Creating a template outlines critical sections such as patient information, vital signs, medical history, and assessments. Customize it based on specific healthcare needs and considerations.
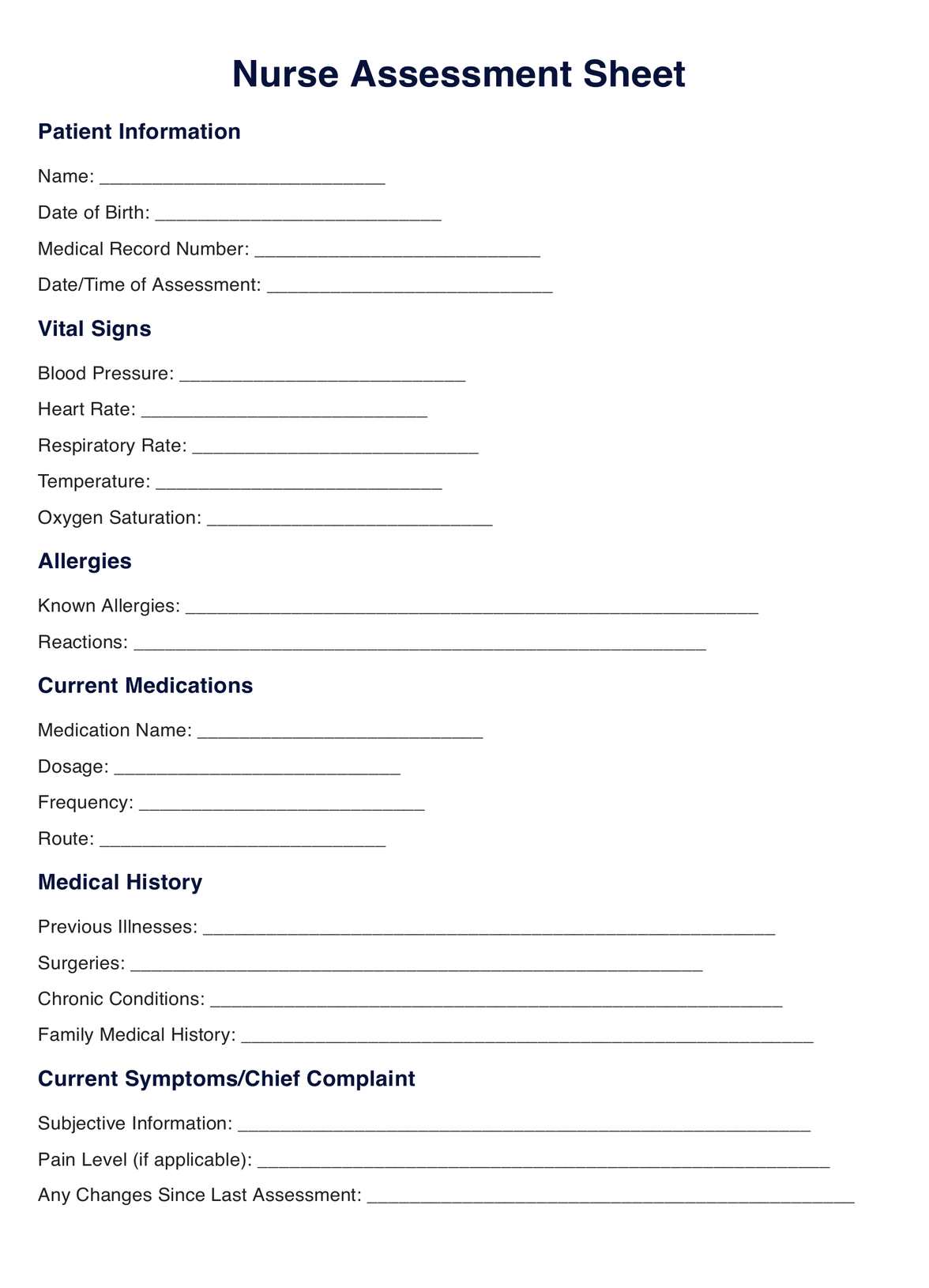
Nurse Assessment Sheet Template
Improve patient care with our Nurse Assessment Sheet Template. Simplify assessments, record vital signs, and improve healthcare documentation. Download now!
Use Template
Nurse Assessment Sheet Template Template
Commonly asked questions
Templates are used during patient encounters, admissions, routine check-ups, and follow-up visits to systematically gather and document essential patient information.
Healthcare professionals use templates to record vital signs, patient history, and observations. It is a structured guide for comprehensive patient assessments, promoting consistency and effective communication.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











