A physical exam of the eyes involves a series of assessments to evaluate visual acuity, eye movement, pupil reactions, and the health of ocular structures. Eye care professionals follow a comprehensive process to ensure all crucial aspects of eye health and function are assessed.
Eye Physical Examination
An eye physical exam assesses vision and eye health and detects any abnormalities or diseases. Download Carepatron's free eye exam PDF here.
Eye Physical Examination Template
Commonly asked questions
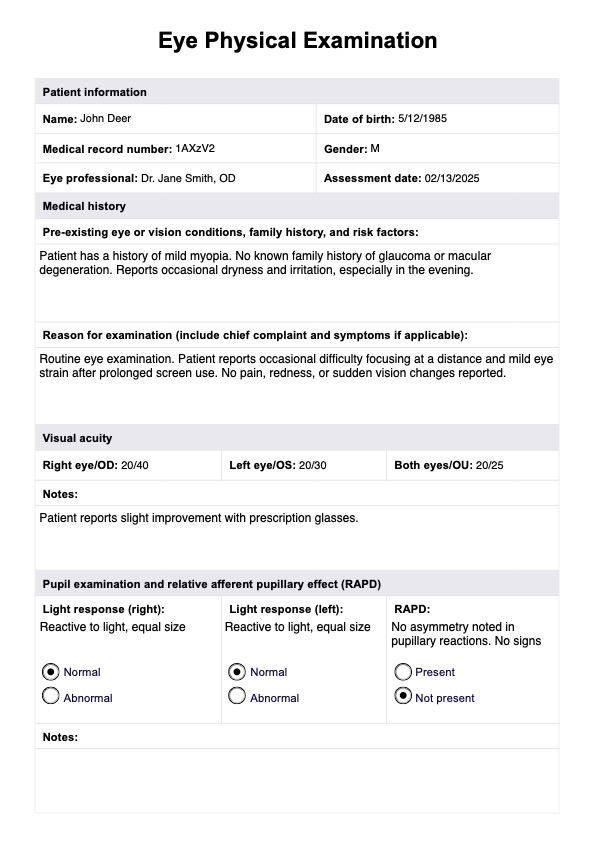
A routine eye exam typically includes visual acuity testing, pupil assessment, evaluation of extraocular movements and extraocular muscles, confrontation visual field testing, external examination, and various specialized tests based on individual needs. If the patient has a family history or particular risk factors for a particular eye condition, the examiner may perform additional testing.
The appropriate frequency of eye exams depends on the patient's individual health, family history and risk factors. Generally, patients should aim to present for eye testing approximately every 2 years, but more frequent exams are advisable if specific symptoms such as eye pain or vision loss occur.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











