GI bleeding can result from conditions like peptic ulcers, inflammatory bowel disease, or diverticulosis. The risk of bleeding increases with factors like blood-thinning medications or liver disease. Monitoring symptoms like bright red blood or tarry stools helps identify the source early.
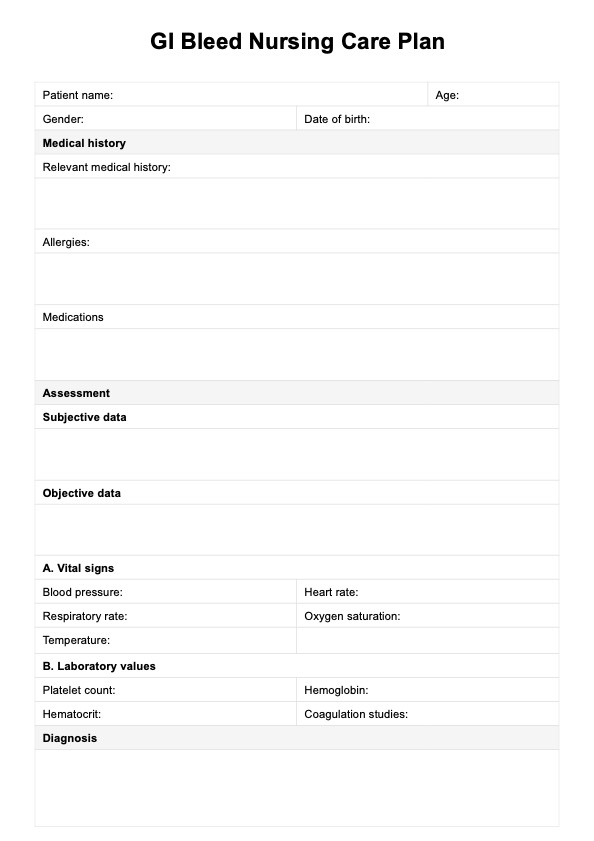
Gi Bleed Nursing Care Plan
Access a comprehensive GI Bleed Nursing Care Plan Template for effectively managing gastrointestinal bleeding. Download a PDF copy.
Gi Bleed Nursing Care Plan Template
Commonly asked questions
In cases of severe GI bleeding, blood transfusions, including the administration of packed red blood cells, may be necessary to replace lost blood and restore stable vital signs. This is critical when blood loss is significant, and the patient is at risk of shock or decreased blood volume.
It’s crucial to evaluate fluid balance and administer intravenous fluids to prevent dehydration and maintain fluid and electrolyte balance. This helps stabilize the patient and support their overall health, especially during active gastrointestinal bleeding.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











