House Brackmann Scale
Learn how to use the House-Brackmann Scale for facial paralysis assessment. Download the free template now.


What is facial paralysis?
Facial paralysis is a condition that causes the loss of facial muscle function. It usually affects one side of the face but can affect both sides in rare cases. The most noticeable symptom is the inability to control facial expressions like smiling or blinking.
Causes of facial paralysis
Facial nerve paralysis can have several causes, including:
- Bell's palsy: This is the most common cause of facial paralysis, characterized by sudden, temporary weakness or paralysis. Its exact cause is unknown but may be related to viral infections.
- Stroke: A stroke can interrupt the blood supply to the part of the brain that controls facial muscles, leading to paralysis.
- Lyme disease: This bacterial infection, transmitted by ticks, can cause neurological problems, including facial paralysis.
- Tumors: Benign or malignant tumors can compress and damage the facial nerves.
- Infections: Certain viral infections like herpes simplex and herpes zoster (shingles) can affect the facial nerves.
- Neurological disorders: Conditions like multiple sclerosis or Guillain-Barré syndrome can also cause facial paralysis.
How to diagnose facial paralysis
To diagnose facial paralysis, doctors evaluate a patient's medical history, perform a physical examination, and use diagnostic tests to understand the extent of nerve involvement and identify the underlying cause.
Before diagnosing a patient, a healthcare provider reviews their medical history, asking about current symptoms, accompanying symptoms, and recent illnesses or injuries. During the physical examination, the doctor assesses facial muscle function by having the patient perform simple movements such as closing their eyes, smiling, and raising their eyebrows.
Diagnostic tests can also help determine the cause and severity of facial paralysis, assisting in diagnosis and treatment. Imaging tests such as magnetic resonance imaging (MRI) and computed tomography (CT) scans can reveal structural causes like tumors or brain abnormalities. Electromyography (EMG) measures the electrical activity of muscles to assess nerve damage. Blood tests can identify infections, inflammatory conditions, or other underlying health issues. At the same time, a Lyme titer is a specific blood test used to detect Lyme disease if it is considered a potential cause.
Depending on the findings, further specialized tests might be recommended to explore other potential causes or to plan treatment.
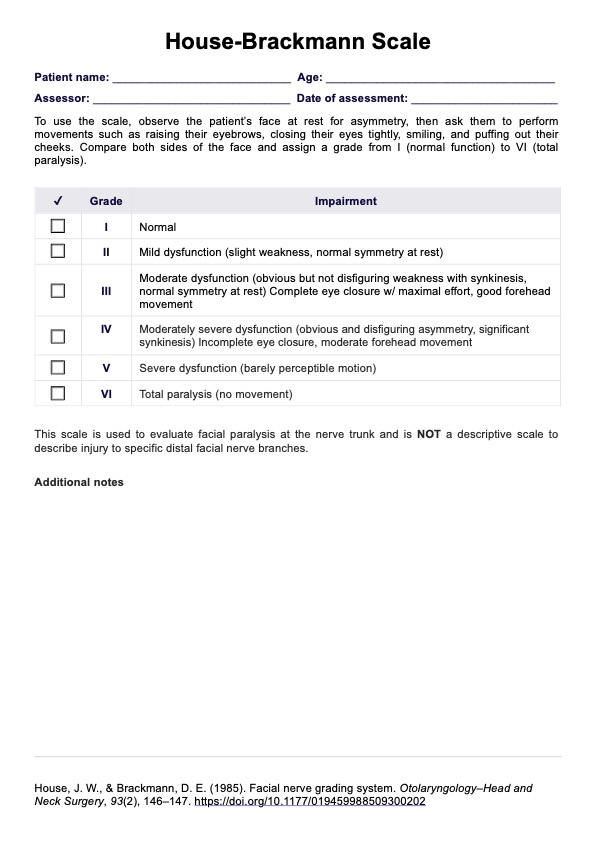
House Brackmann Scale Template
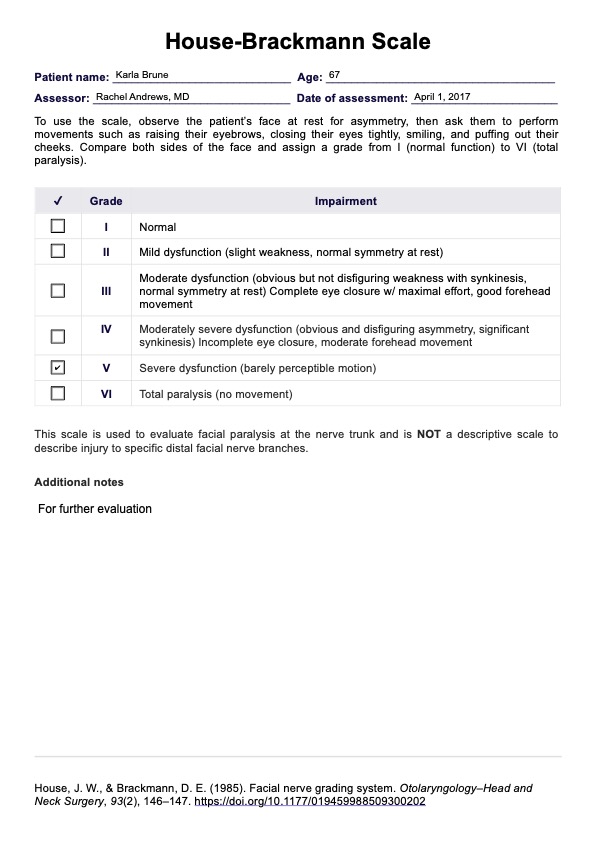
House Brackmann Scale Example
What is the House-Brackmann Scale?
The House-Brackmann grading system is a widely used clinical tool for evaluating the severity of facial palsy by assessing voluntary movement and facial symmetry. Initially developed by House and Brackmann in 1985, it remains one of the most accurate facial grading systems for diagnosing and monitoring facial nerve palsy, particularly in cases related to facial nerve surgery, trauma, and Bell’s palsy.
The House-Brackmann facial paralysis scale consists of six grades, ranging from normal function to total paralysis (House & Brackmann, 1985):
- Grade I represents normal facial function with full tone and motion, no weakness, and complete symmetry at rest and during movement.
- Grade II indicates mild dysfunction, where weakness is noticeable only upon close inspection. Facial symmetry is maintained at rest, and gross motion remains intact. The patient can fully close their eye with minimal effort.
- Grade III corresponds to moderate dysfunction, where asymmetry is more apparent during movement but not significantly disfiguring. The patient can close their eye with effort, though there is some noticeable weakness.
- Grade IV is classified as moderately severe dysfunction, with pronounced facial asymmetry even at rest. The patient has barely perceptible motion in affected areas, incomplete eye closure, and weak mouth movement. Forehead motion is absent.
- Grade V represents severe dysfunction, with minimal voluntary movement. The asymmetry is pronounced even without motion, and the patient cannot fully close their eye.
- Grade VI indicates total paralysis, with no tone, motion, or voluntary movement in any facial region.
The House-Brackmann score is critical in clinical practice for evaluating recovery and determining appropriate treatment strategies. While mild facial nerve palsy (Grades I and II) often resolves spontaneously, moderate to severe dysfunction (Grades III to VI) may require surgical intervention or rehabilitation. By providing a standardized measure, the House-Brackmann facial nerve grading system ensures consistency in diagnosing and treating facial nerve palsy.
How does our House-Brackmann Scale template work?
Our House-Brackmann Scale template is designed to evaluate and document facial nerve function in patients. Follow these steps to get started:
Step 1: Download the scale
You can get a copy of the scale by clicking the "Use template" button. This lets you open the template via the Carepatron app and edit it. To get a PDF copy, click "Download."
Step 2: Assess facial palsy
Use the template to evaluate facial palsy by observing the patient’s facial symmetry at rest and during voluntary movement. Carefully check for weakness, incomplete eye closure, and mouth movement deficits to ensure a precise assessment.
Step 3: Record and monitor
Use the template to accurately track facial palsy over time, ensuring consistency in assessment. Regular evaluations help measure recovery progress and guide appropriate treatment.
Step 4: Review and update regularly
Continuously update the patient’s facial palsy score in follow-up assessments. Tracking changes over time ensures their dysfunction is managed effectively and informs ongoing care strategies.
Next steps after using the House-Brackmann Scale
After evaluating facial nerve function with the House-Brackmann Scale, the next steps involve further diagnostic testing, treatment planning, patient education, and long-term monitoring to ensure comprehensive care.
Conduct further diagnostic testing
As mentioned, additional tests may be required to confirm the extent of facial nerve dysfunction and identify underlying causes. Nerve conduction studies and electromyography help assess nerve and muscle function, providing insight into the severity of the damage. MRI or CT scans may also be necessary to detect structural abnormalities such as tumors, inflammation, or fractures affecting the facial nerve.
Develop a personalized treatment plan
Once the severity of facial palsy has been established, a tailored treatment plan should be created based on the level of dysfunction. Physical therapy is crucial in restoring movement, with exercises designed to improve muscle control and prevent stiffness. Medications such as corticosteroids may be prescribed to reduce inflammation, while antiviral drugs can be considered if a viral infection is suspected. In some cases, botulinum toxin injections may help manage muscle spasms or synkinesis in patients with partial recovery.
Consider surgical intervention for severe dysfunction gross
In cases of severe gross dysfunction, where facial movement is minimal or absent (grades V or VI), surgical options may be necessary. Nerve grafts or transfers can restore function by reconnecting damaged nerves, while muscle transfers reposition healthy muscles to compensate for lost movement. Surgery should be carefully evaluated, with risks and benefits weighed before proceeding. Long-term rehabilitation following surgical intervention is essential to maximize functional improvement.
Educate patients about facial palsy accurate assessment and recovery
Providing patients with a clear understanding of their diagnosis and expected recovery timeline is crucial for effective management. Patients should be educated on the significance of their House-Brackmann score and how it influences treatment decisions. Those with incomplete eye closure need guidance on eye protection measures to prevent complications such as corneal damage. Facial exercises should be demonstrated to encourage active participation in rehabilitation.
Refer to specialists for comprehensive management
Patients with complex or progressive facial nerve dysfunction should be referred to specialists for further evaluation and management. Neurologists, otolaryngologists, and facial plastic surgeons can provide advanced treatment options, including specialized therapy and surgical interventions. Multidisciplinary collaboration enhances patient care and improves outcomes for those with severe facial palsy.
Schedule follow-up visits to monitor progress
Regular follow-up appointments are essential for tracking improvements and adjusting treatment plans. The House-Brackmann score should be reassessed at each visit to measure recovery progress accurately. If a patient is not showing expected improvement, treatment strategies may need to be modified.
Provide emotional and psychological support
Facial palsy can significantly impact a patient’s self-esteem and emotional well-being. Connecting patients with support groups or counseling services can help them navigate the psychological challenges associated with facial nerve dysfunction.
Reference
House, J. W., & Brackmann, D. E. (1985). Facial nerve grading system. Otolaryngol Head Neck Surg, 93(2), 146–147. https://doi.org/10.1177/019459988509300202
Commonly asked questions
The House-Brackmann Scale assesses the severity of facial nerve dysfunction, particularly in conditions such as facial palsy, Bell’s palsy, and post-surgical nerve recovery. It provides a standardized grading system from Grade I (normal function) to Grade VI (total paralysis) to evaluate facial movement, symmetry, and voluntary muscle control. This scale helps clinicians monitor progress and determine appropriate treatment strategies.
The House-Brackmann grading system is the most widely used scale for evaluating Bell’s palsy, as it accurately assesses facial nerve paralysis. It categorizes the severity of facial dysfunction, allowing healthcare providers to track recovery and adjust treatment plans accordingly. Other facial grading systems exist, but the House-Brackmann Scale remains the clinical standard.
The House-Brackmann score for facial nerve weakness ranges from Grade II to Grade V, depending on the severity of movement impairment. Mild weakness (Grade II) includes slight asymmetry and near-normal function, while moderate to severe dysfunction (Grades III to V) involves increasing difficulty with voluntary movement and incomplete eye closure. Total paralysis (Grade VI) represents the most severe form, with no facial motion present.