What is a Musculoskeletal Nursing Assessment?
A Musculoskeletal Nursing Assessment evaluates the function and structure of the musculoskeletal system through subjective and objective data collection. This routine physical exam involves gathering patient history and conducting a physical examination to identify normal or abnormal findings related to the bones, muscles, and joints (Chippewa Valley Technical College, 2023).
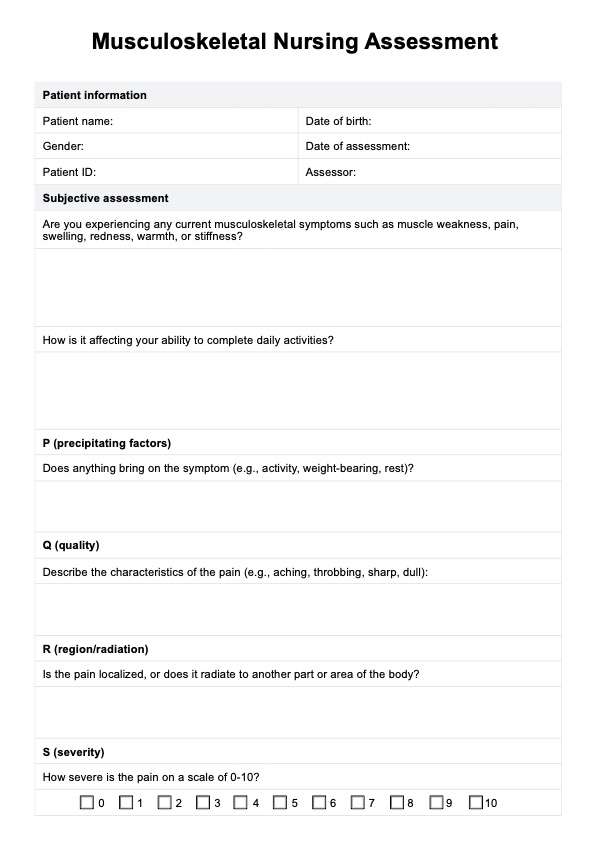
The subjective assessment collects subjective data about symptoms such as pain, swelling, stiffness, or muscle weakness, often using the PQRSTU method to guide the inquiry. Medical professionals ask the patient about injuries, chronic conditions, and mobility concerns and are also considered.
The physical examination involves inspecting two patient identifiers, the upper and lower extremities, for symmetry, deformities, and inflammation. Nurses can assess a range of motion and joint mobility while palpation checks for tenderness, warmth, or crepitus. Nurses also evaluate muscle strength through handgrip or resistance tests to assess upper extremity strength. Lower extremity strength is similarly tested through guided movements. The findings are documented as part of the musculoskeletal assessment documentation.
The musculoskeletal assessment identifies functional impairments or abnormalities, enabling targeted interventions. Conditions like muscle weakness or limited ROM can highlight acute injuries or chronic diseases, guiding further diagnostic or therapeutic actions.