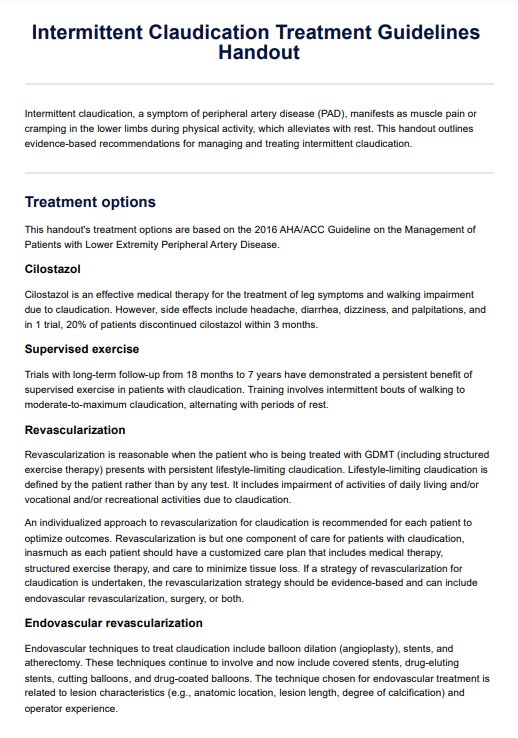
The treatment guidelines for intermittent claudication typically include lifestyle modifications such as supervised exercise programs, smoking cessation, and medication therapy to improve blood flow and manage symptoms. In severe cases, interventions like angioplasty or bypass surgery may be recommended.
Intermittent Claudication Treatment Guidelines Handout
Discover comprehensive Intermittent Claudication Treatment Guidelines Handout. Manage symptoms, improve blood flow, and reduce cardiovascular risks effectively.
Intermittent Claudication Treatment Guidelines Handout Template
Commonly asked questions
Intermittent claudication can be managed effectively by following treatment guidelines that emphasize lifestyle changes, medication adherence, and supervised exercise programs. These interventions aim to improve blood flow, alleviate symptoms, and reduce cardiovascular risks.
Medications commonly used to treat this condition include antiplatelet agents like aspirin, cilostazol to improve walking distance, and statins to manage cholesterol levels and reduce cardiovascular risks.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











