necessitate interventions such as angioplasty, stent placement, or vascular surgery.
Commonly asked questions
Peripheral Vascular Disease (PVD) refers to disorders affecting blood vessels outside the heart and brain. It primarily involves narrowing peripheral arteries (most commonly in the legs) due to plaque buildup. This leads to reduced blood flow, causing symptoms such as leg pain, numbness, and, in severe cases, ulcers or gangrene.
The primary cause of PVD is atherosclerosis, where fatty deposits build up in the arterial walls and restrict blood flow. Other risk factors include smoking, diabetes, obesity, high blood pressure, high cholesterol, aging (especially over age 50), and a family history of vascular or heart diseases.
Symptoms vary depending on the part of the vascular system affected but typically are the result of reduced blood flow to the limbs. Edema (increased swelling), numbness, coldness, and weakness, claudication, and reduced peripheral pulses in the bilateral lower extremities are common. Other symptoms may include claudication, limb hair loss, erectile dysfunction, sores that won't heal, shiny skin, and change in skin color (paleness or cyanosis).
These affect different parts of the vascular system and thus typically have distinct symptoms. Symptoms of cardiovascular disease include breathing difficulty and chest pain. In some cases, an abdominal examination for cardiovascular disease may also be necessary, e.g., by assessing the maximum impulse palpable in the fifth intercostal space.